There are very few things considered more taboo in the world of mental health than the suggestion that problematic family dynamics can lead to a child developing a psychotic disorder. And yet, when we look honestly at the history and research of psychosis and the broader concept of “mental illness,” it becomes apparent that there are few subjects in the mental health field that are more important. I’d like to invite you, then, to join me on a journey into this taboo territory, dividing our trip into three legs. In the first leg (Part One), we’ll go back in time to explore how such a crucial topic has become so vilified, and then embark upon a flight for an aerial view of some of the most essential findings of the last 60 plus years of research that look at the links between problematic family dynamics and psychosis. In the second leg of the journey (Part Two), we’ll explore a framework that offers us the potential to unify the research on the various problematic family dynamics, trauma, and other factors associated with psychosis, locating the roots of psychosis within two core existential and relational dilemmas that I believe we all struggle with to greater or lesser degrees. Finally, in the third and last leg of our journey (Part Three), we will reap the fruits of our exploration, and consider how what we have learned may guide us as parents, as family members, and as society as a whole in offering genuine support to those who continue to grapple with these extreme states of mind.
A Brief History of a Serious Taboo
Between the late 1940s and the 1980s, we saw a steady flow of exploration and research on the links between certain kinds of parent/child dynamics (and general family systems dynamics) and the subsequent development of psychosis within the child. Among those leading the charge on this research were pioneering psychologists and family systems theorists such as Freida Fromm-Reichmann, Gregory Bateson, R.D. Laing, Murray Bowen and Carl Whitaker. Based upon the fruits of this exploration, there was a period of time in which tremendous hope existed that certain kinds of family therapies and parent education could lead to a significant reduction in the amount of adolescents and young adults who went on to experience psychosis and other distressing states of mind, or that such interventions could at least foster recovery for those who had already gone down this path. One book from that era that I find particularly illuminating and accessible to the layperson, highlighting the hopeful family-oriented movement of this time, is The Family Crucible, which documents a successful family therapy process that leads to the reversal of an adolescent girl going down the path of a schizophrenia diagnosis (Napier & Whitaker, 1978).
Fast forward to today, however, and we find that any quick surf across the internet will pull up a plethora of mainstream mental health organizations that are very quick to denounce the possibility that problematic family dynamics has anything at all to do with a young person developing a psychotic condition. So what happened? It appears that the general assumption within mainstream society today is that somehow the entire 60+ years of research finding links between problematic family dynamics and psychosis must have been thoroughly debunked; and in fact you will find explicit statements to this effect throughout the mainstream mental health field today. And yet, after years of poring over the literature on the etiology and recovery of psychosis, I have yet to find any substantial research that directly contradicts the essential premise that problematic family dynamics can lead to extreme psychological breakdown. So again, what happened?
Let’s rewind to the early 1950s, when the development of the first psychiatric drug, the “antipsychotic” drug Chlorpromazine, led to one of the most powerful industries the world has ever known—that formed by a coalition between the pharmaceutical and the psychiatric industries (which I’ll just refer to as the psychopharm industry for short). This industry was founded on a single ideology—the “mental illness” theory, or “medical model” (which I’ll refer to simply as the medical model)—an ideology that gave this industry tremendous power and influence. The medical model essentially states that distressing states of mind can, for the most part, be categorized into discrete “mental illnesses,” and that although these mental illnesses continue to the present day to be rampant and even growing within our society, we must rest assured that the great medical advances of this industry have already developed powerful drugs that can generally contain them, and that it is just a matter of time before our medical technology will eliminate these illnesses altogether (see my book, Rethinking Madness, or my article here for a more thorough critique on the medical model).
The medical model had already been in existence with varying degrees of power for many decades prior to the development of psychiatric drugs, having been particularly fostered within the field of psychiatry. However, up until this point, the medical model had not been able to fully overcome the popularity of the more psychosocially oriented models and methods when it came to making sense of and dealing with human distress, and this presented a particularly challenging dilemma for the psychopharm industry. How could this industry convince the public that much of human distress could be conceived of as discrete “mental illnesses” arising from diseases of the brain and requiring “medical treatment” with psychiatric drugs at a time when psychosocial interventions were showing so much promise? In the 1970s, the answer to this dilemma came in a somewhat surprising form—the parents of those diagnosed with schizophrenia.
As mentioned earlier, beginning in the late 1940s, we find this very dynamic period of time in the field of psychosis theory and treatment/recovery models in the West, in which a series of studies and projects emerged that offered considerable hope for the prospect that for many young people who were experiencing psychosis, their recovery could be greatly facilitated by addressing the problematic relationships within their life. These included various family and social systems models that supported the entire family or social system, seeing the “identified patient” as essentially a canary in a troubled coal mine; residential facilities such as Soteria, Diabasis and I-Ward, which fostered the development of healthy relationships in away-from-family environments; and transpersonal approaches that viewed such crises from within a spiritual context (i.e., as “spiritual emergencies”), and supported the development of healthy relationship between the “self” and the entire web of interdependence that extends beyond simply one’s immediate social network.
But as this psychosocial movement entered the 1970s, just as it was reaching a point of truly game-changing momentum, a tremendous backlash occurred. Many parents, understandably not feeling comfortable with so many fingers being pointed at them, resisted the idea that they played any role in their children’s development of psychotic conditions, and they began to push back, hard. And it just so happened that the psychopharm industry was more than happy to take full advantage of the situation, providing these parents with the perfect remedy to their dilemma—the medical model. For these parents, this model offered them an alternative narrative that relieved them of any burden of responsibility—their children simply have brain diseases, which is terribly tragic but has nothing to do with family and social dynamics; and for the psychopharm industry, these parents provided the ideal platform with which to spread this model so crucial to increasing their power and their profit margin—what could possibly be a more persuasive “grass roots movement” than an army of concerned parents willing to offer their complete devotion?
