An issue that we think deserves more media attention than it is currently receiving is the idea of Preventive Intervention in Psychiatry. The goal of Preventive Intervention is to reduce the rate of psychiatric diagnoses in an at-risk group of people by pretreating all the group members with a medication. For instance, could the rate of PTSD in the military be reduced by pretreating everybody in the military with an SSRI?
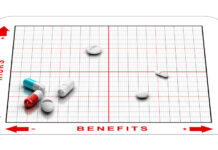
Even if a pretreatment plan is successful in reducing the rate of diagnoses in a given group, there is an obvious downside. To reduce the rate of diagnosis for a minority of the group, the majority of the group must start a lifetime course of treatment for a condition they would never develop. While there are good examples of disease prevention in general medicine – the polio vaccine comes to mind – it is clear at this point that antidepressants are not vaccines.
One research team, directed by Dr. Robert Robinson, is conducting studies on how to prevent depression from developing in patients who have had a stroke. Their reasoning is as follows: If we know that 20%, or some such number, of stroke patients eventually go on to develop depression, can we reduce this percentage by pretreating the entire stroke population? If we pretreat the entire population, then maybe only 10%, rather than 20%, will go on to develop depression.
One of the major studies that this group published was in JAMA in 2008. And “Yes” it was the same study that caused an uproar in the press and eventually led the JAMA editors to try and enact a very questionable policy restricting freedom of speech. But this is off topic.
The study in question examined the use of Lexapro and problem solving therapy for post stroke depression. Both treatment groups had better outcomes than the placebo group. Specifically, in each group the reported incidence of minor depression was: Lexapro, 8.5%; Problem-Solving Therapy, 11.9%; and Placebo, 22.4%. The study concluded that, “Patients who received placebo were significantly more likely to develop depression than individuals who received escitalopram (Lexapro).” As reported in the paper, based on the frequency of depression during the first year of treatment, 7.2 acute stroke patients would need to be treated with Lexapro to prevent one case of minor depression.
When the study was first designed, the protocol submitted to NIH, per grant R01MH065134, called for a four-arm study using Nortriptyline, Celexa, psychotherapy, and placebo. Celexa and Lexapro are both manufactured by Forest Pharmaceuticals. Forest’s patent for Celexa expired in July of 2003. In 2002, Forest spent a significant amount of money on the marketing plan for Lexapro which is a very similar medication to Celexa and has been referred to as a “patent extending” variation of Celexa. By the time of patient enrollment for the post-stroke study, it had become a three-arm trial with Lexapro, psychotherapy and placebo. The paper states that escitalopram (Lexapro) was used instead of citalopram “because of empirical evidence” of possible superiority. Two references are cited. The first (Tamminga et al) is a “thought piece”, not empirical evidence, and does not mention escitalopram (Lexapro). For the second citation, a Lundbeck sponsored study published in 2005, it is hard to see how it informed a decision to switch from Celexa to Lexapro made in 2003. Nortriptyline is not mentioned although Robinson’s study published in 2000 supports superior efficacy of nortriptyline over fluoxetine. In 2009, Lexapro cost over 5 times as much as nortriptyline and over twice as much as generic citalopram.
Following the post-stoke study’s publication it was featured on several media outlets. On Fox News, an academic psychiatrist stated: “Dr. Robinson’s work supports a novel way of preventing such suffering and disability.” The article also stated that “he hopes doctors will start prescribing preventive antidepressants to stroke patients.”
In the USA today, Dr. Robinson was quoted as saying, “I think every stroke patient who can tolerate an antidepressant should be given one to prevent depression.” The paper also reported that Dr. Thomas Insel, the Head of NIMH, disagreed with this statement.
The idea of preventing disease from developing in susceptible populations by administering a medication raises questions about the future of medicine – not just psychiatry. For instance, could we decrease the rate of coronary heart disease by giving everybody over 45 years of age low doses of statins? Most importantly, what is the harm-to-benefit ratio involved with prescribing antidepressants to all stroke patients, especially when the vast majority of them will not develop depression following the stroke even if left untreated? Given a 3% difference between medication and therapy, why not just offer problem-solving therapy universally?
