Editor’s Note: Over the next several months, Mad in America is publishing a serialized version of Peter Gøtzsche’s book, Mental Health Survival Kit and Withdrawal from Psychiatric Drugs. In this blog, he discusses the colossal overprescribing of prescription pills. Each Monday, a new section of the book is published, and all chapters are archived here.
The final nails in the coffin of biological psychiatry
When I discuss the state of psychiatry with critical psychiatrists, psychologists and pharmacists I collaborate with, we sometimes ask each other: “Who are most mad, on average, the psychiatrists or their patients?”
This is not as far-fetched or rhetorical a question as it may seem. When I Googled delusion, the first entry was from an Oxford dictionary: “An idiosyncratic belief or impression maintained despite being contradicted by reality or rational argument, typically as a symptom of mental disorder.”
As you have already seen, right from the start of Chapter 1, and will see more of in the following, the whole of psychiatry is characterised by exactly this. The psychiatrists’ predominant idiosyncratic beliefs are not shared by people considered sane, i.e. the general public, but the psychiatrists forcefully maintain them, even when reality, including the most reliable science we have, and rational argument clearly show that their basic beliefs are wrong.
If psychiatry had been a business, it would have gone bankrupt, so let’s conclude instead that it is morally and scientifically bankrupt.
One definition of madness is doing the same thing again and again expecting a different result. When a drug doesn’t seem to work so well, which is most of the time, psychiatrists increase the dose, change to another drug from the same class, add another drug from the same class, or add a drug from another class.
The science tells us very clearly that these maneouvres will not benefit the patients. Switching drugs, adding drugs or increasing the dose do not result in better outcomes.156-158 What is certain is that increasing the total dose or number of drugs will increase the occurrence of serious harms, including irreversible brain damage, suicides and other deaths.4,159,160 Neuroleptics shrink the brain in a dose-dependent manner; in contrast, the severity of illness has minimal or no effect.160
There is no reliable evidence that the psychosis per se can damage the brain.161 The same applies to other psychiatric disorders, but psychiatrists often lie to their patients, telling them that their disease might harm their brains if they do not take psychiatric drugs. Psychiatry professor Poul Videbech wrote in 2014 that depression doubles the risk of dementia,162 but the meta-analysis he cited did not mention with one word which treatments the patients had received.163 Other studies indicate that it is the drugs that make people demented.164,165
It is routine everywhere to increase the dose, even when the patient has become better. An often-heard comment at conferences at psychiatric wards is: “The patient is doing well after two weeks on Zyprexa, so I will double the dose.” This routine is both insane and harmful. The psychiatrist cannot know if the patient might have improved more without Zyprexa. The doctors mislead themselves and their patients all the time based on their misleading “clinical experience” and their treatment rituals go directly against the science.
In this way, many patients end up on terribly harmful drug cocktails they might never escape from. Although it’s hard to believe, it’s getting worse. A US study of office-based psychiatry found that the number of psychotropic medications prescribed increased markedly in just nine years up to 2006: visits with three or more medications doubled, from 17% to 33%.166 Prescriptions for two or more drugs from the same class also increased, although this shouldn’t happen at all.
I was once invited to follow the chief psychiatrist during one day at a closed ward. We talked with several patients. One of them appeared totally normal and reasonable to me, but to my big surprise, the psychiatrist asked me afterwards if I could see that he was delusional. As I couldn’t, he explained the patient was delusional because he had been on the Internet and had found out that neuroleptics are dangerous. I replied that they are indeed dangerous and that there is nothing delusional in believing this. I was so stunned that I said no more.
On another occasion, I phoned a psychiatric department in Copenhagen that has a very bad reputation because of the patients the psychiatrists have killed there with their drugs.45 A desperate patient in great distress had rung me, but it wasn’t possible for me to get through to a psychiatrist, although I am a colleague and it was within normal working hours.
I insisted that I needed to talk to someone and was transferred to a head nurse. She told me not to become involved because the patient was delusional. When I asked in what way, she said he had found out that neuroleptics were dangerous. I asked her if she knew whom she was talking to. Oh yes, she knew about me.
I shall now illustrate more of the absurd, delusional world of psychiatry with some examples.
