A recent observational study that looked at what happened to people following a first admission for schizophrenia concluded that discontinuing antipsychotic treatment is associated with higher risks of death and rehospitalisation (Tiihonen et al., 20181). This is the latest paper by a group of Finnish researchers who specialise in complex analysis of data from population registers and, contrary to many other data, always find that long-term drug treatment is good for your health. They have extensive links with pharmaceutical companies that make antipsychotics.
The latest study uses the Finnish population registers which record deaths and episodes of hospitalisation and a prescription register for data on antipsychotic prescriptions. The main outcome was a variable that was called ‘treatment failure’ which consisted of a combination of rehospitalisation and death. The use of a combined measure is a bit curious, since death and readmission are likely to show different patterns of occurrence and different associations. Another curious feature is that people who discontinued antipsychotics in the first 30 days following discharge from hospital were excluded from the analysis, without any apparent justification.
The study has a large sample, and I presume that the registers used are comprehensive so that follow-up would be pretty complete. The reliability of the data on use of antipsychotics has been questioned in the past, however (De Hert et al., 20102). The authors point out the limitations of randomised controlled trials in collecting long-term follow-up data and offer their study as a contribution that can help fill this gap. However, there are a number of well-recognised problems with this sort of study and we should be very cautious about accepting its conclusions at face value.
The main problem is that it is an ‘observational’ study and not a randomised controlled trial. An observational study is when you look at the outcomes of people who have a condition and are given treatment in the usual way. You don’t actively intervene as you would in a randomised trial to ensure that the people who have the treatment are roughly the same as those who don’t. Observational studies of this sort can give results that are in completely the opposite direction from those obtained in randomised controlled trials. This happened in the case of the heart failure drug, spironolactone, for example. A landmark randomised controlled trial found that spironolactone reduces the risk of death by about 30%, but a carefully matched analysis of observational data incorrectly found that it increased the risk of death by about 30% (Freemantle et al., 20133).
Authors of observational studies are aware that people who take medicine are likely to differ in important ways from those who do not (or indeed those who discontinue early, the focus of the Finnish study) and that these differences may be related to the outcome of interest and may not be captured in statistical adjustments during analysis. For example, people who are prescribed spironolactone may be older or younger, and may be more or less sick, than those who are not. For this reason, authors of observational studies usually go to great lengths to match users and non-users carefully on a whole variety of factors, both demographic and health-related. They may construct ‘propensity scores’ that combine a number of variables that predict exposure to the treatment of interest, and match people who are and are not treated according to these scores. This is what the authors of the spironolactone analysis did. However, in the present study, people were matched only on the length of time they had been taking antipsychotics. Age and sex were controlled in the subsequent analysis, but there does not appear to have been any attempt to control for the numerous other factors that may influence outcomes like death and readmission. In a previous analysis of mortality by the same group, the following variables were controlled in some way: age, sex, illness duration, previous hospital treatment for attempted suicide, schizophrenia diagnosis, cancer and ischaemic heart disease (Tiihonen et al., 20094). The authors were still criticised for not including variables that might have important effects on mortality such as socio-economic status, substance misuse, indicators of unhealthy lifestyle and detailed cardiovascular risk factors (De Hert, Correll, & Cohen, 2010). Symptom severity, functional status, social support, use of other medication and numerous other factors may also affect the chances of dying prematurely or being readmitted to hospital. Yet, in the present study, there was no effort to match patients on any potential risk factors. The authors reasoned that duration of antipsychotic treatment is a proxy measure of severity, but this seems unlikely since they were only looking at duration of treatment subsequent to the first hospitalisation. Therefore the matching conducted in this study is unlikely to have resulted in groups with similar levels of underlying risk factors for the outcomes of interest.
However carefully you match people, though, the real problem with observational studies is that there are likely to be residual differences between people who take the drug and those who do not, which may be related to outcome. In the analysis of spironolactone treatment, despite the most sophisticated attempt at matching, the results were still completely at variance with those obtained in randomised controlled trials.
