On December 11, 2018, a Welsh charity, www.PAST.Wales arranged an awareness day to be held at the Senedd in Cardiff, home of the National Assembly for Wales. This presented an opportunity to discuss and debate issues of iatrogenesis, dependence, overprescription and prescribed harm within earshot of Welsh Assembly Members. The Assembly has devolved authority for health and can act independently of Westminster, so this was a chance to directly address policymakers. A relationship to the Assembly Members was provided by a petition to the Welsh Assembly raised by campaigner Stevie Lewis, which called for recognition and support for prescribed drug dependence across Wales.
Part 1 – The Presentations
Speakers were Dr David Healy, Stevie Lewis and myself and the event was arranged and hosted by Aled Jones. Aled, whilst working within recovery and substance misuse services, heard many speaking of the lack of understanding or support for withdrawal from medications. His own disastrous encounter with antidepressants and pain medication gave him the awareness of the issues that can arise from their use.
Dr David Healy speaking first, focussed on identifying the context and why pharmaceutical drugs such as antidepressants constitute a political problem. He explained the endemic nature of ghostwriting in clinical trials of psychiatric drugs and that these anonymous writers do not have access to the original trial data. This lack of access to the original data permeates the system such that neither peer reviewers, regulators or treating physicians can access the data they need to make decisions about safety or efficacy. He discussed the clinical trials of antidepressants including Prozac (a drug promoted as one that would make us ‘better than well’) noting that Prozac distinguishes itself as having more negative trial outcomes than any other antidepressant drug. Despite these negative outcomes, the ghostwritten trial reports mostly conclude that the drugs are effective and these are the reports that are used by regulators such as the FDA in the US and MHRA in the UK to licence the drugs for use. He also described how readily patient experiences are discounted and those that experience difficulty are labelled as ‘rotten apples’ when actually, the problem is better conceptualised as a ‘rotten barrel’ problem.
