Taking anticholinergic (aCH) drugs (such as antidepressants and antipsychotics) is associated with an increased risk of developing mild cognitive impairment, according to a new study. Moreover, the drugs interact badly with the APOE ε4 genotype, which itself greatly increases the risk for Alzheimer’s disease. Anticholinergic drugs disrupt acetylcholine production in the brain. The researchers write:
“Our results demonstrate that the use of aCH in cognitively normal, highly educated, and healthy older adults is associated with increased risk of progression to MCI and accelerated cognitive decline, which are exacerbated in the presence of AD biomarkers.”
They add, “Findings underscore the adverse impact of aCH medications on cognition and the need for deprescribing trials, particularly among individuals with elevated risk for AD.”
In the study, aCH drug use was associated with a 47% increased risk of MCI overall. The researchers also found that increased anticholinergic burden (such as adding another drug, using a drug with a stronger effect on acetylcholine production, or taking a higher dose) worsened the effect.
The risk was also substantially increased in people with genetic risk for Alzheimer’s disease and people with the biomarkers of Alzheimer’s disease.
People with the ε4 genotype were already twice as likely to develop MCI than people without the genotype—but being exposed to aCH drugs raised their risk to more than 2.5 times as likely (hazard ratio [HR] = 2.69).
People with biomarkers of Alzheimer’s disease (amyloid and tau proteins) were about three times as likely to develop MCI as people without the biomarkers (HR = 2.98). However, when people with the biomarkers took aCH drugs, they experienced a nearly 5-fold increase in risk for MCI compared with people without the biomarkers who did not take the drugs (HR = 4.89).
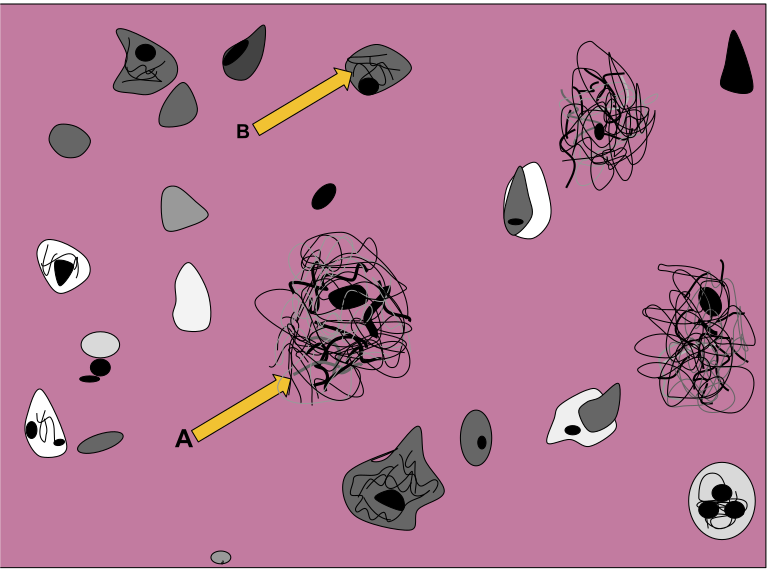
The researchers write that this may reflect a “double hit” in which Alzheimer’s pathology reduces cholinergic neurons in the basal forebrain, followed by the impact of aCH drugs depleting acetylcholine even further.
Declines in memory and language were also steeper for people taking aCH drugs.
The study was led by Alexandra Weigand at the University of California, San Diego, and published in the journal Neurology. The participants for the study came from the Alzheimer’s Disease Neuroimaging Initiative. 688 cognitively normal participants were included, 33% of whom were taking aCH medications. The participants were followed for up to a decade.
The researchers found that, on average, their participants were taking 4.7 anticholinergic medications, and many of them were prescribed doses much higher than recommended; 57% of the medications were being taken at more than twice the recommended dose, while 18% were being taken at more than four times the recommended amount.
Weigand and the other researchers write that “Although deprescribing among all older adults may prove beneficial, the synergistic effect observed between aCH and AD pathologic risk suggests that reducing aCH burden during the preclinical stages of AD may be especially warranted given that this group is particularly vulnerable.”
