 In this blog, I want to give some personal reflections on the events of the last few weeks in relation to the Lancet antidepressant meta-analysis and the lodging of a formal complaint with the UK Royal College of Psychiatrists.
In this blog, I want to give some personal reflections on the events of the last few weeks in relation to the Lancet antidepressant meta-analysis and the lodging of a formal complaint with the UK Royal College of Psychiatrists.
In the interests of full disclosure, I am a signatory to the letter of complaint, so if you are seeking a view from a neutral party, you will want to look elsewhere. This blog is also my personal view and not meant to represent the views of the other signatories.
What’s been happening?
The fun began on February 21st when the Lancet reported the results of a meta-analysis of 522 placebo-controlled trials of antidepressant drugs. In short measure, as Auntie Psychiatry and others have pointed out, the UK media largely recreated a press release written by the Science Media Centre. Respected papers like The Times and The Guardian proved that journalism now means merely reading a press release, not actually taking the time to read the study itself and reach a balanced conclusion about the results which, at best, were modest and confirmed what we already knew from the work of Irving Kirsch and others a decade ago.
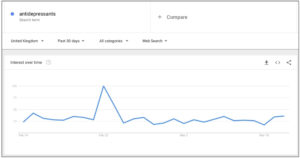
On February 22nd, the word ‘antidepressants’ had its highest ever number of Google web searches in the UK.
Also on the 22nd, The Mental Elf, a popular mental health and psychiatry blog in the UK (with the mantra “No Bias, No Misinformation, No Spin”), said this about the Cipriani meta-analysis:
“It’s been a rough few months for people taking antidepressants. We’ve been bombarded with information that insists our medication is ineffective and harmful, that any benefit we gain from taking these pills is simply a placebo effect, and that by accepting a prescription of antidepressants we are joining an ever-growing zombified mass of morons.”
Elsewhere, the good news story about antidepressant efficacy that ‘put to bed’ the debate continued to be reported far and wide.
In response on February 23rd, Dr James Davies, Dr Joanna Moncrieff, Professor John Read and others pointed out this lack of critical appraisal and the problems with the study itself. Dr James Davies appeared on BBC Newsnight and Dr Joanna Moncreiff appeared on Channel 4 news. Letters appeared in the Guardian newspaper along with critical responses from Professor Peter Gøtzsche and Professor Peter Kinderman amongst others. In addition, social media was alight, with the hashtags #MedsWorkedForMe and #MedsDontWorkForMe doing battle.
A few of us even directly engaged the current President of the Royal College, Professor Wendy Burn, an exchange which Bobby Fiddaman covered in his excellent blog. Some of us, probably naively, felt that we had made a good account of ourselves in the face of the massive media hype.
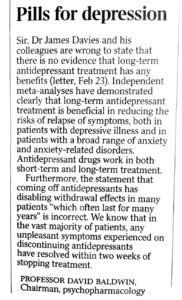
It was what happened next that made things interesting. In an attempt to refute critical comments, Professor David Baldwin, Head of the Royal College’s Psychopharmacology Committee, wrote a letter to The Times on February 24th. In the letter, he said:
“Furthermore, the statement that coming off antidepressants has disabling withdrawal effects in many patients ‘which often last for many years’ is incorrect. We know that in the vast majority of our patients, any unpleasant symptoms experienced on discontinuing antidepressants have resolved within two weeks of stopping treatment.”
I can only imagine how this statement was received at the Council for Evidence-Based Psychiatry, which has been at the forefront of work to educate and inform about the many issues with psychiatric drugs. By February 28th, nine professionals, spearheaded by Professor John Read of the University of East London, had written to Professors Burn and Baldwin, to request a public retraction of the statement or the provision of the evidence in support of it.
As detailed elsewhere, Professors Burn and Baldwin responded directly to John Read, responses which, charitably, we could probably best label as ‘not helpful’ with their main argument seeming to be that the complaint letter was “a bit harsh.” Following this reply, John and members of CEP amplified upon the original complaint, providing evidence in support of the view that antidepressant withdrawal was a significant issue for many people. The letter was signed by thirty academics, psychiatrists and those with lived experience. John Read then personally hand-delivered this second letter to the Royal College’s offices in Central London on March 9th.