These differences occur because the decision about who continues and who discontinues treatment in observational studies is not random. It is a decision made by patients or clinicians that is likely to be related to other factors that predict outcome. For example, we know that people who are compliant with any treatment, including placebo, have better outcomes than those who are not across a range of conditions. In the Women’s Health Initiative, for example, women who showed high compliance with placebo had lower rates of hip fractures, heart attacks, cancer death and death from all causes compared to those who showed poor compliance (Curtis et al., 20115). It seems that people who stick to recommended treatment have other features that mean that they do well. They may be more physically or mentally healthy to begin with, more likely to engage with other aspects of treatment and they may have more social support. Conversely, people who stop medication may be more ill to begin with, at higher risk of neglecting their health in other ways and they may have a more chaotic lifestyle and less social support. We don’t know what unknown factors are influencing outcome, and we are unlikely to be able to identify and measure everything that is relevant.
Clinicians’ decisions to prescribe or to stop medication are also not random. In particular, clinicians may avoid prescribing a drug with known physical complications in someone who already has risk factors for developing those complications. They may not prescribe olanzapine to someone who already has diabetes, for example. Therefore if you look at data from routine clinical care, you may find, contrary to the pharmacological evidence, that olanzapine is less likely to be associated with diabetes than other drugs. Similarly, when someone is seriously physically ill, clinicians may decide to stop some medication. Since antipsychotics are known to be cardio-toxic, clinicians may decide to these drugs if someone develops heart disease, for example.
Not knowing the causes of death in the present study makes the figures even more difficult to interpret. The figures that are presented in the supplemental information suggest that people who had never used antipsychotics since discharge from hospital had the highest number of deaths, followed by those who discontinued antipsychotics within one year, but those who discontinued antipsychotics after longer periods did not show higher rates of death compared with those who continued antipsychotics, although numbers of deaths for these groups were small. Deaths that occurred after hospitalisation (which may include admission to a general hospital) would also not be recorded in this data, however, which may therefore underestimate the risk of death in general.
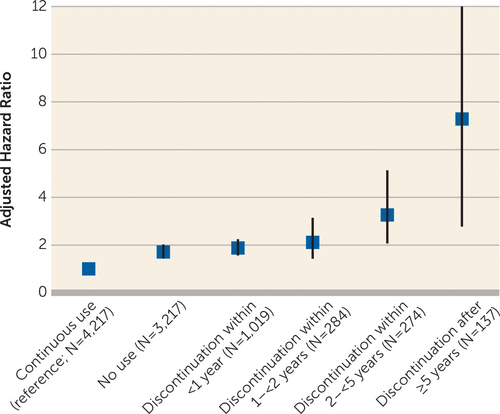
In the unmatched comparison (no matched group is provided for this comparison), the risk of rehospitalisation was only slightly higher among non-users compared with continuous users of antipsychotic medication (HR 1.24 CI 1.18 to 1.30). In the comparison of ‘matched’ groups of continuous users and discontinuers, the risk of rehospitalisation increases with longer duration of treatment prior to discontinuation (see Figure).
Figure
However, the analysis is what is known as a ‘survival’ or ‘time to event’ analysis. The numbers and proportions of people rehospitalised were in fact comparable between continuous users and discontinuers, but length of follow-up was shorter. Follow-up ended at the time of rehospitalisation (or when people switched antipsychotic status — i.e. when discontinuers started using antipsychotics again, or when users stopped taking them), which suggests that readmissions occurred earlier in people who had discontinued antipsychotics, but not necessarily more commonly. This finding is consistent with other evidence showing that stopping antipsychotics brings forward your risk of relapse, but may not influence it in the long-run. This was demonstrated in the Wunderink study of people with first episode psychosis (Wunderink et al., 20136).
The focus on short-term events also explains the discrepancy between the present study and the findings of Martin Harrow’s study, which suggested that people who avoid long-term continuous treatment have better outcomes, including lower rates of relapse and higher levels of functioning and recovery, compared to continuous users (Harrow et al., 20127). The Harrow et al study was also an observational study, of course, and is therefore open to the biases that arise because treatment is not randomly allocated. It is possible that the results of the Harrow et al study are explained by an association between taking long-term treatment and having a worse prognosis, for example.