Speaking next was Stevie Lewis, a campaigner with lived experience of antidepressant dependence and withdrawal and someone who had endured a lengthy period of withdrawal and an extremely unpleasant and lengthy post-withdrawal syndrome. She discussed systematic work undertaken by herself and colleagues Dr Anne Guy and therapist Marion Brown, that identified key failure points in the prescribing of antidepressant drugs. These failure points encompass critical moments in the doctor/patient relationship where chances to provide informed consent or to address potential dependence issues are missed. Stevie also reminded attendees that 158 lived experience accounts had been shared through the Scottish and Welsh petitions. She related that two of the people who had submitted accounts for the Scottish petition had recently taken their own lives, unable to endure the physical and emotional toll that withdrawal had taken on them and the disruption to their lives.
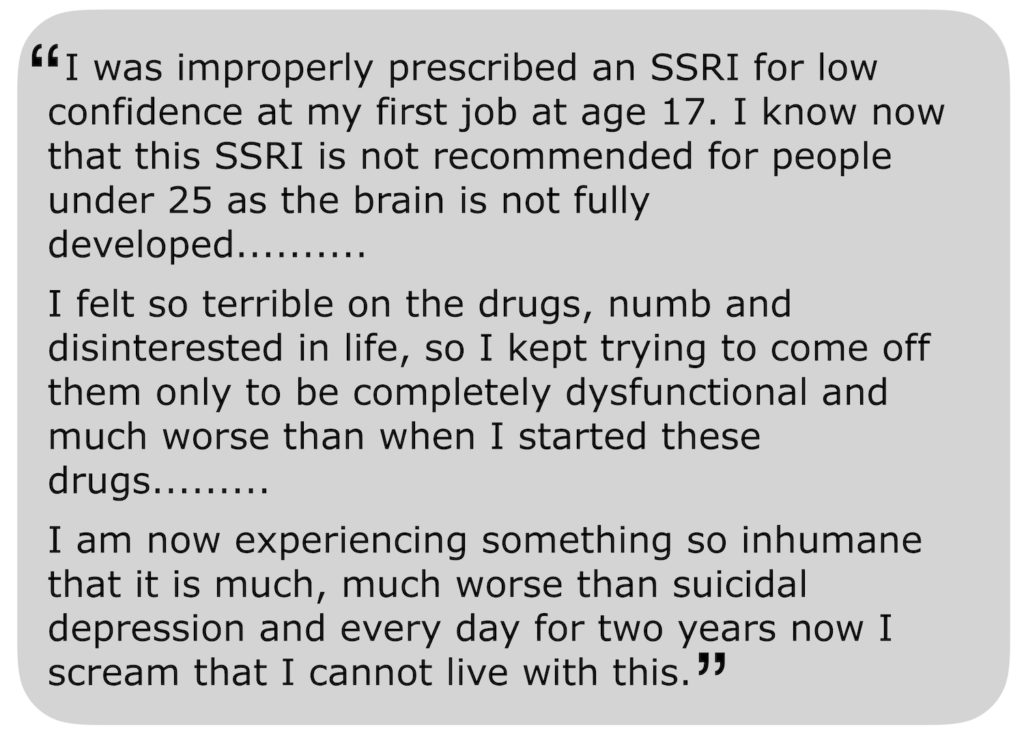
The first, 28-year-old Katalin Balint from Hungary, wrote the following in her submission to the Scottish petition. She took her life on October 1, 2018:
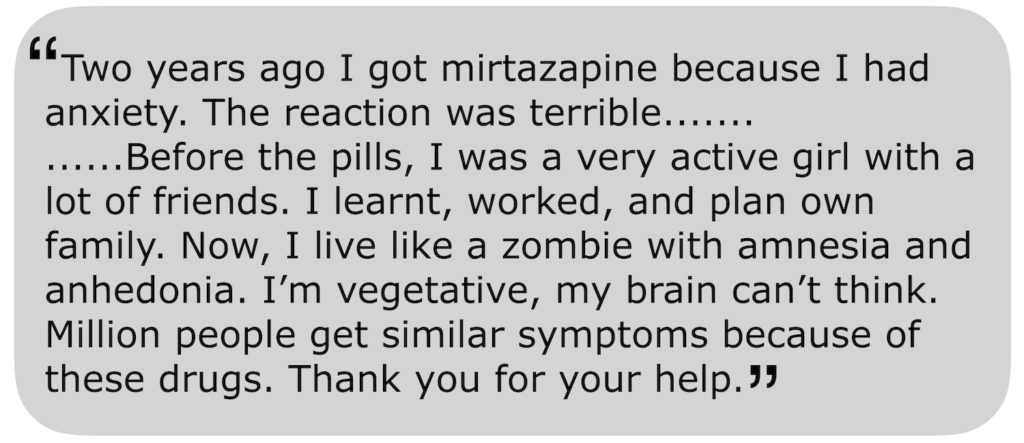
The second, Jo Denison ended her life on November 2, 2018, aged just 35. In her petition submission, she said:
Stevie reminded us all that we must hold two truths in mind with antidepressant drugs. One is that they help people and save lives, but the other reality that we must confront is that they can harm people and take lives too.
For my part, I briefly shared my own experience of being prescribed and then withdrawing from an antidepressant and my recent involvement in campaigning and awareness-raising. I went on to outline why the official guidelines from the National Institute for Health and Care Excellence (NICE) are of little use for anyone who wishes to withdraw slowly and safely. I addressed some of the options available to those who do wish to withdraw slowly and went on to talk a little about potential solutions including Tapering Strips developed in the Netherlands and written about in a study in the journal Psychosis.
Following the formal talks, an audience question and answer session was held in which we discussed more about the link between talking therapies and increased prescribing through referrals, functional medicine as opposed to the medical model and how we can raise more awareness and try to deal with the problems discussed. We also heard moving personal testimonies from attendees of their experiences of taking and withdrawing from a range of psychotropic drugs.