Since then, there has been a smattering of media interest with John Read facing Doctor Clare Gerada (wife of Sir Simon Wessely) on BBC Radio 4’s Today programme. The issue was then given a more balanced assessment on BBC Radio 4’s Inside Health programme. Scottish newspaper The Herald has been a staunch supporter providing good coverage. It is fair to say that the media response to our complaint has been muted and disappointing, in stark contrast to the near hysteria that greeted the Cipriani study and its attendant SMC press release.
On social media, particularly Twitter, there has been an interesting mix of reactions. If you are affected by withdrawal from psychiatric drugs, it is very easy to feel isolated and marginalised, and not uncommon to have your experiences refuted, denied and flat-out contradicted by doctors and psychiatrists. In recent times, there have been accusations of ‘pill shaming’ directed at anyone bold enough to share their difficulties and struggles. The origin of the hashtag #pillshaming is interesting in its own right.
This pill shaming defence has been adopted by some psychiatrists, alongside trying to reduce almost every conversation about the drugs to “they help people” or “they save lives” but with little to no evidence ever provided in support of these claims. Sir Simon Wessely, former president of the Royal College of Psychiatrists, tweeted after the BBC Radio 4 exchange between Professor Read and Doctor Gerada:
“Oh dear. Time for another round of #pillshaming. #r4today @BBCRadio4. Antidepressants are not addictive. There is no tolerance, escalation etc etc.”
That brings us up to date. What happens next will be very interesting. Will it be a ‘strongly worded letter to The Times’? Will it be a veritable feast of studies that confirm that the ‘vast majority’ are over their difficulties in two weeks? Will it be a public debate? Whatever happens, we will keep you updated on progress.
What can you do?
I feel that we need your input — we need to capture experiences and we need to know the cold, hard truths that people struggling with antidepressant withdrawal face each and every day. Firstly, please comment on and discuss this blog, either share your own experiences or perhaps make suggestions for promotion of the complaint and the lived experience input. If you are connected with the media, please draw their attention to the complaint. If you would like to share your experiences with me personally, rather than in the comments below, please email me.

On Twitter, we didn’t want to feel left out of the ‘bring a hashtag’ party, so we have created our own. People are sharing their experience of antidepressant withdrawal using the hashtag #MoreThan2Weeks. Please share your own experience or what you have witnessed family or friends deal with. This particular hashtag has generated over 1,000 tweets in less than 48 hours, please join in if you can.
If you have personally experienced withdrawal effects, share those experiences with the MHRA in the UK or with the FDA in the US. Psychiatrists often claim that there is no evidence of protracted withdrawal, so let’s give them some.
For many of the old guard of psychiatry, who are so wedded to pharmacological intervention, pointing out the limitations and dangers inherent in psychiatric overprescribing is tantamount to an existential threat. A threat to which psychiatry is quite keen to respond — but rarely, it seems, with sound, evidence-based fact. This complaint gives us a focal point for a critical mass of us with lived experience to recount the reality and extent of antidepressant withdrawal.
Finally, I want to thank everyone who has been involved with this complaint, whether signing the letter, sharing their difficulties on social media, asking difficult questions of their doctors or even reading this blog. The recent attention has brought the issue of antidepressant withdrawal into the public eye in the UK like never before — perhaps we can start a similar discussion in the US and elsewhere too.
[Note: for those outside the UK, the media links for BBC Newsnight and Channel 4 News might not work correctly.]















What’s happened is that the Science Media Centre have let fly an absolute broadside of hype which people are starting to see as frankly loopy. But the furore has certainly provided the incentive for ordinary people like me to dig deep and become better informed, and I for one will never be fooled again. I think people just need to understand the extremely weak effect size – it should be on the patient information leaflet actually. Also, you must have seen that even one of the authors John Ioannidis is much more measured : “I am afraid that some news stories gave very crude interpretations that may be misleading, especially when their titles were too absolute, like ‘the drugs work’, ‘the debate is over’ and so forth,” he said. “The clinical (as opposed to statistical) significance of the treatment effects that we detected will continue to be contested”. So, glass half full – a massive meta-analysis verifying Kirsch’s work, and some unhinged statements from biological psychiatrists that can’t stand up to scrutiny.
