
“For more than 25 years,” Michel Lejoyeux and Jean Adès confirmed in their 1997 essay “Antidepressant Discontinuation,” “physicians have known that abrupt or tapered withdrawal from antidepressants can produce discontinuation phenomena consisting of somatic and psychological symptoms. Flu-like symptoms; gastrointestinal distress, including nausea and vomiting; arrhythmias; anxiety; sleep disturbances; movement disorders; mania or hypomania; panic attacks; and delirium have all been reported.”
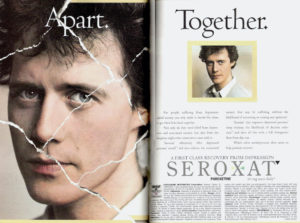
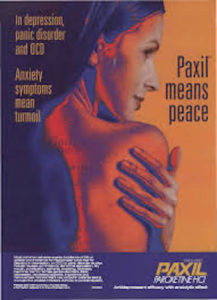
The Paris-based researchers were, however, referring to imipramine and other tricyclic antidepressants from the 1950s, discussed in my previous post, and were keen to cast their second-generation counterparts, selective serotonin reuptake inhibitors (SSRIs), as largely “well-tolerated” and not dependency-inducing. The new class of antidepressants (Prozac, Zoloft, and Paxil, in particular) were at worst said to produce “transient, mild,” and self-resolving symptoms lasting up to 7-14 days after treatment.
Lejoyeux and Adès claimed at the time that incidence rates for SSRI withdrawal reactions varied between “0% for fluoxetine [Prozac], 50% for paroxetine [Paxil], and 86% for fluvoxamine [Luvox]”—rates that subsequent systematic reviews determined were set too low. Just as significant, the researchers were instrumental in renaming antidepressant withdrawal as “discontinuation syndrome,” a term the drug companies favored because it implied treatment had ended too soon and needed to be resumed, either at a higher dose or on a different drug.
The 7-14 day time-frame for “discontinuation” would be repeated almost unchallenged for more than two decades, including by professional associations such as the UK’s National Institute for Health and Care Excellence (NICE), Royal College of Psychiatrists, and the American Psychiatric Association, which has yet to update its prescribing guidelines. It would also be used (including by those same professional bodies) as a way to minimize or outright deny the existence of longer-term withdrawal, which was subsequently found to last months, often years.
These associations might instead have paid closer attention to the concerned letters their professional journals began to receive just months after the drugs’ formal approval—letters largely ignored by the leaders of clinical trials, who until recently tended to dismiss them as anecdotal evidence, mostly valueless in altering the drugs’ treatment profiles.
In what appears to be the first of these patient reports for SSRIs, Linda Barr and colleagues at Yale University noted in 1994 several cases of mild-to-severe adverse effects following “abrupt discontinuation” of paroxetine (Paxil). They included “severe vertigo, gait instability, nausea, emesis [vomiting], and diarrhea,” which were described as debilitating for 7-10 days, though as “resolv[ing] gradually over the following week.”
The following year, 1995, Miki Bloch and colleagues at the National Institute of Mental Health wrote to the Lancet about two cases of “severe psychiatric symptoms associated with paroxetine withdrawal.” In both cases, “men without a history of major psychiatric disorder developed severe behavioural symptoms when paroxetine was withdrawn.” The first of them, a healthy 36-year-old, reported on his second day of withdrawal “hypomanic-like symptoms, including hyperactivity, decreased need for sleep, and irritability that developed into agitation, aggressiveness, and volatility.” After two additional weeks of fluctuating symptoms, he began to “experience ego-dystonic impulsive behaviour such as shoplifting and suicidal impulses and gestures.”
In the second case, involving a healthy 48-year-old male who tapered paroxetine over a 12-day period, the patient had in his second week “developed physical symptoms of dizziness, blurred vision, nausea, lethargy, and insomnia. He also reported feeling angry, irritable, and short-tempered … with some highly atypical explosive vocal outbursts and tantrums. He became preoccupied with homicidal thoughts and plans, initially directed towards acquaintances and later towards his own children. These became so intense and ego-dystonic that he contemplated suicide. Physical and behavioural symptoms lasted about 9 days and then remitted spontaneously over 2-3 days”—that is, far into his third week of withdrawal.
Also in 1995, this time in the American Journal of Psychiatry, Robert Pyke at the University of Michigan wrote of a 44 year-old white woman who had terminated treatment on 10-20 mg/day of paroxetine, following “complete remission of depression and anxiety,” because of twitching, dizziness, nausea, and anorgasmia. On her third day after tapering, “Ms. A began to experience anorexia, nausea, and diarrhea and had a shaking chill. Eye movement produced visual lag, dyscoordination, and an unpleasant occipital feeling of movement. These apparent withdrawal symptoms were unlike prior symptoms and were incapacitating for the second through the fourth days of symptoms. On the 11th day, symptoms improved, but dizziness and diarrhea recurred intermittently through the 23rd day” (emphasis added).