Part 2 – Audience Q&A
I think we all felt that it would have been good for more Assembly Members to be present throughout, but the fact that these issues were being publicly discussed on their turf was a significant achievement.
In parts of Wales, one in six adults takes antidepressants and this is higher than England or Scotland. Support for anyone struggling with dependence or withdrawal issues is patchy and inconsistent and much of it depends upon whether your doctor has had any prior experience of such difficulties. North Wales has a prescribed medication service which joins a very small number of officially recognised support services, including the R.E.S.T. service, previously written about on Mad in America. Other support is most commonly in peer-led initiatives such as P.A.S.T Wales, The Bristol and District Tranquilliser Project and Oldham Tranx which arose from an initiative led by veteran benzodiazepine awareness campaigner Barry Haslam.
In the UK there does seem to be momentum building with a review into drugs that can lead to dependence led by Public Health England with support from the Council for Evidence-Based Psychiatry, more reporting on TV and in newspapers of the problems of dependence and withdrawal and more engagement on social media with the Royal College of Psychiatrists and other campaigners.
What action the Welsh Assembly takes in response to this thorough airing of an issue that is slowly gaining mainstream attention remains to be seen, but I personally feel that we have taken a huge step forward in confronting the problems associated with a less than cautious approach to prescribing.














> [antidepressants] help people and save lives
It’s a lie! There is no proof!
Find a single study that proves that antidepressants have saved a single life! Where is this study? People who lie do not represent me!
The meta-analysis of Healy & Whitaker (2003) shows that the suicide rate is 5 times higher with antidepressants than with placebo!
Enough of lies! Enough of complacency! Whenever someone spreads this lie to please the pharmaceutical industry and the “medical community”, there will be people taking antidepressants and committing suicide! It’s a lie that kills people, so stop spreading it, right now!
Healy, D., Whitaker, C. (2003). Antidepressants and suicide: risk-benefit conundrums (html) Psychiatry Neurosci 2003; 28 (5)
Report comment
I have not listened to the entire talk, so don’t want to comment on that yet. But do want to point out that I do personally know people who do believe the antidepressants help and/or helped them. Despite me personally having the common symptoms of antidepressant discontinuation syndrome being misdiagnosed as “bipolar,” which was harmful, not helpful, to me personally. And I will mention it’s a tremendous shame that this type of misdiagnosis, is no longer considered malpractice, according the the DSM5.
I do believe that those that believe in the efficacy of the antidepressants are likely people who have benefitted by the placebo effect, rather than actual antidepressant benefits. But, I do believe we should be respectful to all.
I don’t know, other than it’s a shame our medical community seemingly doesn’t know anything about the common adverse and withdrawal symptoms of the drugs they prescribe. It is shameful the doctors are so brainwashed by the pharmaceutical industry. The doctors should not be doing pharmaceutical drug testing on the masses, rather than proper drug testing being done, prior to the masses being force drugged by miseducated doctors.
The whole situation is largely proof that none of our governmental organizations are doing their job. Instead these governmental organizations are all seemingly functioning in a manner that works to destroys humanity, for the benefit of the corporations, who control our government officials via our fraud based monetary system, including the medical community.
Medicine should still be viewed as an art, as it historically was, not a science. “’It is far more important to know what person the disease has than what disease the person has.’― Hippocrates.” The pharmaceutical and insurance industry’s fraud based claims of “evidence based medicine” are just that, scientific fraud based medicine. How sad, and sickening, so many doctors have fallen into the belief system of today’s fraud based, pharmaceutical and insurance industry’s medical guidelines.
Especially since it was known by medical researchers, since the turn of the century that, “It is now evident that the American medical system is the leading cause of death and injury in the US.”
http://www.webdc.com/pdfs/deathbymedicine.pdf
This scientific fraud, of the for profit only motivated, misdiagnosis of psychiatric/medical child abuse covering up “mental health” industries, that currently exists, within Western civilization’s paternalist religions and medical industry’s needs to end, not be exported.