When it comes to psychological health, surely stroke patients are not the only susceptible population. Now that the bereavement exclusion is gone from the DSM-V, should we prescribe a prophylactic course of antidepressant therapy for anyone who has lost a loved one? Even if a prevention plan reduces the number of people who eventually receive a diagnosis of depression what about all the healthy people exposed to a medication’s side effects?
In a 2009 editorial, in The British Journal of Psychiatry, titled, “Prevention of First-Episode Depression: Progress and Potential” Dr. Robinson and Ricardo Jorge discuss the idea of preventive treatment for psychiatry. In the introduction they state, “The Institute of Medicine Committee on Prevention of Mental Disorders recommended in 1994 that prevention intervention defined as an intervention before the patient receives a diagnosis.” And in their conclusion they state, “Perhaps three months of antidepressants administered to 20- or 30-year olds with no physical illness or history of mood disorders or to 60-year olds might block the effects of subsequent depressions or physical illness with associated depression on morbidity or mortality. Obviously only empirical data can answer these questions, but as preventive interventions in psychiatry continue to emerge, we should not set our sights too low.”
This idea of prescribing antidepressants for people who do not meet the criteria of a psychiatric diagnosis but who meet the criteria for membership in another group, that happens to have a higher than average rate of diagnosis is worthy of debate. What about other high risk groups? Should we medicate all the veterans returning from Irag, all the pregnant women in the country, and all the children in foster homes? Where do we stop? At some point in our lives we probably all fall into a high-risk group.














The problem is that antidepressants don’t work any better than placebo. They’re useless and dangerous. Citalopram can cause heart attacks! Plus, antidepressants can lead to suicide attempts. They blunt emotions and keep people from being in touch with their feelings. Watch the number of suicides jump if they start giving antidepressants to everyone. But hey, who cares as long as the drug companies want to do this! Their billions of dollars in profits are much more important than the lives of human beings.
Report comment
As one who has never had a stroke but has had similar type issues that were greatly worsened by being on ADs long term, I am horrified at the thought of giving ADs to stroke victims prophylactically. Yeah, and even if they develop depression, seeing their abilities further deteriorate thanks to the meds will make things alot worse.
But as Stephen Gilbert so wonderfully points out, who cares about what happens to human beings as long as the profit dollars are preserved.
Report comment
Hi guys. Thanks for another great post, this time on a neglected topic I think deserves more attention. Anyone who has read Anatomy of an Epidemic should be skeptical of the potential consequences of prevention programs that (a) increase the likelihood of exposure to psychiatric medications, and/or (b) “educate” individuals that their symptoms may signify a chronic, biologically-based mental illness. At the university where I work, all athletes are screened with a depression questionnaire. Every athlete who scores above a pre-determined cutoff score is informed that he or she is at risk for clinical depression and is provided with information about treatment options. This mental health screening program and others like it (e.g., “National Depression Screening Day”) are typically regarded as benevolent and helpful. I’m not convinced of this, especially when there is literally no scientific evidence to support the mental health benefits of such interventions.
Report comment
Let me take a big guess as to who provides the money for these screenings. Could it be the drug companies??????!!!!!!!!
Report comment
Looks like a good guess: http://www.cchrint.org/psycho-pharmaceutical-front-groups/screening-for-mental-health-inc/#_edn9. The corporation that initiated National Depression Screening Day (and other, related efforts) is heavily subsidized by drug companies and is presided over by a biological psychiatrist with extensive pharma ties.
Report comment
Pfizer was all that I needed to see. One of the most corrupt of all drug companies.
Report comment
Whitaker’s work is critical here. It seems more likely that we’d be causing depression in people who wouldn’t develop it otherwise. This is INSANITY!