Another explanation is the different lengths of follow-up. Although the Finnish study presents itself as a 20-year follow-up, this is the maximum duration, and most people were only followed up for just over a year at most. People who did not use antipsychotics at all had the longest median duration of follow-up at 408 days, continuous users were followed up for a median of 376 days, and people who discontinued antipsychotics were only followed up for a median of between 122 and 134 days (i.e. just over four months). The benefits that non-users of antipsychotics show in the Harrow et al study start to become apparent at the four-year follow-up point. So, unlike the Harrow et al study that followed everyone up for 20 years, the present study is not telling us anything about the long-term outcome of people taking antipsychotics. It may be telling us that people are more likely to relapse in the immediate period after stopping antipsychotics, although given the caveats about observational studies, we should be cautious about even going this far. But it certainly does not tell us what happens over 20 years, as it advertises itself as doing.
So what should we make of this latest offering overall? First, because it is not a randomised trial, it does not provide convincing or conclusive evidence that stopping antipsychotic medication causes rehospitalisation or death. People stop antipsychotics for all sorts of reasons and in all sorts of circumstances that may be related to rehospitalisation or death quite independently of their use or non-use of antipsychotics.
Second, this is not a study of a controlled and gradual reduction of antipsychotics with the support of professionals. Some instances of discontinuation may have been of this sort, but most are likely to have been unsupported discontinuations done without the clinical team’s knowledge, and some may have been discontinuations prompted by physical illness.
We need evidence from randomised controlled trials, such as the Wunderink study (Wunderink, Nieboer, Wiersma, Sytema, & Nienhuis, 2013), and the ongoing RADAR trial, to show whether a gradual and supported reduction and discontinuation of antipsychotic treatment increases rates of rehospitalisation, and if so by how much. Only a trial in which the decision to continue or discontinue treatment is randomly assigned can avoid the biases inherent in analysis of observational data and provide a reliable answer.















That’s offensive plain and simple.
Report comment
Which is offensive Pat? The study and its conclusions or Dr. Joanna’s critique of it?
Report comment
“First, because it is not a randomised trial, it does not provide convincing or conclusive evidence that stopping antipsychotic medication causes rehospitalisation or death. People stop antipsychotics for all sorts of reasons and in all sorts of circumstances that may be related to rehospitalisation or death quite independently of their use or non-use of antipsychotics.
Second, this is not a study of a controlled and gradual reduction of antipsychotics with the support of professionals. Some instances of discontinuation may have been of this sort, but most are likely to have been unsupported discontinuations done without the clinical team’s knowledge, and some may have been discontinuations prompted by physical illness.”
That is it.
And we need to move on from this to abolishing psychiartry. If you take the drugs and are forced to do so three four five of them at a time ala polypharmacy: benzos, antipsychotics, sleepers, SSRI’s you will really know why and realise the studies are bullshit for people to talk bollocks over while the victims rot in horrendous hell on these neurotoxins.
We see a different value through the filter of change over time and realise either something good and very bad has occurred. History will show psychiatrists harmed and killed a hell of a lot of people and got away with it. This has started with legal cases and will continue with pharmacogenetics and skilled research use of the internet and platforms to show the public. We will project to the future and dismantle .
Report comment
Researchers with “extensive links to Pharma companies that make antipsychotics” pretty much explains their “conclusions”.
Report comment
Two other important biases can be cited.
Due to the immense social pressures to continue taking neuroleptics, some patients may continue to buy the drugs without consuming them.
In the Vermont study, in-depth interviews revealed that two-thirds of patients who were reported to have regular medication were lying.
Still due to social pressures to continue taking neuroleptics, some patients are readmitted to hospital when their family or psychiatrist discovers they have stopped their treatment, even if they do not relapse.
This is a common measure in France.
See my comment on the other publication.
Report comment
To ensure that they do take their “medication” people are often injected with recordable Long Acting Drugs like Modecate (Fluphenazine Decoanate) – which I describe (below).
Report comment
My solution? Withdraw carefully by tapering and hiding out. If necessary fake an illness like FM or Chronic Fatigue Syndrome. You will probably be very sick for a while.
And tell nobody!
I took vitamins at pill times to psych my folks out. To this day they don’t know. And they don’t know why I’m suddenly doing better either.