One of my psychiatrist friends sent a letter to a family doctor about a 21-year-old student, recently discharged from a private hospital after she had been given TMS 21 times. When I asked what this is, my friend replied: “Transcranial Magnetic Stimulation, the latest in a long line of crackpot fads to hit psychiatry, designed to separate the worried well from their money.”
When she became increasingly anxious, she was given 12 electroshocks. She had two diagnoses, borderline personality disorder and bipolar affective disorder, and was discharged on these drugs (prn: as needed; bd: twice daily):
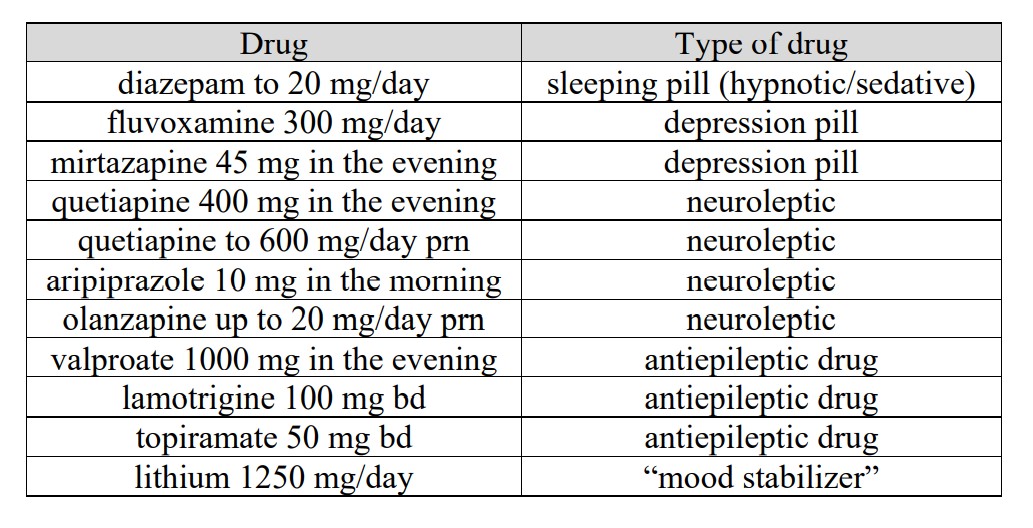
This is insane and constitutes gross medical malpractice. No one in the whole world knows what will happen when all these drugs are given together, only that it is far more dangerous than if fewer drugs are used.
The referral letter notes that the patient sleeps heavily and her appetite is excessive. She is trying to diet, as she has gained about 50 kg with the drugs. She has little energy, interest, or motivation, doesn’t exercise or mix socially, and has no sexual interest. She has bouts of feeling low and miserable with occasional suicidal ideas due to not liking herself, and also has bouts of feeling “manic,” during which she is unpleasantly agitated and tends to overspend in the hope of feeling better.
She also has frequent bouts of agitation and irritability and has described classic akathisia. She has no paranoid ideas and she is ritualistic about security and order but there are no true obsessive-compulsive features. She has been anxious since primary school.
My colleague ended his letter by telling the family doctor that this case was a perfect demonstration of why he had published major objections to mainstream psychiatry. The patient had an anxious personality with secondary depression and did not have borderline personality disorder; apart from this, none of the people using this diagnosis could say what it borders on.
“If she stays on this level of drugs, she will be dead by forty. She is aware of this and wants them reduced but they are all highly addictive and can produce severe withdrawal states, which mimic major mental disorder.”
A court case I have been involved with is no different. It is a typical story that illustrates the role of a depression pill as “Psychiatry’s Starter Kit.”
As far as I can see, this young man should never have been offered a psychiatric drug. He should have been offered psychotherapy for his problems that seemed to be transient. On top of this, he was functioning well when his psychiatrist decided to put him on a depression pill for “depression.”
His psychiatric “career” lasted 33 years before he finally succeeded to come off the last drug, but he still suffers from long-lasting withdrawal effects. His drug list during all these years is mind-blowing. He was prescribed the three main types of psychiatric drugs, sedatives/ hypnotics, depression pills and neuroleptics, on and off in various combinations, amounting to a total of three different sedatives/ hypnotics, five depression pills and six neuroleptics.