The power of this coalition between defensive parents and the psychopharm industry rapidly escalated, leading to a kind of perfect storm that essentially obliterated the movement towards family therapy and general relationship support as a means to addressing psychosis and other extreme states. The flagship organization of this coalition, which still maintains extraordinary power and influence within the mental health field today, is the National Alliance for the Mentally Ill (NAMI). As an indication of just how successful this coalition has been, in spite of over 60 years of very robust research showing strong correlations between problematic family dynamics and psychosis, and in spite of robust research showing the great benefits of fostering healthy interpersonal relationships as a means to support recovery from psychotic conditions (discussed in more detail below), it has become one of the most serious of taboos within the mental health field to suggest that problematic family dynamics can precipitate psychosis and other extreme states of distress.
In short, then, we find ourselves living in a society in which disability due to psychological breakdown has been continuing to grow at nearly exponential rates in spite of (or perhaps partially because of, as documented so well in Robert Whitaker’s Anatomy of an Epidemic; 2010) a psychopharm industry whose scope and power has likewise grown at a nearly exponential rate. And all the while, we find that the very hopeful and well established premise that so much of this psychological breakdown is rooted in problematic family dynamics has been discarded like so much outdated and worthless trash.
I and others have come to believe, however, that this has been a colossal mistake—that if we take the time to pick up this “trash” and carefully reconsider it, we will find that we have thrown away some truly valuable gems, gems that have the potential to offer real peace of mind to so many troubled individuals and families within our troubled society. So let’s take the time now to look more closely at some of the key findings of the links between family/relational dynamics and psychosis, and explore some of the implications of these with regard to avoiding the onset of psychosis in youth, and in supporting the recovery of those who have already experienced such a breakdown. But before we do, let’s first take a closer look at what we mean by the term “psychosis.”
What Exactly Is Psychosis?
We typically throw the word “psychosis” around freely as if we’re pointing to a condition or illness that is well established, but I’ve come to feel that the term “psychosis” is far overused and abused in our society. Essentially, whenever someone has beliefs, perceptions or behaviors that don’t line up with the generally accepted norms of one’s society (i.e., consensus reality), they’re at risk of being diagnosed with a “psychotic disorder,” typically “schizophrenia,” “schizoaffective disorder” or “bipolar disorder.” However, just because certain beliefs, perceptions or behaviors are considered “abnormal” does not automatically imply that they are “unhealthy,” and vice versa. To the contrary, contemporary society as a whole is extremely violent and destructive—indeed, multiple indicators suggest that we as a species will be quite fortunate if we survive the 21st century; so we need to rein in any tendency we may have to automatically assume that “abnormal” beliefs, perceptions and behaviors are problematic or represent “mental illness,” and that “normal” beliefs, perceptions and behaviors are necessarily “healthy.”
As I’ve discussed extensively elsewhere (and as summarized in my article here), I think it’s helpful to first make the distinction between those anomalous experiences (shorthand for “nonconsensus beliefs, perceptions and behaviors”) that are harmful/distressing and those that are not. If they’re not harming anyone or distressing the individual, then what’s the problem? Why give them any kind of label at all? And in those cases where they are harmful or distressing, this still does not necessarily mean that they are qualitatively any different than other harmful or distressing beliefs and behaviors that are considered more “normal,” such as burning fossil fuels, eating meat, getting drunk or believing in the special entitlement of one’s nation, race or religious group.
There clearly are, however, certain states of mind that are more than simply the existence of certain anomalous beliefs, perceptions and behaviors, or experiencing particularly intense states of emotions. Many people clearly do develop a condition in which these kinds of extreme experiences become significantly unstable and overwhelming, and it is this condition to which I think it can be helpful to refer to as “psychosis.” I have come to see this condition as generally representing an unconscious attempt of a desperate psyche to radically transform one’s deepest experience and understanding of the self and the world—a condition that occurs when one’s current experience and understanding of the self and the world has reached a point where it is simply no longer tolerable, for whatever reason. And considering that our capacity to relate to self and other is so profoundly shaped by our relationships with our parents and other close family members, it stands to reason (and to the research, as discussed below) that these most primary of our relationships can profoundly affect our vulnerability or resilience to such psychological breakdown.
An Overview of the Research on Family Dynamics and Psychosis
Regardless of the particular theoretical model used—whether seeing the etiology of psychosis as being predominantly due to “nature” (i.e., biological/genetic) or “nurture” (i.e., one’s environment), or some combination thereof—what remains undisputed is that the development of psychotic conditions tends to run in families. In spite of the fact that the prevailing mainstream belief is that psychotic disorders are caused by yet to be established genetically inherited brain diseases, the research supporting this is actually very weak (discussed more thoroughly in Rethinking Madness; 2012). On the contrary, when looking at the research linking psychosis to environmental conditions, and especially interpersonal conditions, we find quite a rich and compelling history of research that strongly supports this link. Let’s take a moment now to go over some of the most significant of these:
Between the late 1920s and the late 1950s, psychotherapist Frieda Fromm-Reichman devoted much of her time to trying to understand the nature of psychosis, and to working therapeutically one-on-one with people struggling with such conditions. Building her own theories from a predominantly psychoanalytic relational orientation, she essentially came to the conclusion that psychosis typically occurs when a person becomes overwhelmed by a dilemma in which they both intensely long for and intensely fear the symbiotic merger with another. She believed that such a predicament most commonly emerged as the result of early childhood relational confusion and injury associated with the child’s primary caretaker, which is most often the mother (and hence her coining the controversial term, “schizophrenogenic mother.”) In 1964, Joanne Greenberg, a patient of Fromm-Reichman who experienced full recovery from a debilitating psychotic condition, published the bestselling book, I Never Promised You a Rose Garden, which offers a compelling autobiographical account of the potential for full recovery from long-term psychosis when such individuals are supported in repairing early childhood relational injuries.