— Steve
Report comment
I thought i’ve seen it all and i was shock proof but wow! How many times does it need to be said that psychiatry is a scam, fraud, swindle perpetrated by delusional quacks? I’m getting tired saying this.
Report comment
I have one answer as to why this so called preventative work is being developed: http://www.youtube.com/watch?v=NWg8iaLuBDg
Report comment
If antidepressant prevented suicides we would see it in statistics.
We do *not*.
So, they do not “save lives.”
The subjective idea that they improve the quality of life?
Again, we would see it.
And we do *not”.
What we *do* see is people becoming *fat* and *asexual*.
Kinda depressing, actually.
Duane
Report comment
Yes, the regress here leads us back to termination of the pregnancy or, better yet, the forced sterilization of high-risk breeders. This hateful language/attitude has been documented in Robert’s book, ‘Mad in America.’ Many readers will be surprised to read that eugenics was first an American idea and several States passed forced sterilization laws. These laws were repealed after WWII but this had less to do with a shift in attitude towards the “mentally defective” and more to do with the horror/outrage of the concentration camps.
I share the authors concern with the increase in so-called mental health prevention efforts. We’ve seen how the DSM 5 will make “early diagnosis” easier. Many of you have seen/read the reactions in the media and elsewhere after Sandyhook, “If we could just have gotten to them sooner…”
The day may come where we’re encouraged to start taking our meds before trying to have a baby. Surely, we can combine our contraceptives with psychotropics for a more efficient delivery system.
*This response contains some sarcasm.
Report comment
I think the mention of the eugenics movement in the first half of the XX century is particularly apt. The combination of bad science, ideology and economic interests that drove the eugenics movement are very comparable to what drives psychiatry nowadays.
But this comparison also offers some hope; I’m thinking of G.K. Chesterton, the writer who in the UK managed to almost single-handedly deflate the support for eugenic policies (Churchill was very keen on them) by continuously exposing the absurdity of eugenics with great humour and common-sense. He was not a scientist or a politician or someone in a position of power, just a man with a brain, courage and, admittedly, a degree of access to the media. He showed that it can be done.
His articles against eugenics make very educational reading; you might want to check out for example “Eugenics and Other Evils” edited by Michael W. Perry. Inkling Books, Seattle, 2000. (ISBN 1-58742-002-3)
Report comment
Thanks for the book suggestion, it looks fascinating!
Report comment
The secret agenda is to lower the rate of population growth. Antidepressants are much more effective at reducing libido and sexual response than they are at reducing depression.
Report comment
How can you cal it secret anymore? It’s so blatant.
Report comment
Thank you for this valuable article. One positive result, though, of the the situation you write about is that this outrageous overreaching by psychiatry and the drug companies may lead to a big backlash by the public.
Well, I hope so anyway.
Report comment
Good point Ted. Surely society will eventually get the message that everyone is at risk of psychiatric interference and fiddling. Then let’s hope that psychiatry rather than the so called mentally ill become the targets for stigmatising behaviour and labelling.
Report comment
I’m not so sure. Yesterday afternoon I just happened to catch part of the Katie Couric talk show and there was a young housewife and mother telling the audience how she had a chemical imbalance in her brain and truly needed her antidepressants so that she could function better as a mother and wife in her family! And the audience applauded enthusiastically!
Report comment
I know what you mean. I see that the so-called ‘Chemical imbalance’ theory is being supported by Rethink, the ‘mental health charity’…
“There are several types of antidepressants one of which you may be prescribed. While all the antidepressants seem to be equally effective, one may suit you better than another. This is a brief guide to antidepressant medication.
Two of the chemical messengers in the brain are called serotonin (sometimes called 5-HT) and noradrenaline. Both are important in the areas of the brain that control or regulate mood and thinking. It is known that these two chemical messengers are not as effective or active as normal in the brain of someone who is depressed.
Antidepressants increase the amount of these chemical messengers, helping to correct the lack of action of the messengers and improving mood.