He also developed Parkinsonism, very likely drug induced, and was treated also for that. Sedatives/hypnotics were prescribed for about 10 years, depression pills for about 25 years, and neuroleptics for about 30 years, and there was a considerable degree of polypharmacy.
It is remarkable that anyone can survive all this and continue being employed.
The psychiatrist stopped the drugs abruptly many times. Not tapering off slowly these drugs after having put a patient on them for long periods of time constitutes highly dangerous malpractice.
I hope he will win the case, but unfortunately, judges are very authoritarian and always emphasize what other psychiatrists do in similar situations. This is wise, as a general precaution, but not when virtually everyone is at fault. If a bank defrauds its customers, it doesn’t help in court that other banks do the same. Then why is everyone excused in psychiatry? How will it ever be possible to win cases, given this injustice?
Occasionally, a case is won.4 Wendy Dolin in Chicago sued GlaxoSmithKline after her husband, a highly successful lawyer who loved life and had no psychiatric issues, was put on paroxetine because he developed some anxiety regarding work. He got akathisia and threw himself in front of a train six days after starting paroxetine, not realising it wasn’t him that had gone mad; it was the pill that made him mad. Baum & Hedlund in Los Angeles won the case, but then? GlaxoSmithKline appealed the verdict.
When Wendy heard I had arranged a meeting about psychiatry in relation to my book launch in 2015,4 she decided to go to Copenhagen and tell her story. Four other women who had lost a husband, a son, or a daughter to drug-induced suicide when there was absolutely no good reason to prescribe a depression pill also came, on their own account. My programme was already full, but I made room for them. This was the most moving part of the whole day. There was stunning silence while they recounted their stories, which can be seen on YouTube.167
The colossal use of psychiatric drugs is not evidence-based but is driven by commercial pressures. I studied whether two widely differing drug classes, neuroleptics and depression pills, showed similar patterns in long-term usage. The usage patterns ought to be very different because the main indication for neuroleptics, schizophrenia, has traditionally been perceived as a chronic condition whereas the main indication for depressions pills, depression, has been perceived as episodic.
However, they were not different. They were the same:169
Percentage of current users in Denmark who redeemed a prescription for the same or a similar drug in each of the following years after 2006.
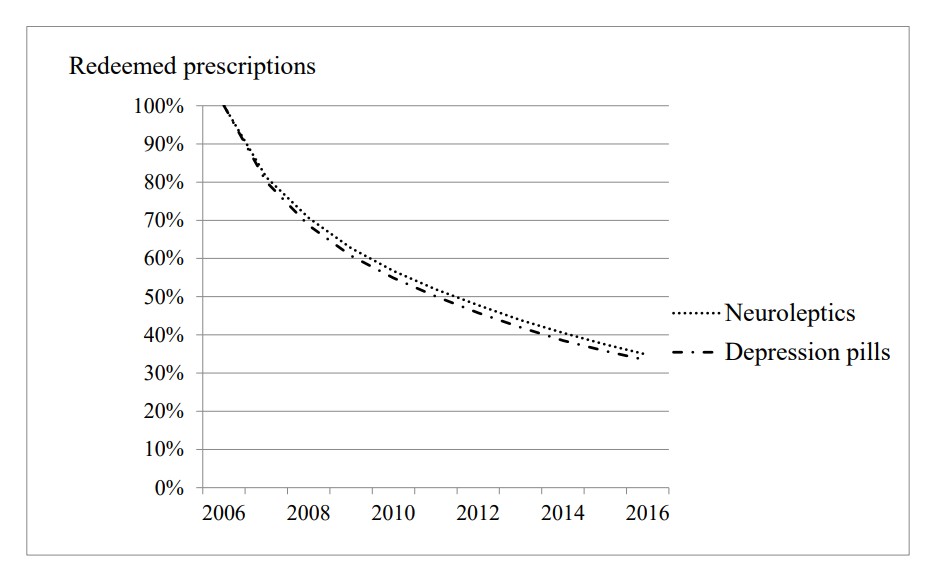
I started the clock in 2006, following patients onwards in time. That year, 2.0% of the Danish population deemed a prescription for a neuroleptic and 7.3% for a depression pill. Many of the patients had already taken their drug for years, but this group of people also included some who were first-time users in 2006, namely 19.8% vs. 20.0%. This was a remarkably similar percentage for two groups of widely different drugs used for widely different disorders.