In the 1950s, Gregory Bateson and his colleagues followed a line of reasoning similar in some ways to that of Fromm-Reichman, and after extensive research, proposed the “double-bind hypothesis” (Bateson et al., 1956). This hypothesis suggests that if the authority figures within a family (typically the parents) place the child in a double-bind by setting up conflicting injunctions so that it is impossible for the child to satisfy one without violating another, then a situation can result in which the child experiences such overwhelming distress that they are forced into a kind of psychotic reaction as a kind of extreme strategy to tolerate this otherwise intolerable situation.
Piggybacking off of the work of Bateson and his team’s double-bind hypothesis, R.D. Laing suggested that these kinds of interpersonal and intrapersonal binds that develop within dysfunctional family systems go on to create an incompatible knot, or untenable dilemma within the child that forces her to essentially “go mad,” which he saw as a profound transformation of the self resulting from a desperate attempt to resolve this otherwise irresolvable dilemma. After closely studying the family and social systems surrounding over 100 cases of individuals diagnosed with schizophrenia, he concluded that, “without exception the experience and behavior that gets labeled schizophrenic is a special strategy that a person invents in order to live in an unlivable situation [author’s emphases]” (1967, pp. 114-15). So Laing was one of the first in the West to emphasize the deeper wisdom and potential for positive transformation and renewal within the process of psychosis. Laing went on to write extensively on these topics, with The Divided Self (1961), Sanity, Madness and the Family (1964) and The Politics of Experience (1967) being among the most essential of these.
In the late 1940s and 1950s, Murray Bowen, a founding pioneer of family systems theory and therapy, came onto the scene as a leader in researching links between certain kinds of family dynamics and the development of “schizophrenia.” Among his most well-known family systems concepts is Differentiation of Self, which essentially refers to the capacity to experience a self as distinct from others, and particularly from one’s primary caretakers. He derived this concept during his years of working with those diagnosed with schizophrenia, when noticing that those so diagnosed typically developed an unusually poor Differentiation of Self.
Bowen also came to notice a significant pattern in which patients diagnosed with schizophrenia often improved when being separated from their families (typically when being placed in the hospital), but then deteriorated upon returning to their families. Subsequently, he became inspired to head an inpatient hospitalization project for the National Institute of Mental Health, in which he compared family members deemed “schizophrenic” with those considered “normal,” and concluded that:
. . . family members were involved in the [psychotic] process with the patient more deeply than had been hypothesized. Fathers were admitted to the family groups, and the hypothesis was extended to think of schizophrenia as a symptom manifestation of an active dynamic process that involved the entire family, and a plan was devised to treat the family as a single unit rather than individuals within a unit. (Bowen et al., 1960)
In this and his other work, then, Bowen contributed significantly to the idea that what is called “schizophrenia” is more appropriately seen as a problem existing broadly within the entire family system rather than simply existing solely within the “identified patient.”
In 1966, George Brown and his colleagues effectively demonstrated that “schizophrenia” patients discharged from the hospital and returned to family environments that have particularly high degrees of criticism, hostility and emotional dependency, are much more likely to return to the hospital. He coined the term “expressed emotion” or “EE” to describe this particular family dynamic, and found that patients from high-EE homes were about 6 times more likely to be rehospitalized than those from low-EE homes (Brown et al., 1966), a finding that has since been replicated numerous times. A later closely related study followed adolescents for 15 years and found that of those whose parents both scored highly on EE measures, 36% of them went on to become diagnosed with schizophrenia, whereas not a single youth became so diagnosed if one or both parents scored low on EE measures (Goldstein, 1987).
In the 70s, stemming directly from this earlier research and Laing’s Kingsley Hall experiment, we witnessed a movement towards the development of residential facilities whose aim was to provide the opportunity for young people grappling with psychosis to extract themselves from problematic family systems and live within social environments designed to maximize healthy relationships with others while offering support in resolving their psychotic crises and moving towards independence. The most well known of these is Loren Mosher’s Soteria home, which was originally established as a National Institute of Mental Health funded research project, comparing the recovery outcomes of such a home with those of mainstream “treatment as usual” (which primarily consisted of hospitalization and psychiatric drugging). This study demonstrated that the Soteria project was equal or superior to the standard treatment on every outcome measure studied, with a significantly higher percentage of Soteria residents going on to live independently with less psychiatric drug use and fewer rehospitalizations (Bola & Mosher, 2003).