Report comment
Hi James,
Thanks for everything you are doing. The same debate is happening here down under. less than 5 days after I read the Guardian’s story our “The Press” had the headline “Antidepressants don’t work” following a presentation by Peter Gotzsche and Robert Whitaker, and others, in Christchurch New Zealand I cringed when I saw it and thought loudly “it’s not as simple as that”
Psychiatry continues to use divide and conquer as it’s tactic. But social media is better than “the News” and we know this. I do find it a little sad as it polarizes those who have had good experiences and bad. But I see iatrogenic harm everyday and it makes me cry and unable to do my job sometimes. I am an occupational Therapist who has become a peer leader for our region. When I’m awake in the middle of the night I comment on the UK FB group “Drop the Disorder” and I’ve done that a bit this week as we have lost another beautiful young man in our community to suicide this week (another victim of psychiatry I believe)
I will continue to follow the debate with great gusto (and I must remember this hashtag thingie) BIG psychiatry has cost me over $140,000 in lost income 🙁
Report comment
I have had a good experience with Zoloft. It brought me out of my depression. But the benefits were short term. My life was no better. My family treated me poorly–in a way they never did till my shrink told them I was hopelessly insane.
The reason I get angry when people insist these things work is this hurts “consumers” when they aren’t magically transformed into walking smiley faces from pill popping.
They talk about “pill shaming.” How about patient shaming?
You take the drugs religiously–exactly as prescribed. But your depression continues. Or it worsens. Or you become floridly psychotic.
Your parents or partner run to your shrink in desperation. He smiles, and (I assume) lies through his teeth. “The meds have been overwhelmingly proven to be safe and effective. Obviously your child/partner isn’t taking them exactly as prescribed or everything would be fine.”
They accuse you of “non compliance” despite your tearful protestations. When you complain they aren’t working they laugh at you.
Your therapist either accuses you of “non compliance” too, or says you just aren’t working hard enough. Since the drugs have thoroughly straightened out your thought processes you have NO EXCUSE to keep making bad choices–like lying in bed half the day from drug-induced fatigue.
Actually doing something to help the “crazy”–little stuff like words of encouragement, letting them know you still love and accept them, helping them financially since they’re forced to live in crushing poverty–these are totally unnecessary.
All the supporters of psychiatry I know are cold, unloving, and selfish. If they cram pills down your throat they can throw you on the scrap heap and go on their merry way. Their conscience is totally appeased. “I made her take her ‘meds.’ That’s all that’s needed.”
Let her rot. If she commits suicide, who cares? It’s nobody’s fault after all.
Report comment
The term “antidepressant” is a misnomer, and a euphemism for a dangerous, neurotoxic drug. Those who have been drugged and poisoned with these neurotoxins are most often unaware of their predicament. Those who have been fortunate enough to survive drugging often experience the effects of extreme iatrogenic harm. If such survivors are well enough to tell their sad tale, their stories are often appropriated and misused by psychiatrists or even psychiatric reformers. Psychiatry is a system of slavery and coercion. The neurotoxic drugs that are euphemistically referred to as “medication” are worse than physical chains. They rob innocent human beings of their powers of reason and create legions of docile, chemically lobotomized, suffering slaves. The chiefs of pharmaceutical companies that produce and market these neurotoxins are guilty of manslaughter many times over, and must be held accountable for their crimes. The psychiatrists who peddle these neurotoxins know not what they do. If they do know, they are just as guilty as the manufacturers of these thanatophoric, or death inducing drugs. The blood of the innocent cries out from the ground against psychiatry and the pharmaceutical industry. God’s justice cannot sleep forever. Slay the Dragon of Psychiatry.
Report comment
A question I bet no one has been allowed to ask publicly. How many people has James Baldwin helped taper off SSRIs?
None of the shrinks I know ever did that. They told me I was stuck taking drugs till I died. No wonder I wanted to die.
Another thing. Who runs the Mental Elf? My guess is it’s probably psychiatric professionals and/or “concerned loved” ones with one or two token SMI’s to laud the “life-saving medications.”
Report comment
Love the title to this post. One could say the Prozac, now Xanax, Generation comes of age, and starts shooting up the place.
Report comment
I was put on an antidepressant initially on 6/29/2000. It did not work for smoking cessation, which is for what it was prescribed, so I was abruptly taken off of it by my PCP after about a month. I suffered from the typical flu-like withdrawal symptoms first, these were misdiagnosed as things like the “flu” and “pneumonia,” resulting in mistreatment with other drugs.
Oddly, it wasn’t until after 9/2001 that I started getting the really bizarre antidepressant withdrawal symptoms, like powerful dreams, nightmares, brain zaps, odd sexual side effects, and mild confusion. But I was dealing with a “confusing” interpersonal situation at that time, although our entire country was dealing with a strange and “confusing” situation in 9/2001 also.