Report comment
I have to agree. There are studies–but they’re very skewed and conducted by folks who should recuse themselves from such research the way judges won’t preside over cases where they have vested interests.
At the same time, I don’t want to hurt people’s feelings. We need to show compassion to the deceived.
For the deceivers it’s another matter. “Shame patients. Praise pills,” is the mantra of today’s shrink.
If someone says, “My meds give my life meaning and hope,” I sigh with pity. If you live to consume drugs and all your hopes are in the latest pill, you must have one sad life. My hope is you’ll discover the truth and be set free.
They don’t believe in themselves, so the capsule or tablet is the lucky talisman given by the witch doctor (shrink.) Incidentally the witch doctor has taught them not to believe in themselves but be totally dependent on him and believe all he says without question.
Report comment
Hi James, this is fantastic. I think the reason the UK is moving forward on this, is because people are at last speaking out!
Report comment
There is nothing fantastic about it! We have to give change to the psychiatric industry! They destroyed, they deserve to be destroyed in return!
Report comment
Thanks Fiachra, hopefully we can get more public discussion going on this in 2019.
Report comment
One in six of the Welsh on antidepressants OMG!
Report comment
Thank you to James for writing this – and to MIA for publishing.
This has facilitated a couple of mentions/references published in BMJ rapid responses (to an 18 December BMJ ‘News’ article about ‘Treatment Resistant Depression’ – see below for full text). https://www.bmj.com/content/363/bmj.k5354/rapid-responses
—————————————
This is the full text of the BMJ article: (others can respond too! – via link above)
News
Treatment resistant depression: what are the options?
BMJ 2018; 363 doi: https://doi.org/10.1136/bmj.k5354 (Published 18 December 2018)
Cite this as: BMJ 2018;363:k5354
By Greta McLachlan (BMJ)
Some patients with treatment resistant depression have tried up to 12 antidepressants and waited 10 years before they are seen at specialist centres, a recent press briefing heard. The figures fall far short of targets set out in draft guidance from the National Institute for Health and Care Excellence, which says that all patients who have not responded to two antidepressants should be referred to specialists.1
NICE’s definition would mean that 2.7 million people in the UK have treatment resistant depression (between 10% and 30% of people with depression), an unmanageable number for the NHS’s psychiatric services.
Allan Young, honorary consultant at Maudsley and Bethlem Hospitals in south London, told the briefing that though GPs were good at identifying and treating depression, “TRD [treatment resistant depression] is a subgroup—and there isn’t the capacity in secondary mental health teams to deal with this.”
So what are GPs supposed to do? The answer it seems is, first, know the options and, second, know when to refer.
Second line options
After trying selective serotonin reuptake inhibitors or serotonin and norepinephrine reuptake inhibitors, GPs could try the multimodal serotonin stimulator vortioxetine, said Young. If symptoms persist after an adequate dose and trial of this, patients should be reassessed for diagnosis, adherence, and other comorbidities, he said.
Adding in psychotherapies such as cognitive behavioural therapy is the next option. If this is unsuccessful, adding an atypical antipsychotic, such as lithium, quetiapine, or aripiprazole, has been shown to be beneficial.2
The thyroid hormone liothyronine (T3) is another effective adjunct second line treatment with few side effects.2 Although its price has risen 6000% over the past 10 years, from £4.46 for 28 pills in 2006 to £258 in 2017, it is still useful, said specialists.
Tony Cleare, professor of psychopharmacology and affective disorders at the Institute of Psychiatry, Psychology and Neuroscience at King’s College London, said that if GPs don’t think they are adequately trained to prescribe these drugs they should refer patients to specialist centres. And any patients about whom GPs have concerns or GPs believe are not coping with their depression should also see a specialist, said Young.
“GPs used to ask me, ‘Who should we refer?’ You should refer people that you think need referring. It sounds a bit daft, but it’s the old gatekeeper model: if you refer everyone willy-nilly then the whole system will break down,” he said.