Report comment
Psychiatric Drugs + Mortality
Every hospitalization I had in Ireland between November 1980 and April 1984 (bar the first) was a Suicidal Event. I never attempted suicide before I consumed Strong Psychiatric Drugs – or after discontinuing Strong Psychiatric Drugs.
Near Fatal Modecate Experience Pg 1
https://drive.google.com/file/d/0B0zhbh8V4MBAVk1KSmgwZTdKeHM/view?usp=drivesdk
Near Fatal Modecate Experience Pg 2
https://drive.google.com/file/d/0B0zhbh8V4MBAemlnNW0zUERieDA/view?usp=drivesdk
If I hadn’t managed to stop taking these drugs in 1984, I would still be a Psychiatric Patient.
Report comment
From Dr Philip Hickey
https://www.madinamerica.com/2016/11/neuroleptic-drugs-akathisia-suicide-violence/
https://en.m.wikipedia.org/wiki/Akathisia
From Wikipedia:
“…Neuro-psychologist Dennis Staker had drug-induced akathisia for two days. His description of his experience was this: “It was the worst feeling I have ever had in my entire life. I wouldn’t wish it on my worst enemy.”..”
Report comment
Did someone say “schizophrenia”? Is MIA still so backward as to believe that “schizophrenia” is a psychiatric “disease”? Please, please, please. “Schizophrenia” is nothing more than the sacred symbol of psychiatry. https://psychiatricsurvivors.wordpress.com/2016/06/19/schizophrenia-the-sacred-symbol-of-psychiatry/
Report comment
You’re right, none of the DSM disorders are valid disease entities, including “schizophrenia.”
https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2013/transforming-diagnosis.shtml
And here’s your medical evidence that the antipsychotics/neuroleptics can create both the negative and positive symptoms of so called “schizophrenia.” The antipsychotics/neuroleptics create the negative symptoms of “schizophrenia” via neuroleptic induced deficit syndrome. And the antipsychotics/neuroleptics create the positive symptoms of “schizophrenia” via antipsychotic induced anticholinergic toxidrome.
https://en.wikipedia.org/wiki/Neuroleptic-induced_deficit_syndrome
https://en.wikipedia.org/wiki/Toxidrome
The symptoms of “schizophrenia” are real, and the “schizophrenia” treatments create both the negative and positive “schizophrenia” symptoms.
Withdrawal from the antipsychotics can also create a drug withdrawal induced “super sensitivity manic psychosis,” which is always misdiagnosed as a “return of the illness.”
Our society could get rid of “schizophrenia,” if we could just get the doctors to stop prescribing and forcing the antipsychotics/neuroleptics onto innocent human beings in the first place. Wake up, psychiatrists!
Report comment
Dr Joanna,
I think your main motivation is to improve people’s lives.
SCHIZOPHRENIA
Most people that are diagnosed as “schizophrenic” are not “schizophrenic” at all.
They might have problems – but they are not “schizophrenic”. In Psychiatry “schizophrenia” is about making money.
MEDICATION
When I stopped taking “medication” I found I couldn’t survive without the “medication” even though I was okay refusing it to begin with. In my opinion the main problem is the “medication”.
Whether a person Recovers or not in my opinion, depends on their ability to withdraw successfully from the “medication”.
DISABILITY
Psychiatric Drugs are very disabling and In my opinion its the “medication” that causes the Disability the Taxpayer Pays for.
PSYCHIATRIC DRUGS CAUSING SUICIDE
My Drug induced suicide attempts and hospitalizations, and the attempts to cover these up, can be identified on my records in Black and White.
Suicidal tendency was only a problem for me while I consumed Psychiatric Drugs suitable for Severe Mental Illness.
Report comment
NEAR FATAL COVER UP 1.