Antidepressants are not addictive.”
http://www.rethink.org/living_with_mental_illness/treatment_and_therapy/medication/antidepressants/index.html
I wonder if this has anything to do with Rethink’s partnership with Lundbeck, creators of Celexa and Lexapro? http://www.lundbeck.com/uk/the-community/charities
It also begs the question; what is a supposed ‘charity’ doing, involving themselves with any drug company and spouting about medication?
Leonie
Report comment
This idea of “preventative intervention in Psychiatry” shows that they are in denial regarding the damage been done by messing with people’s brain chemistry. A Yale study found that about 1 in 12 admissions to Psychiatric hospitals was a result of “mania” or “psychosis” induced by SSRIs. http://www.ncbi.nlm.nih.gov/pubmed/11235925
Not forgetting the risk to the unborn baby and the lawsuits eg relating to the drug Celexa (Citalopram).
http://www.celexa-birthdefects.com/
Also not forgetting the link between SSRIs and suicide and violence in some people.
Report comment
I can personally attest to this. I went manic on Celexa. This was a slow build up that actually took place over a number of years, as my akathisia and insomnia got worse. My pdoc treated those symptoms with more xanax, and trazodone. I developed severe alcohol cravings and told him about it and his response was to increase my dose of Celexa. A couple of months later, I tried to kill myself while on a business trip, by downing an entire bottle of Celexa in my hotel room. I remember little of it.
I spent the night in the ER. I am surprised I wasn’t taken to the psych ward (and grateful), but they treated it more as an alcohol related even (I’d been drinking as well).
When I got home I told my pdoc about it, and he chided me. To him, this was a silly joke.
I asked for a medication holiday and he refused to cooperate, so I tapered off all meds on my own. It was brutal, but I no longer take psychiatric meds.
I cringe when I hear groups like the NRA call for widespread psych screenings. More people on psych meds= more violence. Guaranteed!
Report comment
Thanks for revealing the story. It’s paradigmatic in several ways, and it’s the kind of thing the public should knows. Instead of making plans to get you off the SSRI yiour shrink puts you on drugs that will mitigate your symptoms, supposedly. But meantime your on more drugs. Then he increases the SSRI which predictably will make your more agitated. Then after a dramatic suicide attempt he laughs and still refuses to help you get off drugs. Wow. And when you think the the State brings all its weight down on the poor guy selling crack on the corner. The latter is benign compared to the cunning and nefarious government licensed drug dealer. Everyone should read this story. Congratulations for making it through.
Seth Farber
http://www.sethHfarber.com
Report comment
Thank you, Seth. I bookmarked your web page. Yes, in retrospect one would wonder why a patient would put up with this abuse, but when in the midst of it, it’s hard to gauge what is going on and how much the medication has thrown off good judgement. I actually welcome the manic episode now, only because it was the kick in the pants I needed to get off of these drugs and away from this kind of “treatment.”
Report comment
It really is hard to know whether to laugh or cry. Even accounting for rampant stupidity and corruption it becomes increasingly hard not to give in to paranoid tendencies and start believing there’s a Dr. No-style villain pulling the strings from some secret base in an uncharted tropical island and trying to bring about the collapse of civilization. Where’s 007 when you really need him?
Coincidentally I was just reading this on the BBC:
http://www.bbc.co.uk/news/magazine-21636723
An out-of-work single mother of two living in a motel and relying on a food bank to (more or less) feed her children says: “I seen a doctor… for depression. She put me on some anti depressants and Xanax for my panic attacks.”
Well, there you have it, forget stroke patients, think big – unemployment carries a big risk of depression, so does poverty, what better group for carrying out government-funded campaigns of mass prevention of depression? Think about it, what a gold mine!
Report comment
They are not trying to collapse western civilization, but create a class of serfs and overlords that was the model for much of human history. A strong middle class threatens their oligarchy and has been an aberration for much of human existence. They are the predators and we are the prey. There is nothing they will stop at to complete this transformation. False flag terrorist attacks, brutal austerity, 1984 surveillance, drones etc. We are not going to get anywhere if we are soft and naive. Psychiatry is just a tool. DO PEOPLE GET THIS?