“In the package insert,” Pyke complained, “the manufacturer of paroxetine [GSK] lists withdrawal syndrome, without description, among rare adverse reactions (fewer than one in 1,000 patients). Dizziness, nausea, and diarrhea, but not the other symptoms, were reported previously in a few patients after withdrawal. The 3-week duration of symptoms was longer than the 5-15 days reported by the manufacturer.” By February 2001, under pressure from a larger evidence-base of adverse effects, the drug-maker would raise that number (1/1000) significantly, putting the overall number affected by withdrawal symptoms at fully 20% of patients, or an eye-opening one-in-five.
Physicians Lloyd Frost and Samarthji Lal then wrote from Canada in a follow-up 1995 issue of the American Journal of Psychiatry that three of their patients had complained of “shock-like sensations after discontinuation of SSRIs.” Two days after stopping paroxetine, the first of these, a 32-year-old man diagnosed with OCD, “complained of electrical shocks’ that ran quickly through his upper body and down his arms and hands. The[se] lasted a few seconds but occurred constantly if he moved. Keeping his head motionless prevented the shocks. At times the shocks made walking difficult, so he would lean against the wall for support. Five months of gradual paroxetine withdrawal led to cessation of the shocks” (emphasis added).
A second patient of theirs, a 28-year-old man, similarly “complained of ‘electric-like waves’ that ran from his forehead and stopped in his abdomen.” These would last five seconds and recur 3-5 times each evening. He “also experienced nausea, light-headedness, insomnia, inner shakiness, and dizziness that [also] forced him to hold onto the wall to walk. Symptoms subsided with a week except for the electric-like waves, which lasted 3 weeks” (emphasis added).
A third man, aged 22 and prescribed sertraline (Zoloft), suffered the first of several attacks of “electric shocks” while in a swimming-pool, with a force so debilitating he “thought he ‘was being electrocuted.’ At times his ‘whole body would fly back,’” Frost and Lal report in astonished concern, “which once led to a brief loss of control of his car’s steering wheel…. Less intense shocks persisted for 4 weeks and ceased 13 weeks after sertraline cessation” (emphasis added).
In each of these cases, notably, even gradual tapering from SSRIs had generated chronic adverse effects up to five months later.
Although it needs to be emphasized that the first randomized controlled trials of SSRIs made no mention of these recurring and concerning patient reports, they determined independently that “19 out of 55 patients (34.5%) reported at least one adverse event on discontinuation, compared with 7 out of 52 (13.5%) on placebo.” Oehrberg and colleagues also determined in 1995 that 77% of those in the paroxetine group reported at least one adverse event (compared with 55% in placebo), a difference they presented as “statistically significant (P = 0.012).” Even so, they concluded: “Overall, paroxetine was well tolerated and most patients were able to discontinue abruptly without ill effect, even from higher doses (40 and 60 mgs).”
Three years later, by contrast, an RCT sponsored by Eli Lilly and led by Jerrold F. Rosenbaum and Maurizio Fava at Massachusetts General found that “abrupt interruption of antidepressant therapy for 5-8 days” was in fact “associated with the emergence of new somatic and psychological symptoms in patients treated with paroxetine and to a lesser degree sertraline, with few symptoms seen with fluoxetine.” The latter drug (Prozac), notably, was made by the pharma company sponsoring the trial.
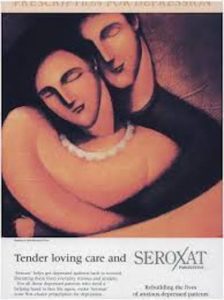
As Prozac had first entered widespread use in 1986, with Zoloft following in 1991 and Paxil in 1992, even the 1996 Lilly-sponsored symposium on discontinuation took place a full decade after the first of the new antidepressants had been approved and marketed for mass use. Adopting wholesale the talking-point that the newer drugs were virtually free of withdrawal symptoms and dependency problems, with high tolerance, the media’s coverage was uncritical, almost giddy in enthusiasm. Prozac became a blockbuster drug from cover stories in Newsweek and Time. Peter D. Kramer’s Listening to Prozac (1993) coined the phrase “cosmetic psychopharmacology” to warn that use of SSRIs might spread beyond prescribing for conventional illness, leading to an embrace of the drugs for their alleged capacity to “enhance” personality.
Yet as Bruce Stutz wrote later in the New York Times, in a thoughtful article on his own difficulties tapering Effexor (Venlafaxine), “By then it had become clear that drug-company estimates that at most a few percent of those who took antidepressants would have a hard time getting off were far too low.”
“The symptoms of discontinuation syndrome could be fierce,” he added, recounting in detail, at varying doses, his own harassing problems with brain zaps, panic attacks, insomnia, and despair, even on lower and lower doses of Effexor.
After first raising the possibility of SSRI withdrawal in 1994, Maurizio Fava and colleagues went on to publish several more articles on the phenomenon (a prelude to many more), including in 2006 a paper citing additional withdrawal symptoms such as “agitation, anxiety, akathisia, panic attacks, irritability, aggressiveness, worsening of mood, dysphoria, crying spells or mood lability, overactivity or hyperactivity, depersonalization, decreased concentration, slowed thinking, confusion and memory/concentration difficulties.”