The patients got a new prescription every single year till they stopped or came to 2016, my last observation year, when 35% vs. 33% of the patients were still on treatment.
These results are shocking. Whatever the flawed guidelines might have tried to tell doctors, they didn’t work as expected, and drug usage was clearly not evidence based. I almost felt I had discovered a new law in nature. Contrary to our hunches, 1 kg of feathers fall with the same speed as 1 kg of lead, provided they fall in a vacuum, according to the law of gravity. Similarly, the usage of these two widely different classes of drugs fell with the same speed. A huge proportion of patients continue taking their drug, year in and year out, for more than a decade.
This is iatrogenic harm of epic proportions. The patients dislike the drugs so much that their doctors need to persuade them to take them. Such persuasion is not needed to motivate people to take baby aspirin after a heart attack to reduce the risk of a new attack. Neuroleptics are even forced upon patients against their will “for their own sake.” If not forced, few would take them.
When healthy people have taken a neuroleptic just to experience what it is like, they have told me, or have published, that they were incapacitated for several days!170 Difficulty reading or concentrating and an inability to work are common harms—but the whole body is affected. We cannot doubt the power of these toxins.
What we are seeing is the result of systematic deception of doctors and patients. The patients are routinely being asked to endure the harms because it may take some time before the drug effect sets in. They are not told that what they perceive as a drug effect is the spontaneous improvement that would have occurred without the drug, or that it can be difficult to come off the drug again. The lie about the chemical imbalance has also contributed. The patients often say that they are afraid of falling ill again if they stop taking their drug because they believe there is something chemically wrong with them.
Mainstream psychiatry doesn’t bother about evidence but will continue business as usual pretending my results don’t exist, and they will say that, “we all know that long-term treatment is good for people; if they don’t get their drugs, they will relapse.”
In 2014, Norwegian psychiatrists wrote about what they called an “alarmingly high discontinuation” rate of neuroleptics in patients with schizophrenia, 74% in 18 months. I would call this a healthy sign, but the psychiatrists argued it highlighted “the clinicians’ need to be equipped with treatment strategies that optimize continuous antipsychotic drug treatment.”171 Really? What about forced feeding with pills, like the Strasbourg geese are fed to produce foie gras? Neuroleptics make people fat. But psychiatrists don’t need to do this. When they don’t get their will, or the patients spit out the tablets, they can use depot injections.
Next, I decided to find out if there was a similar pattern of usage of benzodiazepines and similar agents (hypnotics/sedatives), lithium and stimulants (ADHD drugs).
Since we have known for decades that benzodiazepines and similar drugs are highly addictive and should only be used for up to four weeks (restricted use was recommended already in 1980 in the UK),172,173 and because the therapeutic effect disappears quickly, usage of such drugs ought to be very low, and by far most users in a given year should therefore be first-time users. This was not at all the case:174
Percentage of current users in Denmark who redeemed a prescription for the same or a similar drug in each of the following years after 2007.
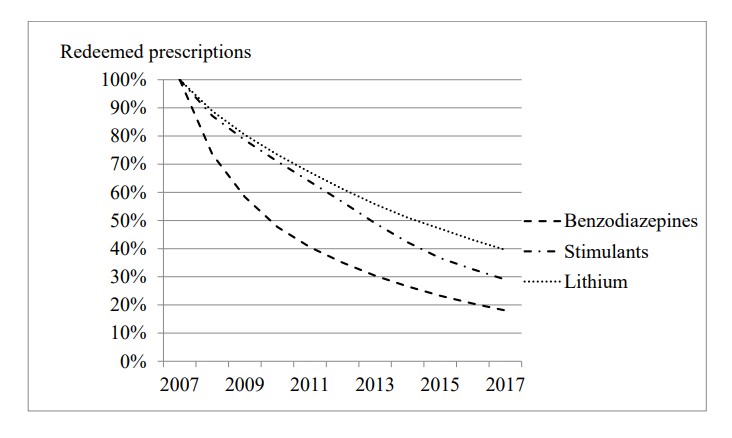
In 2007, 8.8% of the Danish population deemed a prescription for a benzodiazepine or similar agent, 0.24% for lithium and 0.16% for a stimulant. For benzodiazepines, only 13.0% were first-time users. For the two other drugs, the numbers were 40.4% and 11.2%, respectively.