These common symptoms of antidepressant discontinuation syndrome were misdiagnosed as “bipolar,” despite this being a blatant misdiagnosis, according to the DSM itself. We all know what kind of massive poisoning fest that misdiagnosis leads to, thankfully I escaped the lunacy fest of the mental health system for the most part in 2005, and completely by 2009. I do still have the brain zaps, but I’ve learned to live with them and control them.
Bottom line is there is definitely a problem with tardive and protracted antidepressant discontinuation symptoms. Oh, by the way, the FDA link doesn’t work.
Report comment
You can’t distinguish very well between biological explanations, nurture/environments events and attitudes that implant fatigue.
Point two is maybe the rise in individuals that have depression is from the ECOLOGICAL aspect. Meaning the how living organisms relate to one another and surroundings on mass scale.
Where we were decades ago is like the ice age when you look at where we are now pertaining to involvement and community dynamics. For better or worse is this portrayal with community. To be undone this community framework now and move forward better is ideal. See Wikipedia ecology page https://en.m.wikipedia.org/wiki/Ecology
May need to cipher these unique distinctions out within your own mind frame and make an informed decision.
Report comment
Thanks, all of you for taking the time to read and to comment. Campaigning on this, as you can imagine, I get many messages that are deeply troubling and show the impact of this on lives, on families, on careers. This isn’t a problem restricted to drugs for depression, of course, it is common to all classes of psychiatric drug. Unfortunately, ‘antidepressants’ are the visible tip of the iceberg. In the UK, they are the poster child, vaunted as the psychiatric success story in the media. UK Prescribing figures have just been released by our National Health Service, in 2017, we prescribed 67.5 million antidepressants, costing our health services £255 million. That is for a population of 53 million people. In 2007, the figure was 33 million, we have more than doubled prescriptions in a decade and the media response recently has just fuelled that shocking rise. I am so glad that more people are coming forward to tell their stories and share the reality of this and grateful to you all and Mad in America for shouting from the rooftops.
Report comment
No problem. Good reply comment.
So this may sound implausible, however often some good ciphering is the way. What’s that you may wonder? Aww well that’s when you spend a night or two by yourself on the back deck or while hiking and quietly determine whether have biological reason, nurture/environmental cause or an attitude dilemma.
These distinctions are scarcely defined to having depression but center on spectrum of mental health challenges.
This is not insensitive although I’ve been ingrained to feel that having recovery journey that involves hospitalizations is one way to think about these distinctions. Often if road has been formed out of pleasure and chisled by pain it may be due to attitude dilemma. Third an environmental stressor leaves no words but to each his own.
Report comment
The antidepressant Cymbalta (duloxetine) has been a real bitch for me to get off of. Even doing a slow taper since June 10th of last year, I’ve experienced withdrawal symptoms. Such as a crippling headache that would disappear after I took a pill! Thanks for the reminder to report it to the FDA. Such a shame that the American Medical Association has not followed suit with the article in the French medical Journal that put Cymbalta on its “do not prescribe list” and recommends that doctors don’t prescribe it. All those lawsuits about Cymbalta and the AMA has no comment. I wish I had never started taking it. For every five years a person has been taking Cymbalta, it takes an average of a year to get off and that doesn’t eliminate withdrawal symptoms, it just reduces their severity.
Report comment
I’ve heard cymbalta is an absolute bitch to get off of. Hang in there. I had about 5 years slow taper off paxil, with terrible withdrawal, and then 2 years of brain zaps and mood problems. I feel pretty normal finally though. You can do it!
Report comment
Groan! My mom’s on that crap. She says she needs it because her nerves get bad when she goes off.
Risky as it is I am “coming out” as non-compliant in August. Too many loved ones are on these poisons. If they see my improvement maybe they’ll realize they’re trapped in “The Matrix.”
Report comment
I tapered myself off of anti-depressants and mood stabilizers 13 months ago. I still am having lots of issues including: tiredness/lethargy, vision changes, stomach/bowel issues, and a persistent “hangover” effect/fog-headedness. I was on these drugs for 29 years.
If I knew then what I know now I would have never gone on them at all. However, I don’t have a time machine and cannot change the past, as much as I might want to.
I’m not sure if there is anything that can be done or if I am permanently screwed. Aside from the usual eat right/exercise information there doesn’t seem to be much out there and my Psychiatrist can give me no help. There is some information about the tapering but not so much for what follows. It’s been 13 months! Am I going to be like this forever?
Report comment