On November 8 1986 I wrote to Doctors at Galway Ireland asking them to send over Adverse Drug Reaction Warning to the UK concerning the Drug Modecate Depot:-
ADR Request ltr Pg 1
https://drive.google.com/file/d/0B0zhbh8V4MBAZlVTbHdBRDFFSHc/view?usp=drivesdk
ADR Request ltr Pg 2
https://drive.google.com/file/d/0B0zhbh8V4MBAZ0otNjFyN0NJajA/view?usp=drivesdk
ADR Request Ltr Pg 3
https://drive.google.com/file/d/0B0zhbh8V4MBAcExwMzhEMVRzdm8/view?usp=drivesdk
The 1986 ADR Warning Request Letter describes AKATHISIA fairly Well :-
1. Extreme Restlessness
2. Unpredictability
3. The worst experience of my life.
4. What I am most worried about
IN RESPONSE:-
Dr Donlon Kenny from Galway sent over a 24 November 1986 Record Summary with Adverse Drug Reaction Warning Deliberately OMITTED.
Irish Record Summary Pg 1
https://drive.google.com/file/d/0B0zhbh8V4MBATlNoNTlpYy11X28/view?usp=drivesdk
Irish Record Summary Pg 2
https://drive.google.com/file/d/0B0zhbh8V4MBAMmlqS18xQVZlcms/view?usp=drivesdk
INACCURACY
The 1986 Irish Record Summary also contains significant distortion. For example at the Original Admission at Galway Southern Ireland in 1980 :- I Presented with NO Psychotic Symptoms.
Admitting Doctor Dr Fadel on Presentation
https://drive.google.com/file/d/0B0zhbh8V4MBANjBTZEtkbjBhMkU/view?usp=drivesdk
PSYCHOPATHIC BEHAVIOUR
Dr Donlon Kenny at the time also sent me a letter dishonestly reassuring me that my concerns had been looked after.
Dr Donlon Kenny False Reasurrance Ltr
https://drive.google.com/file/d/0B0zhbh8V4MBAeUFLam5rYmtXd3c/view?usp=drivesdk
Report comment
NEAR FATAL COVER UP 2.
In October 2012 I discovered to my horror that my GP Surgery at London W2 5LT had been “making use” of my dated 1986 Irish Record Summary (as if it were a present day event) for Financial gain.
When I originally signed up with this GP Surgery in 1997 they were too lazy to follow anything up, so they guessed Mental Health Diagnosis – but they guessed wrongly.
When they discovered in 2002 that they could gain financially they sought my records out and then discovered their mistake. So the doctors altered the 1986 Irish Record Summary by cutting out the last paragraph of the first page.
In 2002 I was working as a building subcontractor in the House of Commons.
My GP Surgery never in 5 years interviewed me so they knew nothing about my history, and when I showed my doctor the 1986 Adverse Drug Reaction Letter (in October 2012) he got so frightened that his shirt ended up sticking to his body.
First of all he promised me and committed in writing to the removal of all diagnosis. Some time later I discovered he hadn’t done as he had promised and I complained – he then responded in writing with fairly useless excuses.
NEAR FATAL COVER UP
But this doctors Surgery at London W2 5LT still have not acknowledged the 1986 Adverse Drug Reaction Warning Request letter which explains my hospitalizations and my Disability.
They are intentionally covering up Psychopathic Behavior from historical doctors at Galway, Southern Ireland, and attempting to follow their “guidance”.
Report comment
Below, is a Research Paper from my Historical Consultant Psychiatrist at Ireland on the Offending “medication”, from 1998.
https://ps.psychiatryonline.org/doi/full/10.1176/ps.49.10.1361-b
There’s NO mention in this Paper of:
1. Drug Suicidal Reaction,
2. Drug Induced Disability,
3. Drug Rebound Syndrome,
4. The Option of Full Recovery,
as a result of Careful Withdrawal from these Drugs, with Psychotherapy.
https://www.nuigalway.ie/our-research/partners/
€ 9.6 million from the manufacturer.
Modecate (Fluphenazine): Suicidal
Identification, from 1983
https://www.madinamerica.com/wp-content/uploads/2016/11/Suicide-Associated-with-Akathisia-and-Depot-Fluphenzaine-Treatment-KShear-1983.pdf
Report comment
Dear Fiachra and others,
I agree that the term ‘schizophrenia’ is meaningless, since it is applied to so many different situations which have little in common with each other. I am sorry to hear about your previous experiences with the medical system.
Joanna
Report comment
Dr Moncrieff points out the authors’ links to pharmaceutical companies, but the implied claim in her books and other articles over the last decade, that she is primarily concerned to reduce overmedication in mental health practice, is questionable.