The patients got a new prescription every single year till they stopped or came to 2017, my last observation year, when 18%, 29% and 40%, respectively, were still in treatment.
These findings are also disturbing. No matter which psychiatric drug people take or what their problem is, roughly one-third of the patients are still in treatment with the same drug or a similar one ten years later. For benzodiazepines and similar agents, continued use after ten years was “only” 18%, but given what we know about these drugs, it can be argued it should have been zero many years before 2017. This is a disaster.
The same can be said about the usage for the other four types of drugs, which was very similar as the span only went from 29% to 40% (see the figures).
If we accept the evidence-based premises that these drugs do not have worthwhile effects, particularly when considering their substantial harms, and that the patients generally dislike them, the data show colossal overuse of the drugs to a similar degree.
Psychiatry’s main focus for the next decades should be on helping patients withdraw slowly and safely from the drugs they are on, instead of telling them that they need to stay on them. But it won’t happen. Psychiatry’s focus is on itself—a kind of eternal selfie it sends to the world all the time.
Usage of psychiatric drugs continues to increase markedly in virtually all countries. In the UK, neuroleptic prescriptions increased by 5% per year on average and depression pills increased by 10%, from 1998 to 2010.175
In Denmark, the sales of SSRIs increased from a low level in 1992 almost linearly by a factor of 18, closely related to the number of products on the market that increased by a factor of 16 (r = 0.97, which is an almost perfect correlation).176 This confirms that usage is determined by marketing.
It took almost 30 years after we had the evidence before it became generally accepted that benzodiazepines are addictive.172 This was expected and should have been investigated from the beginning because their forerunners, the barbiturates, are highly addictive. The first barbiturate, barbital, was introduced in 1903, but it took 50 years before it was accepted that barbiturates are addictive.
Benzodiazepine dependence was documented in 1961 and described in the BMJ in 1964. Sixteen years later, the UK Committee on the Review of Medicines published a systematic review of benzodiazepines,173 concluding that the addiction potential was low, estimating that only 28 persons had become dependent from 1960 to 1977. The fact was that millions had become dependent. In 1988, the Medicines Control Agency finally woke up and wrote to doctors about their concerns.172
But the party went on, and history repeated itself. The declining use of benzodiazepines was replaced by a similar increase in the use of depression pills,176 and a lot of what was previously called anxiety and treated with benzodiazepines was now conveniently called depression.5 Drug companies, clinicians and authorities denied for decades that depression pills also make people dependent.172
We did a systematic review of the withdrawal symptoms and found that they were described with similar terms for both benzodiazepines and SSRIs, and were very similar for 37 of 42 identified symptoms.177
Our 2018 study of 39 popular websites from 10 countries was also revealing:32 28 websites warned patients about withdrawal effects, but 22 stated that SSRIs are not addictive; only one stated that the pills can be addictive and warned that people “may get abstinence symptoms.”
Imipramine came on the market in 1957, and a paper from 1971 describes dependence with this drug when it was tested in six healthy volunteers.178 As I wrote on the first page in this book, 78% of 2,003 lay people regarded depression pills as addictive in 1991.179
Thus, we have known for 50 years or more that depression pills are addictive, and the patients have known it for at least 30 years, but 50 years after we knew it, the dependence problem was still being trivialised by the UK Royal College of Psychiatrists and the National Institute for Health and Care Excellence (NICE),180 and in the rest of the world, too.
To read the footnotes for this chapter and others, click here.













“This is insane and constitutes gross medical malpractice. No one in the whole world knows what will happen when all these drugs are given together, only that it is far more dangerous than if fewer drugs are used.”
Actually, all the doctors are taught in med school, that combining either or both the antidepressants and/or antipsychotics, can create “psychosis” or “hallucinations,” via anticholinergic toxidrome.
https://en.wikipedia.org/wiki/Toxidrome
Albeit, I will admit this common medical knowledge is blatantly missing from the psychiatric DSM “bible.” No doubt, because it’s how the unethical, paranoid, dangerous doctors have been covering up their unethical, incompetent husband’s malpractice, et al, for decades. Which is the function of the medically incompetent psychiatric system, who claim to be ignorant of this fact, and likely need to be judged fairly by God.