Report comment
I wish I could believe that – it would be a relief to think that at least they know what they’re doing. But my fear is that it might be more a case of the blind leading the blind, all following the tinkling of coins in each other’s pockets.
But whatever the reason or unreason behind the idea of preventive psychiatric interventions I can think of fewer things that could unravel a society faster and more efficiently than this. It is just pure madness – the bad kind of madness.
Report comment
Also, I wish there was an “edit your post” option on this site or alternatively that I would learn to re-read my posts before I hit “Post Comment” instead of afterwards. The humiliation of typos and careless grammar…
Report comment
You’re not alone with that wish.
Duane
Report comment
To clarify.
I do the same thing, Morias.
Duane
Report comment
And if the state welfare authorities referred her for those meds, you can guarantee they will eventually force compliance by threatening to remove her children. Lots of people end up on the drug carousel this way.
Report comment
Stephen Gilbert’s data is correct.SSRIs are no better than placebos for reducing depression, and much worse than exercise. But let’s add some date. Healy shows that the placebo suicides are really withdrawal suicides. Thus the popular SSRI anti-depressant are 3 to 10 times more likely to trigger suicide. These drugs are extraordinarily dangerous. Add to this 50% impotence in males. In addition 20% will develop mania and be re-diagnosed as “bipolar.” Soon they’ll be on a cocktail of drugs, which will lead to premature death preceded by diabetes and tardive dyskinesia. Don’t forget these drugs are Jekyll and Hyde drugs so with these numbers on SSRIs there are sure to be a many more gruesome murders. If there are any settlement it will be done quietly out of court so the public will never find out about it.
None of this will lead the public to blame the drug companies since as Mencken said “no one ever went broke underestimating the intelligence of the American people.” It’s hard to predict what will happen beyond this because the advertizing writers are so resourceful, and the psychiatrists are so eager to help that short of a major and imaginative effort on the part of anti-psychiatry forces to outwit the drug companies there will not be any movement toward reducing the consumption of drugs.More likely they’ll come up ith a new miracle drug that supposedly has less adverse side effects.
Seth Farber,Ph.D., author of http://www.amazon.com/Spiritual-Gift-Madness-Psychiatry-Movement/dp/159477448X
Report comment
The most astonishing thing about these psychiatric preventive interventions is that according to the model of the very people who propose them they would prevent genetically-determined conditions which should not affect most people regardless of their circumstances. I know that in general psychiatrists are not too bothered about being consistent with their own models of mental illness aetiology but this takes it to new heights of absurdity. You really couldn’t make it up.
Report comment
One issue not highlighted in our original post is the fact that this study examined the prevention of minor depression, not major depression- meaning that prophylactic antidepressants modestly reduced the incidence of not full-blown major depression, but of depression/sadness not conventionally considered to be a major mental disorder.
Report comment
The idea that the drugs work for major depression but not for minor depression comes up quite often.
All I can think is that this argument is void of any common sense.
*If* (and that’s a big, ‘if’) the drugs “work” on major depression how is it that they have little or no effect on anything less than major.
It’s like saying the drugs can “lift” 30 lbs of depression, but cannot “lift” 10 lbs.
Set that dumbell down.
You can’t lift 10 lbs.
Here, try the 30 lbs dumbell.
That should work.
Yeah, right.
It’s void of any common sense.
As is psychiatry as a whole.
Duane
Report comment
spelling – dumbbell
Report comment
There are a lot of “dumbbells” in psychiatry.