Two other similar but lesser known “madness sanctuaries” developed in the 70s were Diabasis, designed and directed by John Weir Perry, and I-Ward, a project initiated by the Contra Costa County Hospital. Though less well researched than Soteria, the evidence suggests that these other homes were able to demonstrate very hopeful outcomes similar to those of Soteria. After reviewing the collective research on the outcomes of such homes, Mosher concluded that “85% to 90% of acute and long-term clients deemed in need of acute hospitalization can be returned to the community without use of conventional hospital treatment” (1999, p. 142).
Unfortunately, in spite of their success, all of these homes were closed due to a lack of funding, which Mosher and others have ascribed to an underhanded political assault by the psychopharm industry, as the existence of such homes clearly represented a potent existential threat to the psychopharm industry. Since that time, several other Soteria and Soteria-based homes have been established within the U.S. and Europe, but these have generally demonstrated less successful outcomes, due most likely to the fact that these more recent homes have been crippled by a mental health system that has become increasingly entrenched within the medical model paradigm. In particular, these more recent homes have generally not been trusted to receive people experiencing first-episode psychosis, they have often been forced to alter their approach in certain ways to conform more with the medical model, and they have often found themselves excessively burdened by being required to support individuals who have already received significant psychosocial injury from years of previous drug treatment and institutionalization (see this article by Dan Mackler for a more thorough analysis of these issues).
Beginning in the late 70s and through the early 90s, several other models that drew from a family systems perspective came onto the scene. In contrast to the Soteria-type homes, these programs consisted of trained facilitators who worked directly with the families (and extended social systems to various degrees) within the family’s natural environment. One such approach is Windhorse Community Services, which draws its guiding principles from the Tibetan Buddhist tradition, and attempts to foster the “basic sanity” and wisdom that underlie the chaotic system that has emerged within the mind of the individual and the broader family system. Windhorse continues to provide services in several regions of the United States, though remains generally marginalized by the mainstream system and forced to conform to some extent with the medical model philosophy and treatment approach.
In the late 70s, a team of Italian psychologists developed the Milan family systems approach to working with those diagnosed with schizophrenia, drawing particularly from Bateson’s work on the double bind theory, and developing what they called the “counterparadox” technique, which consisted of various ways to directly counter the entrenched double binds, or “paradoxical communication,” that had formed within such families (Selvini-Palazzoli et al., 1978). Drawing directly off of the work of both Bateson and the Milan team (as well as Russian philosopher Mikhail Bakhtin’s Dialogism; 1984), a group of mental health professionals in Western Lapland, Finland, developed the Open Dialogue approach, which involves a team of facilitators who work with the family in their own natural environment, and who create a space in which the principles of “tolerance of uncertainty,” “dialogism,” and “polyphony” are emphasized (Seikkula & Olson, 2003). In essence, this approach attempts to create a space in which all voices are heard, and any existing rigid right/wrong or true/false frameworks held within the family system are exchanged for one that is more open to multiple perspectives, with the idea being that such a space provides the fertile ground for genuine resolution and a more sustainable order of harmony to emerge. After documenting the outcomes of this approach for over 25 years, the Open Dialogue approach has demonstrated the best evidence-based recovery outcomes in the entire Western world, with over 80% of individuals experiencing a psychotic breakdown going on to experience full medication-free recovery. The Open Dialogue approach has recently begun to spread to other parts of the world, continuing to offer significant hope for individuals and families so afflicted.
Presumably due to the increasing dominance of the medical model paradigm in the later decades of the 20th century and up to the present day, research into problematic family dynamics and psychosis has become increasingly sparse. However, over the past 20 years or so, a closely related line of research has come into sharper focus—research into correlations between childhood trauma and the subsequent development of psychosis. In particular, a number of adverse childhood experiences have been shown to be highly correlated with the development of a psychotic disorder, particularly those listed in Table 1.
The findings of several such trauma-based studies have been particularly striking, essentially shattering any doubts people may still have about environmental and relational factors playing a major role in precipitating a psychotic condition in a young person. For example, a 2004 Netherlands study followed 4,045 participants who were initially free from psychotic symptoms for 3 years. They found that victims of child abuse were 9 times more likely to go on to develop psychosis, and that the victims of the most severe child abuse were 48 times more likely to develop psychosis (Janssen et al., 2004). And in 2007, a UK study went over the records of 8,580 participants to identify the correlations between a broader array of childhood trauma and psychosis. They found that individuals with 3 types of trauma were 18 times more likely to have subsequently developed a psychotic condition, and that those with 5 or more types of trauma were 198 times(!) more likely to have subsequently developed psychosis (Shevlin et al, 2007). In contrast, research into biological or genetic correlates for psychosis has not been able to establish degrees of correlation anywhere close to these (for a particularly comprehensive review of the literature on childhood trauma and psychosis, see Read et al., 2008).