On the horizon
James Rucker, honorary consultant at the Maudsley and Bethlem Hospitals, says that there have been relatively few medical advances in depression treatment since fluoxetine (Prozac) hit the scene in the late 1980s.
“As the pharmaceutical pipeline has run dry, people have looked to history for inspiration,” he said, pointing to investigations by his team at King’s College London into psilocybin.3
In the 1960s psilocybin was marketed as a medicine by Sandoz (now Novartis) as a “catalyst” for people with treatment resistant depression. In a systematic review of clinical trials Rucker has shown that approximately 80% of patients who were given psilocybin showed clinical improvement.4 This did not mean “we are saying psilocybin is ‘safe,’” he said, or that it was an effective drug for treatment resistant depression, “but we are trying to work out if it is.”
In 1970 psilocybin was made a schedule 1 drug in the UK, making it nearly impossible to use in clinical trials. The evidence that placed psilocybin into schedule 1 was “flimsy,” said Rucker, and public opinion on the drug is now shifting, making it possible for him to study psilocybin in the same way as all potential new medicines.
Ketamine
It’s a situation similar to that of ketamine, although ketamine is still used routinely in hospitals and “field” settings such as conflict or disaster zones.
A 1996 randomised controlled trial showed that ketamine had an almost immediate effect on treatment resistant depression. Patients’ symptoms improved within an hour, and the effects lasted for up to seven days. These results have been replicated numerous times, and ketamine is now being used to treat treatment resistant depression in specialist centres. It is delivered as an intravenous infusion, taking about an hour to administer.
The drug company Janssen is trying to develop an intranasal ketamine spray, which would make the process of administration much quicker and cheaper.
James Stone, of the Institute of Psychiatry, Psychology and Neuroscience, told the briefing: “[Our] Oxford clinic is overrun with people wanting ketamine treatment as their depression is so bad.”
Ketamine spray could be available in the United States as early as next year, he said, and enter the European market two or three years later.
However, neither ketamine nasal spray nor psilocybin would be take home drugs. They would still need to be administered in controlled environments, much like methadone is now, agreed the specialists.
ENDS
Report comment
Why do you report this psychiatric comment? There is no depression, there are only little informed naives and drug dealers, having nothing to do with humanity. All is just drugs and chemical balancing for these doctors who hide their cruelty and greed behind good feelings and a junk professionalism. I can not advise the depressive people too much to take their life in their hands by the most resolute means, and not to be euthanize as an animal, since psychiatric drug addiction is only a slow agony of human consciousness.
Donald Trump announced the death penalty for drug dealers. I say that he is a hypocrite! The drug dealers are in his government, in his companies, and their tentacles extend into the most shabby medical offices in the United States! And they talk openly about the best way to intoxicate the population in their medical journals, and nothing happens to them! Oh, do these people like to talk about the death penalty for drug dealers? Well, they will have a surprise on the day of the revolution!
Report comment
Yes indeed. That BMJ ‘News’ article (quoted in full) was published this week – and perhaps others will also respond to the BMJ about it? If you click the link near the top of above post, you will see that some of us have had responses published, and have included link to the MIA article. The BMJ only publishes some selected responses. It feels important to take our discussion to the medical profession – so not to be just talking between ourselves but talking with the medical profession in a ‘mainstream’ medical journal.
Report comment
Greta McLachlan is not a human being, because she identifies human feelings to diseases.
And do not tell me, “but if she is also a human being!” she is not human in the philosophical and political sense of the term. She constitutes a terrible and mortal danger for humanity, she degrades, she defiles humanity by her propaganda and her treatments and should be prevented to harm by the most resolute means.
Her existence raises my heart because it represents everything I hate: hypocritical, dirty, she promotes ketamine and psilocybin, presenting them as miracle drugs capable of resolving depression in 7 days! What is the BMJ, the journal of itinerant doctors of the 19th century? It’s a shame that the BMJ publishes this kind of insanity, it’s like the Wild West! Let’s throw this fake doctor into the trash!