But I will disagree, “No one in the whole world knows what will happen when all these drugs are given together,” since I know what will happen, thus I’m quite certain God also knows. And I do hope and pray God will judge all the unethical doctors fairly.
Report comment
I like the appropriate comparison to Criminality:-
“….judges are very authoritarian and always emphasize what other psychiatrists do in similar situations…” ” …If a bank defrauds its customers..”
Irelands largest export is Pharmaceuticals. Ireland has also over the years developed a high Suicide/Familicide/Homicide Rate, with the possibility of Akathisia rarely being mentioned.
My own Historical Irish MH Records were fiddled by Doctors at Ireland to hide Akathisia – with Present Day UK doctors attempting to cover this up.
https://drive.google.com/file/d/1vYO9r1FkdJSv8Bi8Q3c3u9WXNZXkmxvO/view?usp=drivesdk
Present Day UK doctors were attempting to promote the Historical Irish MH Records as Legitimate – while at the same time attempting to cover up the Dr Shipman Type Medical Fraud from Ireland.
Report comment
I would imagine that a proportion of Akathisia deaths with genuine investigation would be reclassified as (medical) murder.
…just like a Restauranteur that kills a diner by guaranteeing the diner the absence of ingredients they are highly allergic too – knowing full well that the diner might be easily exposed to these ingredients.
Report comment
But if it’s acceptable practise for doctors to ‘Cover Akathisia Up’ in a patients records – then this would explain the mystery increase in Suicide/Familicide/Homicide at Ireland.
(…and why the Irish Medical Council avoided the subject when I brought it up with them).
Report comment
Delusional is an accurate description, but I think that describing many psychiatrists as being in a cult is accurate as well. They have an unhealthy devotion to pharma. Dr. Gotzsche understands the enormity of the problem. Unfortunately medicine does not. If the patients knew that there is no scientific data supporting the use of these medications, much less the use of half a dozen at a time, they would be livid. Especially as they spiral into worse and worse health. Reading Dr. Gotzsche’s thoughtful work would be enough to influence most anyone, except cult members who have given up on reason and critical thought.
Report comment
Margaret Singer has several main characteristics of cult indoctrination.
-Keep members ignorant about what is going on with aid from a behavioral change program designed to get them to commit more to the cult. First it’s therapy then 1 drug then 2 then 3, then a “hospitalization”.
-A sense of powerlessness is installed (essentially the result of all psych labels and proclamations that people are ill and sick for life)
-dependency is formed and the environment is controlled (for psych this extends to literal drug addiction, and “hospitalized camps”)
-Manipulation and a system of rewards and punishments that change people’s social identity.
-Create a closed system of thinking impervious to criticism, logic or evidence. Dissent from the cult is punished and discouraged (patients are slandered as “lacking insight” forcibly drugged/jailed, psychiatrists get fired if they dissent)
-The cult members blindly follow leaders who have inherently higher status than the other members.
If this were a psychiatry “diagnosis” 4 out of 6 of these traits are needed to be diagnosed as a cult. The treatment would be large amounts of cognitive impairing deadly sedating drugs. Forced if need be.
Report comment
“….- Create a closed system of thinking impervious to criticism, logic or evidence….”
This one resonates with me!
Report comment
Absolutely it is a cult. It is easy to snag the students. I doubt they even need to use the word “science”, in order to snag potential students.
It’s a personality driven occupation, appealing to people for a variety of reasons and or pressures to do something.
And it’s great if we can make a business out of people’s hardships, milk them for all it’s worth. Drain them of whatever potential was there.
It is a really self centered business, and has zero to do with true wellbeing for others. Not for the shrinks either.
Report comment
The psych students would be high status members of the cult. If they don’t recognize the professional does nothing but hurt people before spreading the cult they’ve already lied and caused massive harm. Most don’t have the courage to admit it so they go on in denial pretending they are saviors. This is pretty easy since almost all of society agrees with the cult, and lavishes high status members with wealth and power. Speaking out against cult dogma results in retaliation which is further deterrence.
It also resembles how gangs initiate new members by having them commit a crime. Psych does this with family and friends by telling them to coerce people on drugs. A family member who has done this has to either stay in denial or admit they hurt their loved ones.