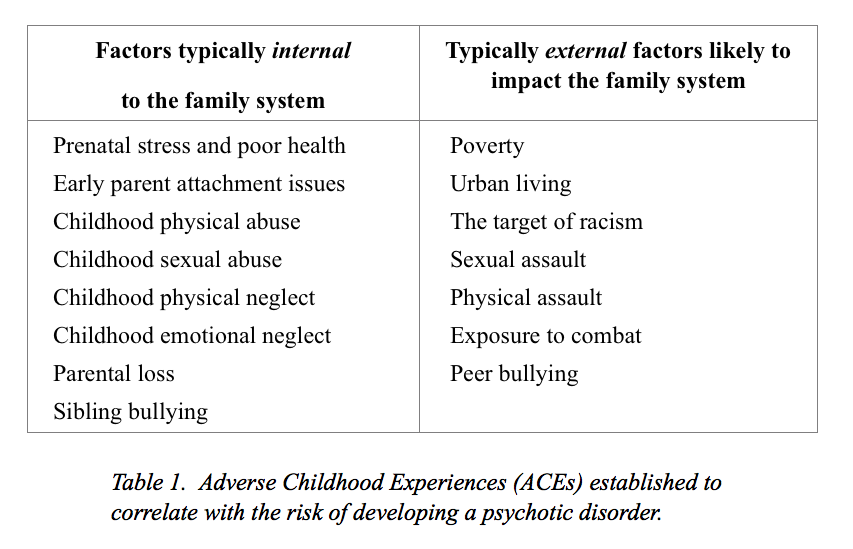
Note that one factor not listed in Table 1 in spite of significant correlations with the onset of psychosis and other extreme states is the use of psychoactive drugs, including both recreational drugs (such as cannabis and methamphetamines) and most major classes of psychiatric drugs. I didn’t include this factor in the table, however, since drug use doesn’t typically represent an adverse childhood experience in itself, but rather is generally best seen as a common response to the distress caused by such experiences, as psychoactive drugs can often provide temporary relief from such distress. There is a painful irony in using such drugs to ameliorate distress, however—although they may provide significant relief in the short term, they actually increase the likelihood that the person will go on to develop psychosis and other distressing states of mind further down the road (see Whitaker’s Anatomy of an Epidemic or my own Rethinking Madness for more about this).
When looking at the list of childhood traumas in Table 1, it’s easy to see that all of them are either directly related to serious problems within the family system, or at least directly impact upon them. So looking more closely at this list, and at the types of problematic family dynamics that have been implicated within the research mentioned above, a very important question emerges: What do all of these have in common? In other words, is there some common denominator that all of these types of trauma and patterns of problematic family dynamics share, a single underlying factor that makes someone particularly vulnerable to experiencing a psychotic breakdown? Indeed, I believe that there is, which will be the topic of exploration in Part Two.
* * * * *
References:
(for all three parts of the article)
Bakhtin, M. (1984). Problems of Dostojevskij’s poetics. Theory and history of literature: Vol. 8. Manchester, UK: Manchester University Press.
Bateson, G., D. Jackson, D., Haley, J., & Weakland, J. (1956). Toward a Theory of Schizophrenia. Behavioural Science 1, pp. 251-54.
Baumrind, D. (1989). Rearing competent children. In W. Damon (Ed.), Child development Today and Tomorrow. San Francisco: Jossey-Bass.
Berry, K., Barrowclough, C., & Wearden, A. (2007). A review of the role of attachment style in psychosis: Unexplored issues and questions for further research. Clinical Psychology Review, 27(4):458-475.
Bola, J., & Mosher, L. (2003). Treatment of acute psychosis without neuroleptics: Two-year outcomes from the Soteria project. Journal of Nervous and Mental Disease, 191(4), 219-229. doi:10.1097/00005053-200304000-00002
Bowen, M. (1960) A family concept of schizophrenia IN D.D. Jackson (Ed.) The Etiology of Schizophenia. New York: Basic Books.
Bowen, M. (1993). Family therapy in clinical practice. Lanham, Maryland: Rowman & Littlefield Publishers, Inc.
Bowlby, J. (1969). Attachment and Loss, 3 vols. London: Hogarth, 75.
Brown, G.W., Bone, M., Palison, B. & Wing, J.K. (1966) Schizophrenia and Social Care. London: OUP.
Fromm-Reichmann, F. (1948) Notes on the development of treatment of schizophrenics by psychoanalysis and psychotherapy. Psychiatry, 11, 263-273.
Furnham, A., & Cheng, H. (2000). Perceived parental behavior, self-esteem, and happiness. Social Psychiatry and Psychiatric Epidemiology, 34(10, 463-470.
Galambos, . L. (1992). Parent-adolescent relations. Current Directions in Psychological Science, 1, 146-149.
Goldstein, M. The UCLA High-Risk Project. Schizophrenia Bulletin 1987; 13(3):505-514.
Greenberg. J. (1964). I never promised you a rose garden. Chicago; Signet.
Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, de Graaf R, et al. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatrica Scandinavica 2004;109(1):38-45.
Karen, R. K. (1994). Becoming attached: First relationships and how they shape our capacity to love. Oxford, UK: Oxford University Press.
Laing, R.D. (1960) The divided self: An existential study in sanity and madness. Harmondsworth: Penguin.
Laing, R.D. and Esterson, A. (1964) Sanity, madness and the family. London: Penguin Books.
Laing, R.D. (1967). The politics of experience. New York: Pantheon Books.
Miklowitz, J.P. (1985) Family interactions and illness outcomes in bipolar and schizophrenic patients. Unpublished PhD thesis, UCLA.
Mosher, L. R. (1999). Soteria and other alternatives to acute psychiatric hospitalization: A personal and professional review. The Journal of Nervous and Mental Disease, 187, 142-149.
Napier, A.Y. & Whitaker, C.A. (1978; 1988). The Family Crucible. New York: Harper & Row.
Neufeld, G., & Mate, G. (2014). Hold on to your kids: Why parents need to matter more than peers. New York: Ballantine Books.
Norton, J. P. (1982) Expressed Emotion, affective style, voice tone and communication deviance as predictors of offspring schizophrenic spectrum disorders. Unpublished doctoral dissertation, UCLA.