The UK’s ‘Critical Psychiatry Network’ of which she is co-chair, has known about complaints to the Royal College of Psychiatrists, concerning their ‘false, misleading and irresponsible’ statements about ‘antidepressants’ for nearly two months: http://www.drnmblog.wordpress.com/2018/03/27/rcpsych-oligarchy-now-appears-to-be-deliberately-misleading-while-spinning-its-response-to-my-complaint-about-its-statements-on-cipriani-et-al/ .
Neither Dr Moncrieff, nor the other co-Chair, Dr Hugh Middleton have supported the complaints. This failure to significantly criticise pro-pharmaceutical bias by UK psychiatrists appears to go back to, at least, 2013, when Dr Charles Nemeroff MD gave a prestigious lecture at London’s Institute of Psychiatry (IoP). Dr Carmine Pariante MRCPsych (of the IoP) simply wrote a letter to ‘dear Joanna’, and neither Dr Moncrieff nor her co-Chair ever referred (to my knowledge) to the corrupt GSK-funded psychiatrist again: http://freepdfhosting.com/5be73b1bf4.pdf
A few days ago I left a brief comment on Dr Moncrieff’s Blog, with a link to my mildly critical Blog post on ‘Pillshaming is real’
( https://drnmblog.wordpress.com/2018/04/18/pillshaming-is-real-heres-a-newish-way-to-reduce-it-and-to-reduce-antidepressant-use/ ). That comment is still being moderated. I will now attempt to leave a brief comment below this (duplicate) piece on her Blog, with a link back here. If Dr Moncrieff declines to allow my comments through moderation then it will be clear to all that the ‘Critical Psychiatry Network’, under its current co-Chairs, seeks to impose a narrow and misleading version of ‘critical’ discourse.
Report comment
Dear Neil,
I approved your comment on pillshaming as soon as I was notified about it. It appears on my version of my website. Please let me know if you still can’t see it.
Hugh Middleton and several other psychiatrists from the Citical Psychiatry Network signed the recent complaint about the Royal College’s coverage of antidepressant withdrawal. I did not as I have too much on my plate with trying to get the Radar trial completed at the moment.
Also, the Critical Psychiatry Network was critical of the invitation to Charles Nemeroff back in 2013, and we managed to get coverage of it in the Independent newspaper https://www.independent.co.uk/life-style/health-and-families/health-news/honoured-in-britain-the-us-psychiatrist-who-took-12m-from-drug-companies-8654535.html
Joanna
Report comment
I’m a bit confused as to what Dr MacFarlane is saying, because he says that critical psychiatrists have overstepped the mark by saying there’s no such thing as an antidepressant, and yet he accuses them of having only a questionable commitment to reducing overmedication. I stand to be corrected, but could any psychiatrist be doing more to provide an evidence based criticism both here and in scientific papers, not to mention a really significant real life drug-reduction programme, than Joanna Moncrieff?
Report comment
Yes, I suggest that extremist language such as Peter Gotzsche’s ‘depression pills can’t cure anything’ cause unnecessary distress to people with depression who opt for medication, often comes across as ‘depression doesn’t exist’, and doesn’t address the issue of adequate support.
Of course there is some valid criticism of drugs in Dr Moncrieff’s work (as in that of many others), but the call to move towards a ‘drugs-based model’ and away from a ‘diagnosis-based model’ is in keeping with ‘depression doesn’t exist’. That is not just ‘pillshaming’ but also ‘diagnosis-shaming’.
Dr Moncrieff has been criticised for suggesting that ‘to reduce benefit levels’ is a primary aim of psychiatry: http://philipfthomas.com/?p=68 . Her response was not entirely convincing: http://www.madinamerica.com/2016/01/what-disability-benefit-trends-tell-us-about-psychiatric-treatments-and-the-economy/
Dr Moncrieff evades the fact that the complaint I linked to is about the ‘final answer’ claims for antidepressant efficacy in the February 21st Lancet study (Cipriani et al), not the separate complaint about ‘withdrawal’.