Oops,
Duane
Report comment
I have already posted a link to this study on Chrys Muirhead’s “Brain Surgery For Mental Illness In Scotland: Going Under The Knife When Treatment Resistant”, but I think I should re-post it here since it is closely connected to the subject of this article and perhaps Leo & Lacasse will find it interesting if they are not already aware of it. The study in question is: Whalley HC, Sussmann JE, Romaniuk L, Stewart T, Papmeyer M, et al. (2013) Prediction of Depression in Individuals at High Familial Risk of Mood Disorders Using Functional Magnetic Resonance Imaging. PLoS ONE 8(3): e57357. doi:10.1371/journal.pone.0057357
It can be accessed online at:
http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0057357
I think there is little doubt that this study is part of a drive to push for preventive intervention in psychiatry, and in fact claims to have found an effective predictor for MDD (major depressive disorder). Their own conclusion is: “These results suggest that increased activation of the insula can differentiate individuals at high-risk of bipolar disorder who later develop MDD from healthy controls and those at familial risk who remain well. These findings offer the potential of future risk stratification in individuals at risk of mood disorder for familial reasons.”
I confess I have not read the study in detail and in any case I cannot really comment on the data from the fMRIs, but even a cursory look at the study sets off alarm bells. I’ll just mention one issue by way of an example:
Of a control group of 70 (which, interestingly, was almost 40% smaller than the experimental group), 4 people developed MDD. These 4 were simply excluded from the study. This might at first glance seem logical since the control group was supposed to provide the mean values of “healthy” brain functioning with which to compare “high-risk pre-MDD” brains (my terms, not theirs). But in a study which is precisely attempting to identify predictors for MDD one cannot simply exclude 4 members of the study which have in fact developed MDD. To do so is to intentionally exclude relevant data from the study. The fMRI data for those 4 individuals had already been collected, and although they should certainly not be included in the HC (healthy control) group, the HRW (high risk group who remain well at two year follow-up) or the HR-MDD (high risk group who has developed MDD at two year follow-up), they should have been assigned to a group of their own: C-MDD (Control group who has developed MDD at two year follow-up).
A great deal is made in the study of the fact that differences of insula activation have been observed in ALL subjects in the HR group who had MDD two years after being scanned but, leaving aside the reliability of that claim, how about the 4 subjects in the C-MDD group? Did they show differences in insula activation two years prior to MDD diagnostic (or rather, two years prior to follow-up assessment)? If they did, this significantly strengthens the researchers’ claim that atypical insula activation is a predictor of MDD and so it would be absurd to leave that data out of their study. On the other hand, if they did not show differences in activation, this clearly undermines their case for insula activation being a good predictor for MDD, and to leave that data out would call into question their integrity. It is interesting at this point to note the exact wording of their conclusion: “increased activation of the insula can differentiate individuals at high-risk of bipolar disorder who later develop MDD from healthy controls and those at familial risk who remain well.” But not, it would seem, differentiate between healthy controls and controls who later develop MDD…
There is also something else to note about these 4 individuals in the control group who developed MDD, a great missed opportunity: had they been subjected to the same fMRI scanning at the two year follow-up (none of the subjects were, since the study is only concerned with prediction, and apparently only in -potentially lucrative- “high-risk” groups), they could’ve compared brain functioning and/or morphology in those individuals before and after MDD diagnostic. I suspect the findings of this comparison could have been extremely valuable (even if it was in a small number of people) and possibly challenged the assumption that all differences in brain functioning and/or morphology observed in subjects with mood disorders must be in one way or another hereditary and degenerative. But that of course would not sit well in a study that starts: “Mood disorders […] are known to be heritable, with overlapping genetic architecture.”
A lot more (and nothing good) could be said about this study, and this without even touching on the FMRIs themselves. I hope whatever its authors are getting in exchange for their scientific integrity is worth it (as usual, the “Competing Interests” section makes informative if somewhat predictable reading).
Report comment
This type of research is being heavily funded now. You can expect to see a lot more studies like this one. The results of brain scans to diagnose psychiatric disorders are highly questionable. See http://survivingantidepressants.org/index.php?/topic/3953-the-trouble-with-brain-scans-for-psychiatric-problems/
Report comment