Other studies have found similar results to this one, including a 2019 study that found especially high dementia risk for people taking antidepressants (29% increased risk) and antipsychotics (70% increased risk) compared to non-users. Similarly, a 2017 study found that higher anticholinergic burden was associated with the risk of cognitive decline. A 2016 study was reported on in Time magazine after finding that anticholinergic drugs decreased brain volumes and impaired brain functioning vital for memory.
Interestingly, other researchers have suggested using antidepressants for dementia prevention because of preliminary findings that the drugs might reduce levels of amyloid-beta-42. There is no evidence that antidepressants actually reduce the likelihood of dementia.
****
Weigand AJ, Bondi MW, Thomas KR, Campbell NL, Galasko DR, Salmon DP, . . . & Delano-Wood L. (2020). Association of anticholinergic medication and AD biomarkers with incidence of MCI among cognitively normal older adults. Neurology. Published online September 2, 2020. DOI: 10.1212/WNL.0000000000010643 (Link)















Thank you Peter,
If a psychiatrist prescribes harmful chemicals, is he really cognitive?
Should he even be allowed to be running around in the playground with
open scissors?
“look, she is comparing our medications to open scissors”
Report comment
Has anyone gotten brain damage from open scissors like the millions who’ve gotten brain damage from psych drugs?
Report comment
At least a scissor injury would be to a specific part of the brain and not flood every single cell in the body.
Report comment
I have come to realize that drugs are prescribed mainly on the basis on flawed and greedy short term studies.
This is really scary, that so few precautions are taken, that risks are blindly discarded and ignored.
Risks are not dutifully considered and explored and this is nothing short of utter madness.
I was a child whose mind was sacrificed by antidepressants.
I grew up with dementia and was so impaired that I actually developped a phobia of productivity (which was severely hampered), as well as a fear of thinking. I had to relearn to talk, so I know what this article is about.
When will there be reason in psychiatry (and medicine), and respect for human life? (and yes this is a cry of desperation)
Report comment
Thank you, Peter, for pointing out what is blatantly obvious to anyone who has ever been forced and/or coerced into taking the anticholinergic drugs.
It’s of paramount importance that the psychiatrists learn this information, since all the psychiatrists I have ever dealt with denied that the anticholinergic drugs could cause any harms, other than “increased thirst.”
Although I must confess, I’m not certain what is “professional” about knowing basically nothing about the common adverse effects of the drug classes one prescribes.
Nonetheless, thank you for helping to educate the psychiatrists regarding the common adverse effects of the mind numbing and dumbing psychiatric drugs.
Report comment
Psychatrists, “You lack insight and the mental ability to understand why you need to be addicted to these cognitive impairing and brain damaging drugs.”
One begins wonder, are there any characteristics of “mental illness” that aren’t also caused by the drugs?
Report comment
Well, given the fact that the two “most serious mental illnesses,” schizophrenia and bipolar, are both created with the psych drugs. And let’s be realistic, depression is most likely caused by depressing real life events, not a “chemical imbalance” in any one individuals’ brains.
“One begins wonder, are there any characteristics of ‘mental illness’ that aren’t also caused by the drugs?” Probably not.
Report comment
Why are you connecting anticholinergic (aCH) drugs to antidepressants and antipsychotics? This is incorrect. Antidepressants and antipsychotics are not aCH based and don’t work on the same neurotransmitters.
Anticholinergic (aCH) drugs are given with antipsychotics when the latter induce movement side effects (EPS) like parkinsonism and others.
Anticholinergic (aCH) drugs are mostly given in the first years of diagnosis of Alzheimer’s Disease under the assumption that it might slow down the disease’s progression. This might be wrong and even lead to the contradictory results, as indicated by the paper you review. Again, this was shown to be the case for a genetic sub-type. So please, even if there is a lot of wrong doing in the pharma industry and the medical practice, it is important to not spread misinformation.
Report comment
You are misinformed, Kerena.
https://www.aafp.org/afp/2010/0301/p617.html#sec-3
https://www.goodrx.com/blog/new-study-finds-that-some-drugs-may-raise-dementia-risk-as-many-as-20-years-later/
https://utswmed.org/medblog/depression-medication-dementia/
https://www.ti.ubc.ca/2018/09/10/113-anticholinergic-antimuscarinic-drugs/
Report comment
Thank you, Peter, for this important article. People should certainly be warned about these risks prior to starting psychiatric drugs.
Report comment