Report comment
The problem, Marion, is that would involve paying tribute to the “psychiatric experts.” As a survivor of psychiatry’s drugs and mind games I refuse to acknowledge it as a legitimate branch of medicine. Societal control is its true function.
I’m sure they have no interest in anything “crazies” say unless its telling how
“Psychiatry saved my life! Now I no longer go on drinking binges and wake up with strangers in my bed. I get along with everybody, have a wonderful career, a happy, affectionate marriage and am a pillar of the community.”
The truth is the exact opposite happened. Never a party animal, I’m a lonely virgin at 45, my health is ruined, and 25 years of psych drugs/labels destroyed all chances of gainful employment after my teens. I’ve no interest in more effective mind altering drugs to perhaps stop my heart from beating or mess up my thinking again.
There can be no dialogue with those determined to use us as subhuman test subjects. Who dismiss anything but mindless hymns of praise to their guild as proof of Severe Mental Illness and would lock us all up for drugs and shock if possible.
If you’re trying to foist more brain drugs on gullible consumers this is the wrong place, btw. Most of us are fighting or have fought like mad to get OFF those things. Like trying to sell handcuffs to someone kidnapped and forced to wear them for 20 or 30 years.
Psychiatric drug promotions are NOT welcome here.
Report comment
Sorry – there is a misunderstanding here. Perhaps MIA moderator can delete the text in my post at the top of this thread that is causing offence. (I don’t seem to be able to edit it now).
Report comment
Writing as moderator: I will take a look and see what I can do to make it understandable.
Report comment
Posting as moderator: I read what I think is the post (the BMJ references) and was myself confused as to what is yours and what is quoted from someone else. That said, I didn’t find anything in there particularly offensive – it just seemed like an outline of the kind of “thinking” one sees in medical journals, contrasted with the very important comments on the article about side effects. What I got out of it was that, rather than recognizing that the so-called “ADs” are ineffective and even destructive in what appears to be the majority of “patients,” they blame the patients or their “TRD” and continue to insist that their “treatments” are effective.
If there is another interpretation, let me know.
If you do want me to delete part of the post, please let me know which part you mean and I can do this for you.
Report comment
No, Marion Brown, there is no offence. You shocked us but this text is not yours, so you do not have to pay for it. We do not shoot at the messenger.
Report comment
It’s a good thing to quote Greta McLachlan to show how disgusting psychiatry is, to show that senior psychiatrists promote illegal drugs as thugs to advance their careers.
“[Our] Oxford clinic is overrun with people wanting ketamine treatment as their depression is so bad.” said James Stone.
Ketamine, ketamine! Give us ketamine!
They are the Mafia.
Report comment
Sorry Marion. I was unduly harsh. Apparently you weren’t even defending treatments (coercive at least.)
I still doubt they’ll publish comments from “ungrateful consumers” like me.
Don’t kill the messenger. 🙂
Report comment
Thank you Steve – and Sylvain. You have picked up what I was meaning to show! The reason that I quoted the full BMJ article is that is only accessible in part on the BMJ website. This BMJ News report, complied by a BMJ writer, summarises what the ‘experts’ are ‘advising’ our family doctors (GPs) …. and right now! VERY alarming.
Report comment
I support the motion that Depression as an illness, was more or less invented in the 1980s to support the sale of Prozac.
Report comment
Our society has a big problem with Sadness Shaming. Like we need an excuse not to be ecstatically overjoyed 24/7.
Doctors love selling pills for the “disease” of unhappiness. But SSRI’s are a smashing success only because people have no tolerance for painful emotions and think sadness is sinful. (I was told this in church. Now they say, “Depression is a sin unless you have the mental illness bipolar. Which is really a physical illness you’re born with and can’t help without ‘meds.'”)
We have a right to unhappiness! If you’re freakishly happy all the time you must be stupid, insensitive, selfish, sheltered, or a combination of the above.