To the authors, as to many researchers, patient advocates, and survivors of psychiatric drugs, these recurring symptoms began to look increasingly like a drug-related syndrome—a problem due largely or entirely to the drug prescribed, with little or no relation to the condition it was supposed to treat.
In my next post on this topic, we’ll see how these far-reaching problems of misdiagnosis and misattribution became too overwhelming to ignore, forcing greater consideration of protracted withdrawal or post-acute withdrawal syndrome (PAWS) as part of an evidence-base academic psychiatry has for decades claimed to uphold and revere as one of its guiding principles.















Thank you Christopher.
Psychiatrists and medical doctors have been pretty lucky, so far.
Not without protection though.
No one is completely insulated, and certainly not forever.
Report comment
A WHOLE! aF Klint would strive to realize the dissolving of boundaries in her work… and yet, to have considered to visit the Broad Institute Mental Health Annual Meeting? What sort of research is really understanding, recovery that understands the space in which the research operates does not even come close to the realities the customer experiences, whole as we strive to be and understand.
Report comment
It is harder to make false claims about how those in withdrawal having bad outcomes prove the drugs are safe and effective if you also admit the drugs cause bad withdrawal. That’s why they hid and lied about withdrawal. They didn’t want to give informed consent because less people would buy their drugs and services if they did.
Report comment
It just pisses me off that I started drug “therapy” with Paxil when I was 6. I didn’t have any say in the matter. And 22 years later I’m still on the drug because the withdrawal effects make it impossible to function even somewhat normally.
Then a few years ago I was popped on Anafranil while I was in a (medical, non-psychiatric) hospital pretty much just because I had a recorded history of OCD. I knew it was an older medication that wasn’t prescribed often anymore, but they promised me that I’d find special relief with it because it had “anti-obsessional properties” and that it’d make an overwhelming difference in my life.
Really, the only major difference that Anafranil has made in my life is the worst dry mouth that you can have. To the point where my teeh are rotting because I can’t produce enough saliva.
I’m still (somewhat) functioning in *spite* of the medication. Not *because* of it. I’d love to go off of them, but in my case the withdrawal effects aren’t worth any minor potential gains.
Report comment
6 years old. Just a baby. Animals get obsessed, but ONLY EVER under pressure. Pressure that comes from outside sources. It takes years to undo those pressures. Pills do not undo them. However they made you take them, instead of correcting the pressure. We fail kids, but they should never ever be made to take illegal drugs and psych drugs are illegal if given to children who cannot identify their handlers, nor the drugs.
They say these drugs are “legal” but they are legal, only as far as the abusive allowances make it so. It is very alarming that an adult gives these drugs to children.
But it is now the society we live in where psych and medicine do whatever they want. Everyone needs a job even if that includes abusing kids and teens.
I’m glad you are functioning to realize what transpired, and I’m glad you are part of the community of awareness.
Report comment
A friend who would be on risperdal would be treated to having all of his teeth replaced by the community mental health and insurance. However, I also wonder if his life was shortened by being on this medication. And unfortunately, the level and consistency of advocacy, by, for and with the citizens who are the customers, diminished in time. On the backside, the interest in trying to create the words, that can convey my stand and/or our stance, can convey an arrogance on my part. To me there is a learning of shaped in the conceptual realm of pure science, then applied science. Currently in medical practice, the increased computer program sifting out a pre-survey, to expedite the visit with the doctor, robotically advances a paradigm by which the corporate advances a position. And in reading this article and posts, I would wonder how to implement a way by which the self-monitoring, a way to document and improve through applied arts and sciences, a healing space that moves with the citizen in need. The oddity, in post hospitalization and care is not about receiving more zoom and post surveys, but I think rather to formalize the advocacy to stronger levels while also realizing the implementation with application….. And I’m not sure about this stream of query, though I think from reading Caplan’s writings, that perhaps the healing space can be imparted or conveyed, even when so much has been endured and witnessed. The ethics I would think when understood are enough to stop the runaway train of mental health “care”. Thanks to the whole of the emergent discourse.
Report comment
I’ve had antidepressant withdrawal induced brain zaps for 20 years and counting, so the withdrawal effects of the antidepressants may be permanent.
Adding a PAWS diagnosis might help prevent the psychiatrists from so often misdiagnosing the common adverse and withdrawal effects of the antidepressants as “bipolar.”
Although the fact the psychiatrists took the disclaimer, which pointed out the impropriety of such misdiagnoses, OUT of the DSM5, does not imply the psychiatrists want to end their iatrogenic harm of others.
Report comment
so important to keep exploring and shinning a light on these cultural disorders. Corporate power and the business model is turning pain into profit and when the treatments cause more pain more treatments or offered for profit – its like we’re all being fed on by some corporate monster.
Christophers book Shyness is also excellent.
Report comment