People directly harmed by psych have the same pressures. They can accept they were conned into hurting themselves and then suffer withdrawal, further stigmatization and harassment for quitting the cult or they can maintain denial.
Report comment
This is crazy!
Report comment
I hope I’m not wandering too far away from the subject:
“…There is no reliable evidence that the psychosis per se can damage the brain…”
I notice the heavy use of Anti Epileptic drugs is mentioned in this article. Are these drugs damaging to the brain?
Report comment
Thanks Peter, love your writing and taking the time to educate.
Medical doctors could not honestly ever believe in psychiatry, no true believer in health could ever promote such harmful practice. Harmful first to the psyche and harmful and deadly practices.
No doctor can now die and say that he or she did no harm, especially not knowingly.
You would have to be an idiot to not see, especially if one is in the industry of health. More and more it looks like an industry of power.
Report comment
My 40 yr old brother died undergoing psychiatric ‘care’ and no explanation ever provided. His death was totally unexpected and disturbing but I naively believed it must have been an ‘unusual’ occurrence. I didn’t realize how dangerous and corrupt psychiatry was until I was ambushed by a psychiatrist I saw for “help with sleep meds” for chemo-induced insomnia.
“Psychiatry’s focus is on itself—a kind of eternal selfie it sends to the world all the time.”
Yes, this is why the lies and damage continues – psychiatry only cares about itself. They keep labelling people with crafted, absurd labels in order to push toxic pills because it’s all they’ve got. Psychiatry has made it quite clear it’s not about helping people, it’s all about retaining careers, reputation, ego and big salaries.
When you look behind the curtain you realize psychiatry is the epitome of harm. I really hope more people start suing and winning. Some justice is long overdue.
Thank you Dr. Gotzsche for your outstanding efforts to expose the corruption and to enlighten and protect people.
Report comment
It is insidious. They lie that their victims are ill and then give them drugs that cause illnesses. The drug induced illnesses are then blamed on the victim. When I’m with people taking psych drugs who complain about their physical or mental health it elicits this weird emotion. I know the cause and fix for their diabetes, heart disease, cognitive decline, and inability to be happy and so on but they refuse to even look at the evidence and research. Psychiatry told them they can only listen to psychiatry and that they are too “mentally defective” to understand research.
Report comment
My research shows that the neuroleptics were from the beginning a chemical lobotomy, which worked the same as the previous surgical lobotomy (the one for which Egas Moniz received the Nobel Prize) but had fewer side effects, so they replaced the surgical lobotomy with neuroleptics. The idea was to restrain the dangerous madman, and that was all. All the rest of the “help and treatment” envelope is a false envelope, the aim of which was to raise the status of psychiatry, the profits of pharmaceutical companies, and perhaps also the political propaganda of governments that prefer to argue that their laws on compulsory psychiatric practices lead to helping people, and not simply to tame dangerous individuals like you do with criminals.
Report comment
Other terms defined by examples of doing the same thing over and over again while expecting a different result could also be stupidity or foolishness, or more kindly, to ignorance or unconsciousness….not madness (or insanity). Then again, rare (but many!) individuals have won lotteries or the $100,000 slot machines. This definition (or cliche) has been used to sum-up and describe ‘madness’, but there’s no need to use this convention to reinforce the stereotype just to simply return the label onto ‘psychiatry’, regardless of the ultimate point….and with ‘delusional’ as a cherry on top. The ad hoc diagnostic (of a professor with an MD?) flipping the muddled diagnoses and leaving no sign of irony, self-doubt, or self-criticism. It’s not clear to me that this benefits ‘patients’ any more than ‘psychiatrists’.
Someday I expect the author to mention something about nutrient supplements. Whether or not it’s in any way positive, I’m not sure.
Report comment
Don’t get me wrong, although ‘practice (can) make perfect’, this is not what most psychiatric prescribers (psychiatrists/physicians) are doing. F€#* that s$@£!!! Trial and error has its place, but hardly ever in a desert where most oases are mirages.
Report comment
Peter, click on my name Diaphanous Weeping for something I said over in the MIA article…
“My Letter to An Advocate for Voluntary Treatment” by Emily Hochman.
Since it has relevance for what you are outlining in your great work.
Report comment