Happy happy joy joy. 😛 Please pass the Soma.
Report comment
“If you’re freakishly happy all the time you must be stupid, insensitive, selfish, sheltered, or a combination of the above.”
Not sure what would constitue “freakishly” happy, but overall, this sentiment evokes sadness in me, and feels a bit double-binding. If we have a right to unhappiness–which I would agree and to me it goes without saying that we all have the right to feel our true and authentic feelings–do we not also have a right to be happy, without being judged or labeled for it?
I believe what causes problems is when people try to impose their feelings on others, rather than simply owning how they feel toward anything as their own experience, and not necessarily that of others. “You should be unhappy” and “you should be angry” are just as imposing, oppressive, and unrealistic as “you should be happy.” But I do think lableing people for how they feel in any respect is, to me, where psychiatry and DSM go way wrong. I also think that labeling people for being happy is the same thing.
Report comment
By “freakish” I meant unnaturally. Being a phony.
I realize the rest of what I said about “stupid, insensitive, selfish….” contradicts this. But I have had nurses and social workers in psych wards–later case managers in centers and clubhouses–who lectured us on how crazy we were for not being happy as they were. If they were on disabling drugs and segregated in crushing poverty they might not grin ear to ear either.
“How come you’re not smiling all the time like my super awesome hubby and kids and I did during our Caribbean vacation?” Save it for Facebook Missy! 😛
Covetousness is a sin. So’s arrogance and mocking the suffering.
Report comment
If it’s phony, then the “happiness” is merely a front, not really happy of course. In fact, it doesn’t sound like a very enviable position to be in. Projecting a phony front takes a lot of work and effort and generally carries a great deal of anxiety from all that splitting. I think being authentic is relatively easier, and is where truth comes to light.
I do agree that the lack of senstivity and empathy in the mh industry is over the top. The most memorable line I ever heard from a group therapist in social services was “take your meds and don’t make waves”–not to me, but to a group member who was experiencing crime in his housing. Doesn’t sound like a very happy therapist to me, in fact I’d say she was quite angry, and she said a lot of stuff like this, and indeed, was blatantly ridiculing. Consistent with the rest of my experience with the mh world.
That is one angry and fear-based industry, projecting tons of phoniness, which is why it resorts to control and manipulation, followed by avoidance if questioned. To me, this is the epitome of *lack of integrity.* And that’s the nicest thing I can say about the industry, in all sincerity.
Report comment
I would also like to point out on the topic of informed consent:
Psychiatrists do not warn their patients that all psychiatric drugs can cause severe hyponatremia and a complication of severe hyponatremia; the osmotic demyelination syndrome.
My daughter was prescribed Citalopram without my knowledge when she was 19 years old. She repeatedly developed cerebral oedema and dropped out of college. She was left struggling and lost weight. The prescribing psychiatrist (who self described as suffering from bipolar disorder) diagnosed her with bipoloar and an eating disorder and prescribed her a 1500 calorie a day meal plan (basically a starvation diet). She was referred to an Eating Disorder Program and seen by the director who diagnosed her with 8 psychiatric conditions when she was very seriously ill. She complained of nausea and vomiting. He described her binging and purging! She told him she was too ill to leave the house. Agoraphobia. Attempting to follow the psychiatrists orders. Obsessive Compulsive Disorder ….
The internists listened to the psychiatrists, not Lucie or us. They also left her struggling believing she was mentally ill, eating disordered …
Finally she was found delirious rolling around in the puddles late at night with severe hyponatremic delirium. On admission to hospital, a psych consult was called for (again). The ER physician missed her sodium level of 124 and sent her to the psychiatric unit with severe hyponatremia and cerebral oedema. Her sodium levels were left unmonitored in PAU. As she was so malnourished, she developed a complication (osmotic demyelination syndrome) which can occur in malnourished patients. It develops 4-5 days later with fluid shifts in the brain. Instead of sending Lucie to ICU for desmopressin the PAU pychiatrists discharged her home to suffer ODS 4 days later.