I have not looked at the RADAR trial in detail as I have not prescribed antipsychotic medication for nearly a decade. But, as Dr Moncrieff acknowledges, the so-called ‘Critical Psychiatry Network’ (CPN) has been near-silent on key aspects of pharmaceutical company behaviour since mid-2013. If there is near-silence on Pharma and antidepressants then how credible is CPN research on antipsychotics?
Report comment
It’s reasonable to be ashamed of being called a dangerous madman or madwoman. I do not tell people about my defamatory “diagnosis” because of this. SMI is publicly understood to be a state not just of poor judgment, but moral turpitude.
As far as “pill shaming” and “diagnosis shaming,” who dishes out the pills and defamatory labels? The real shame is not on those “helped” by psychiatry!
Report comment
‘depression doesn’t exist’
Or as has been discussed here often, “depression” is a tautology.
Report comment
Depression does exist but it isn’t an illness.
Report comment
Dr MacFarlane. On Dr Gotzsche: So-called antidepressants don’t cure anything, and in all probability there is no such thing (yet) as an antidepressant. Something can exist and be potentially lethal without being an illness and without needing inneffective drugs. The question of what support interventions might be effective is a different issue and one that involves psychologists and occupational therapists, not just psychiatrists.
As regards the drugs-based model and the discredited disease based model: I have heard from 2 NHS Consultants now that mental illness is caused by a chemical imbalance that the drugs either treat or normalize. This is the deceitful consequence of the disease-based model and leaves you enfeebled and dejected. Shame, yes, shame on them. Or do you think that they are right?
As regards the final answer, putting-to-bed, compelling evidence etc: Dr Moncrieff has said they are placebos, and made other really strong statements. We all know the SMC statements were just comical – I just don’t know where to start with Prof Taylors “much more effective than placebo” quote.
Report comment
Medical science based on lies helps no one but those profiting from selling the ineffective treatments.
Report comment
more lies from mainstream psychiatry. why am I not surprised? I do, however, appreciate Dr. Moncrieff’s work, and the work of other dissident “mental health professionals.”
Report comment
more lies from mainstream psychiatry
Is there some other kind?
Report comment
For my part I found the message that antidepressants don’t work to be highly empowering. This message gave me a sense of hope! It was not my fault the drugs made me feel awful after all. They were no better than street drugs and long term use of those never helped anyone think straight or feel good. They told us that in the 80’s.
But some liars told us the psych drugs were medicine that would set everything straight in my brain since sadness was a brain disease. No way I would have taken them if I had known. Nor would my conservative parents have willingly forced their first born into the career of professional Junkie. 🙁
Been drug free since August 30. Celebrating my anniversary of Drug Free Living in a few months.
I found a job. I can keep my house clean with effort (never could on my drug cocktail.) And I am writing more. And I can enjoy novels in a way I haven’t since I was in my teens.
Like coming alive again. Just sad it took 25 years.
Report comment
To repeat: I think UK depression is 10x (at least) overmedicated and other disorders are as well, maybe less so, maybe more.
My new Blog piece shows how Dr Moncrieff and other supposedly ‘critical’ psychiatrists and psychologists are in reality much closer to ‘mainstream psychiatry’, or even part of it. See the many positive comments from UK non-psychiatrists below it:
https://drnmblog.wordpress.com/2018/05/23/how-drop-the-disorder-colludes-with-the-neoliberalism-it-claims-to-oppose/
Report comment
Dr MacFarlane
I read your blog with close interest, often 2 or 3 times because the links seem to be everywhere. But I’m baffled. What is the point of pushing an argument that the CPN are politically right-leaning? As a slight right-leaner myself I dont see it at all, to be honest I sense more leanings to the left, but I just don’t care which way they lean. I just see people driven by conscience to expose the evidence about mental problems and their treatment. They are winning the argument on the ground and as a user I’m pleased and relieved with the work they do. No doubt I will be flamed, but I don’t see this as politics: human rights yes, but not a left-right neo-lib thing.
Report comment
Hi ConcernedCarer…my perspective on this seems to be new here in the UK, and I was concerned to back it up with evidence (or at least the opinions of others) which led to my putting in so many links. I presume you are based in the US: please correct me if otherwise!