Read, J. (2004). Poverty, ethnicity and gender. In J. Read, L. R. Mosher, & R. P. Bentall, (Eds.), Models of madness: Psychological, social and biological approaches to schizophrenia (pp. 161-194). New York: Routledge.
Read, J., Fink, P., Rudegeair, T., Felitti, V., & Whitfield, C. (2008). Child maltreatment and psychosis: a return to a genuinely integrated bio-psycho-social model. Clinical Schizophrenia & Related Psychoses, 2(3), 235-254.
Read, J., & Gumley, A. (2008). Can attachment theory help explain the relationship between childhood adversity and psychosis? Attachment—New Directions in Psychotherapy and Relational Psychoanalysis, 2(1):1-35.
Resnick, M. D., Bearman, P. S., Blum, R. W., Bauman, K. E., Harris, K. M., Jones, J., … & Udry, J. R. (1997). Protecting adolescents from harm: findings from the National Longitudinal Study on Adolescent Health. Jama, 278(10), 823-832.
Seikkula, J., Aaltonen, J., Alakare, B., Haarakangas, K., Keränen, J., & Lehtinen, K. (2006). Five-year experience of first-episode nonaffective psychosis in open-dialogue approach: Treatment principles, follow-up outcomes, and two case studies. Psychotherapy Research, 16(2), 214-228. doi: 10.1080/10503300500268490.
Seikkula, J., & Olson, M. E. (2003). The open dialogue approach to acute psychosis: Its poetics and micropolitics. Family process, 42(3), 403-418.
Selvini-Palazzoli, M., Boscolo, L., Cecchin, G., (1978). Paradox and counterparadox. New York: Jason Aronson.
Shelvin M, Houstin J, Dorahy M, Adamson G. Cumulative traumas and psychosis: an analysis of the National Comorbidity Survey and the British Psychiatric Morbidity Survey. Schizophr Bull 2008;34(1):193-99.
Siegel, D., & Hartzell, M. (2003). Parenting from the inside out: How a deeper self-understanding can help you raise children who thrive. New York: Tarcher/Penguin.
Siegel, D., & Payne, T. (2014). No-drama discipline: The whole-brain way to calm the chaos and nurture your child’s developing mind. London: Scribe.
Whitaker, R. (2010). Anatomy of an epidemic: Magic bullets, psychiatric drugs, and the astonishing rise of mental illness in America. New York, NY: Crown Publishers.
Williams, P. (2011). A multiple-case study exploring personal paradigm shifts throughout the psychotic process, from onset to full recovery. (Doctoral dissertation, Saybrook Graduate School and Research Center, 2011). Retrieved from http://gradworks.umi.com/34/54/3454336.html
Williams, P. (2012). Rethinking madness: Towards a paradigm shift in our understanding and treatment of psychosis. San Francisco: Sky’s Edge Publishing.
Wynne, L.C., Ryckoff, I.M., Day, J. & Hirsch, S.I. (1958) Pseudomutuality in the family relations of schizophrenics. Psychiatry, 21: 205-220.












This is a great article Paris. I always like how courageous you are in bluntly and directly addressing these controversial issues.
As I’ve noted in other comments, it is pretty obvious from the type of studies you referenced, and from common sense, that poor parenting of all forms can and does contribute to increased risk for “schizophrenia”, i.e. psychotic breakdown. Abuse and neglect cause psychological stress, psychological stress increases the risk of someone being overwhelmed emotionally, and in extreme cases this can lead to psychotic symptoms. It’s pretty logical and the data from John Read, ACE study, etc back it up. I remember in John Read’s interview at UCLA recently he was saying that over 50 separate studies are now showing strong links between trauma, abuse, and development of psychosis.
As Donald Winnicott noted, schizophrenia or psychosis can be viewed as the negative, or mirror image, of the healthy process of increasing security and trust which develops between skilled parents and well-supported children.
It is sad to see NAMI parents saying that poor parenting can’t possibly cause schizophrenia… when sometimes, these are ironically some of the very parents whose neglect, poor parenting skills, and abuse, will have partially contributed to their children’s having a breakdown and getting diagnosed with schizophrenia. One can understand how it’s more comfortable for such parents to delude themselves into believing that they are good parents, and their children’s whole problem is one of faulty brain chemistry and genes (which isn’t very flattering to parents, either).
But the notion that parents should be blamed if they contribute to their children’s psychosis is simplistic and wrong; of course they shouldn’t be blamed. Trauma can be passed down through generations and there is no one person to blame, only problems to be understood. Understanding and acknowledging how parents contribute to psychosis risk can actually be a positive thing because it can allow for change, prevention, and repairing relationships. Deluding oneself that schizophrenia is a brain disease, on the other hand, usually dooms the young person to a life of being drugged and viewed as a chronic invalid. That is unfortunately what happens today to most young people unfortunate enough to be caught in this very unfair situation involving multiple lies about what is known about so-called schizophrenia, told by psychiatrists and our System.
Report comment
Paris, I want to note that your writing appears to me (I have read all of Rethinking Madness) to be mostly missing one major area of hopeful research… Fairbairnian and Kleinian psychoanalytic approaches to psychosis (what a mouthful!).
You mentioned a couple of these in your book (referencing Silvano Arieti) and in this piece, referencing Freida Fromm-Reichmann.
If you haven’t read them in depth, I recommend to you the writers Harold Searles and Vamik Volkan. Their insights into psychosis are truly profound, and their case studies fascinating.