Lucie was not over-corrected in hospital. Her sodium level auto-corrected, meaning SSRI’s not only cause severe hyponatremia, they directly cause ODS due to extreme fluctuations in sodium levels. There are hundreds of case reports of this. However, peer reviewed journals still claim that SSRI’s have no serious adverse effects despite many studies showing approx 32 -40% of patients !!! (all ages, NOT just the elderly) develop hyponatremia on SSRI’s. One study showed that 100% of patients over 62 years of age develop hyponatremia on 3 SSRI’s. Described as “a rare side effect sometimes seen in the elderly”.
Even neonates born to women taking SSRI’s late in pregnancy have been found with severe hyponatremia. How many develop ODS and permanent brain damage which is never diagnosed?
Phototherapy enhances serotogenic effect!
Lucie was seen by over a dozen psychiatrists that fall and NONE recognized the potentially fatal side effects of their drugs. Likely because their peer reviewed journals deny that hyponatremia is a serious adverse effect (!)(despite this being well known in all fields of medicine).
SSRI’s are “the tx of choice” because of their “favourable side effect profile”. This is how they are described compared to older drugs in hundreds of thousands of peer reviewed articles. No mention of a COMMON and life threatening side effect that occurs in approx 40% of patients!!! Unbelievable.
Lucie was permanently brain damaged when she was 19. She was admitted to a psych ward when she developed ODS as she went mad with despair. On the unit, they discovered her brain damage with Montreal Cognition tests but concealed all of this from me and Lucie’s Dad. They refused to allow her to be seen by neurology as I requested because she suffered brain damage due to medical negligence.
She was drugged against her will for 2 months without sodium monitoring. A miracle she wasn’t found unresponsive in her bed (another hyponatremic episode).
She was mis-diagnosed as mentally ill for the rest of her life (personality disordered) and the psychiatrists refused to investigate for brain damage. I discovered all this in her records when she died, age 24. She was my only child. my sunshine.
Report comment
“Psychiatry Changes Lives”
They punish you when you don’t obey, and they punish you when you do;
They label you “borderline personality disorder” when you are sexually active;
They label you “disassociative” when you aren’t.
When you smile they tell you you’re “manic”–
When you don’t smile–or can’t–they say you have a “flattened affect.”
When you cry because they ruined your life they say you need massive doses of the drugs damaging you–or ECT.
When you gain massive amounts of weight on their drugs they say you’re too dumb to eat properly.
They take notes of your poor organizational skills after destroying your frontal lobes.
They take notes of your poor interpersonal skills after destroying your amygdala.
When the community shuns you, they lament how Ignorance causes Stigma–
Because Stigma can be bad for drumming up business–but great for enforcing AOT.
Then the high ranking bigwigs show up on national television to say how YOU have no conscience or empathy and lie all the time.
Being a psychiatrist means turning violent criminals loose on the public (They’re “meds” compliant!) Demonizing the “patients” like no other medical specialist would.
An aversion to the truth.
Crippling and killing the innocent through pointless experiments.
The Thief who only breaks in to kill and destroy.
People of the Lie.
Report comment
I’m so sorry they killed your baby, Niki. She was an adult, and turned to them on her own. It is no consolation, but at least you do not have to bear the burden of being the one who sent her to them. Again, I am so sorry they killed your sunshine (Lucie means light).
Report comment
Niki, you obviously loved your daughter. She was lucky to have you for a mother during her short life.
You couldn’t save her from those who slated her out for destruction. But knowing you loved her must have been some consolation for poor Lucie even as she suffered.
Report comment
My sincere condolences for your Lucie. I am so sorry.
Something about this description of induced hyponatremia is setting off alarms for me– during my long SSRI weaning process, I developed a gastrointestinal condition that made my electrolytes tank over the long term. During that time, my withdrawal became worse and…strange. I’ve never felt quite right about it. I am so sorry for what happened to your family.
Report comment
Interesting article!
Report comment