The CPN is not right-leaning: they are mostly ‘leftist’, although within that there is a spectrum. I think what I say can be extended beyond the UK: governments since Reagan/Thatcher have been ‘right-leaning’ in the ‘neoliberal’ sense of looking to cut taxes & they pick on the vulnerable as an easy target.
There is a long tradition within Marxism of attacking political centrism (‘social democracy’ in Europe) because that, in their view, delays true socialism. That has given rise to unlikely left-right alliances. You could argue that Bernie Sanders’ campaign against Hillary Clinton was of this pattern: although I would say she dealt with that rather clumsily.
I am more concerned about overmedication than overdiagnosis. I don’t agree that if we abolish the latter then the former will fade away: to reduce overmedication, especially in mild & moderate disorders which should mostly be unmedicated, we need to regulate Pharma and oppose its lobbying. My position is closer to Allan Frances.
Hence my pointing out that the CPN’s criticisms of Pharma are actually weak. They have managed to ‘market’ themselves into something they are not, somewhat like many ‘academic Marxists’.
Anyway, thanks for your comments. In the next few months I would like to write something focused more on the US, with US politics & culture as the context.
Report comment
The study seems to be about death and relaps. From a patient point of view the most importent question for me is does “stayng on meds” promote to become healthy (recovery) and functioning well (e. g. cognitive functions). This has become mainstream i strategies. Both the United States, Canada, New Zealand, Australia, the UK and Ireland are building their national strategies on recovery. I can not see the study even looked at this question. What happens with patients never been on meds? Looking from this perspective I found: A paradigm shift to reducing meds from beginning is favorable: Open dialogue achieves quadruple recovery rate, reduces schizophrenia per year to one tenth and disability allowance/sickness is reduced to one third: http://wkeim.bplaced.net/files/recovery-en.html
Report comment
Historical context: Mortality and Standardized Mortality Ratios (SMR) for Mental Illness including Schizophrenia
The standardized mortality ratio or SMR, is a quantity, expressed as either a ratio quantifying the increase or decrease in mortality of a study cohort with respect to the general population.
Dramatic increase in suicide in hospitals from the 50’s to the 80’s
In the mid-50s antipsychotics / neuroleptics where introduced. In the 3 decades from 1950s to 1980s inpatient suicides in psychiatric hospitals ten doubled in Norway (Retterstøl 1988), raised from 50 to 400 per 100 000 in V.A. Hospitals ( Farberow 1975). Similar tendencies are reported from more that 8 countries (Chart 1: Bowers et al. 2008).
Highly reduced life expectancy for psychiatric patients in the 2000s
“SMRs for the 1970s, 1980s, and 1990s were 1.8, 3.0, and 3.2, respectively” (John McGrath et al. 2008) i.e. mortality rates continue to increase in several countries. “The most striking figure in this study is that eliminating suicide in schizophrenia would restore life expectancy to normal.” (David Healy et al 2012). Tiihonens 2009 FIN11 cohort study suggested that antipsychotic use decreased all-cause mortality. De Hert et al. 2010 showed incomplete reporting of data e. g. “exclusion of deaths occurring during hospitalization leading to exclusion of 64% of deaths on current antipsychotics from the analysis”.
Reduced lifetime expectancy for male psychiatric patients in the 21st century was 22 years in Denmark, 19 years in Finland and 20 years in Sweden. This corresponded to the SMR for life expectancy of 2.5 for Denmark, 1.8 for Finland and 2.2 for Sweden, respectively. SMR for suicide was 25, 9 and 21, i.e. suicide is the dominant cause. Women’s numbers are lower (Wahlbeck et al 2011).
Therefore “Antipsychotics should be used more selectively, for shorter durations and with lowest possible effective dose.” (Weinmann et al. 2010).
“People with serious mental illness die up to 20 years younger …” … “Healthcare services should consider a shift away from physical health monitoring strategies and instead focus their resources on primary prevention strategies … These include assertive smoking cessation (with pharmacological support), diet and exercise interventions and where possible, to avoid long-term prescription of antipsychotics associated with adverse metabolic outcomes.” (Athif Ilyas et al. 2017)
http://wkeim.bplaced.net/files/mortality-references.html
Report comment