Searles has the four phases of schizophrenia recovery: Out of Contact, Ambivalent Symbiosis, Therapeutic Symbiosis, and Individuation. For him these phases he encountered in working with schizophrenic patients reversed, or cured, the pathological regression or negative sequence of emotional development that occurred between the psychotic-child-to-be and its early world/parent figures. I recommend his chapters such as “The Mother Transference” (about how conflictual feeling surrounding the psychotic client’s parents get transferred to the therapist) and “Intensive Psychotherapy of Chronic Schizophrenia, A Case Report” which give a great insight into how parental and family relationships contributed to the development of the psychosis and how replaying and modifying these interactions can lead to healing. These essays are in his collections, Collected Papers on Schizophrenia and Related Subjects, and Collected Papers on Counterference and Related Subjects, available on Amazon.
Volkan is technical and hard to read but, in my opinion, is the best and most insightful writer on how to work intensively with severely psychotic people. He writes about how abuse, trauma, and neglect can lead to organismic terror and horror, and the need to defend against these extreme emotions lead to the creation of a subself (a container of developmentally early representations of oneself and others) that he calls the “infantile psychotic self”.
This infantile self arrests the personality in a kind of twilight zone in which the psychotic part in its terror produces delusions, hallucinations, and bizarre thoughts. Meanwhile, the “uninvaded self” – the fragmentary but slightly more mature self-and-other images surrounding the infantile psychotic self structure – attempt to maintain a modicum of a relationship to the external world, but are unable to cope with the primitive overwhelming affects of terror, rage, and despair during difficult periods. The archaic (developmentally early) self-and-other images in the infantile psychotic self have to be painstakingly matured and modified in relation to the therapist or another person or entity, in order to help the person become non-psychotic.
Volkan’s cases of Attis, the delusional “Would-Be-Wife Killer” who later came to be a beloved community priest when he was no longer psychotic, and Jane, the psychotic girl who reminded Volkan of Tarzan’s bride and later became a renowned painter, are truly incredible reading; they are in the book The Infantile Psychotic Self and Its Fates.
The last therapist I want to recommend to you is the Italian Gaetano Benedeti, and his writing in such books as Psychotherapy as Schizophrenia. His long-term study of 50 schizophrenic clients given psychotherapy an average of 3x/week for 5 years, that he did with Pier-Maria Furlan, is particularly interesting and hopeful.
Another writer at these one’s level, if you need more reading, would be Bryce Boyer, e.g. The Regressed Patient. There are many others found in the references of these books.
Also, I have never seen you cite the document I link below, but I think it’s among the most important I’ve read about psychotherapy and psychotic conditions – William Gottdiener’s metaanalysis of 37 studies containing 2,642 people labeled schizophrenic who were in psychotherapy an average of 20 months, 1.5 times a week. A big mix of studies, but most of them were long-term psychotherapy, and the effect size was quite large and robust, favoring psychotherapy as helping people with psychosis be much better off (in other words, obviating the need for the recent RAISE study). The main finding is that 20 months of psychotherapy made psychotic people almost twice as likely to recover as those who didn’t receive therapy. Gottdiener explains the statistical measures better than I can.
Here’s a paragraph you might find of interest: “When antipsychotic medication was used with individual psychotherapy the mean effect size was r = .31 (95% CI + .19 to .42). When antipsychotic medications were not administered with individual psychotherapy the mean effect size was also r = .31 (95% CI + .12 to .48). The corrected effect size and BESD results for psychotherapy with medication and without medication was the same…..
It is surprising that the proportion of patients that were likely to improve without conjoint medication, is similar to the proportion of patients that were likely to improve with a combination of individual psychotherapy and antipsychotic medication. This finding is contrary to most therapists’ clinical expectations. The finding that individual psychotherapy can be effective without medication is not new (see Karon & VandenBos, 1981). However, it is important because it suggests that individual psychotherapy alone might be a viable treatment option for some patients who do not improve from treatment with antipsychotic medications, for some patients who refuse to take medications, or for patients who are treated by therapists that choose to use little or no adjunctive medication. ”
I was not at all surprised by this, but I’m sure most psychiatrists would be.
http://psychrights.org/Research/Digest/Effective/BGSchizophreniaMeta-Analysis.htm
Report comment
Hi bpdtransformation,
I’m glad to hear you enjoyed the article. I’m impressed by your breadth of knowledge(!) Thanks for your suggestions of readings–I’m familiar with some but certainly not all of them, and look forwad to following some of these leads.
You commented:
“But the notion that parents should be blamed if they contribute to their children’s psychosis is simplistic and wrong; of course they shouldn’t be blamed. Trauma can be passed down through generations and there is no one person to blame, only problems to be understood. Understanding and acknowledging how parents contribute to psychosis risk can actually be a positive thing because it can allow for change, prevention, and repairing relationships.”
I just want to say that I couldn’t agree with you more about this, and I hope I didn’t come across in this part suggesting that we take a stance of “blame and shame” towards the parents. I actually will be discussing this very issue in more detail in the next two parts (especially Part Three) of this article. In particular, as you say, all of us (parents included, of course) are embedded within social systems that are very wide (extending out to our extended family, community, nation, and all of the human society) and very deep (extending back through many generations). So as we raise our children, we bring all of this with us–the beliefs and pressures of “wider” and the “deeper” social systems–but we are often oblivious that we are doing so. So when we find that our family system is struggling (and they virtually all struggle at times), as you suggest, the first and most critical step to is become curious about what kind of beliefs and behaviours are present here, where do they come from, and how can we shift towards something more harmonious and wholesome..? So shifting from an attitude of “blame” to “openness, curiousity, humility and shared responsibility.”
Thanks for your comments,
Paris
Report comment
Paris, thank you and no I did not ever think you intended a blame or shame approach. My comment regarding the simplistic nature of blaming parents was covertly directed toward those groups who fraudulently hold that identifying parents as contributors to a child’s receiving a schizophrenia diagnosis constitutes blaming: some NAMI members, the APA, most American psychiatrists, and the disease model in general.
Report comment
Thanks for the clarification, BPDTransformation. Good point about the way people (like myself, you and others) who encourage parents and society to consider the harm that problemtic family dynamics may cause are then vilified themselves–a common derogatory term I have found used to try to shut people like us up is referring to us as “mother blamers.” A frustrating and very “head in the sand” response, to say the least (!) I’ll say a lot more about this issue in Part Three.
Paris
Report comment
Thank you for stating your definition of “psychosis” but for me there was nothing existential about my emotional distress; my experience were a living nightmare and caused unbelievably painful emotional distress.
I think that distressful experiences cause “psychosis” and that parents are a primary cause of distressful experiences but they are not the only source of distress. Good parents are getting involved in harmful support groups with good intentions defend themselves from blame along with bad parents who are there doing the same.
Best wishes, Steve
Report comment
Thanks for sharing a bit about your own experiences, Steve.
To clarify, I certainly have no intention to “romanticize” psychosis (if that’s what you have taken away from my words). To the contrary, having dipped into these waters myself, I agree that it is very difficult to convey to others who haven’t experienced this kind of thing the intensity of pain, terror, confusion, etc., that can go along with such experiences. I simply have a lot of faith in “organismic wisdom,” that as long as we are alive, some part of us will continuously strive for health and wholeness, although whether this is actually attained is a different matter. Also, by “existential,” I’m simply referring to the basic core dilemmas inherent in our existence–difficulties and challenges that we all face, so long as we are alive, and of course learning how to work with the inevitable pain and confusion of life is part of this (I’ll be saying much more about this in Part Two of this article).
Best regards,
Paris
Report comment
Thank you, Steve
Report comment
I think when a child’s natural behavior indicates that they are challenging the norms of the family, how parents react and respond to this makes all the difference. If they shame, punish, or guilt the kid for going against the grain in a way that does no one any harm–and in fact, which gives opportunity for growth in the family– but it’s simply different than what the family dogma would dictate, then there will be rebellion and power struggles, perhaps leading to depression and anxiety, at the very least, due to feelings of being emotionally coerced into compliance. Families can be like a cult, if the dynamics exist to appease abuse and dysfunction. We need permission to be ourselves, for health and well-being to occur.
However, if parents can welcome the challenge because they expect to be challenged by their children, and they know how to set healthy boundaries while giving permission for the kid to explore their nature, even if it goes against their grain, then I feel there will be a better outcome in the clarity and confidence of the child. The child may fall and have to get up again, but that’s part of growth and learning self-resourcefulness and self-care.
I’m not saying it’s not a challenge for parents, who are also human and who come with their own baggage. But I think there is a clear line between a child who is allowed to explore their nature and one who is shamed, demeaned, and ostracized for being themselves, or even for having a need, when these should be totally expected. Parents may have issues, but they are the adults and influence kids in every way, first and foremost. How they set the example for how to deal with their personal issues and the shit in the world is what the kid will most likely internalize and repeat, when they experience life’s challenges.
It’s a delicate balance, but I think raised awareness around the issues of parenting and control are always helpful to all concerned. After all, what we learn in our families is what we bring to our communities, these are direct reflections of each other. Social healing is the order of the day, imo.
Report comment
Actually, regarding the personal issues of the parents, when a kid challenges them and they feel angry and blaming about that, that is a PERFCT opportunity to work on their issues. Blame the child for challenging them? I don’t think the child is at all at fault, no way they can be. It’s their job to challenge parents.
Great growth and healing opportunities for all concerned, if we stay out of (or work through or ascends, however one wants to put it) judgment, blame, and guilt. Everyone makes mistakes, we needn’t punish ourselves for them, nor punish others for making them. Better to simply correct them and move on in a new way. That’s how we evolve forward.
Report comment
I think these are all really good points, Alex. They speak directly to what I’ll be discussing in Part Three of this article–towards effective parenting and communication. I’ll look forward to any feedback you may have on that section, if you’re so inclined.
Best wishes,
Paris
Report comment
Thanks, Paris. I definitely look forward to the next parts.
Family healing was core to my own healing and personal transformation. I was the ‘truth-speaker’ (and forgiver) who challenged the family system in every way, and for a while, it was hell to pay, and, indeed, it was literally crazy-making.
But I worked with these issues for years to find a delicate balance, where I honored from where I came without giving myself over to values which were not meaningful to me–and which in fact, were stigmatizing and wounding to me, as a child–and I was finally able to unearth and dismantle what I had internalized from the family dogma, so that I could achieve the emotional freedom to walk my soul path of truth, which has proven to be extremely beneficial healing in every way imaginable.
Family healing is a remarkable and enlightening journey of personal discovery and integration. I’m so happy you are writing about this, specifically, I feel it is extremely valuable and supportive to changing the world. It is the core of our society.
Report comment
Hi, Alex,
There are all kinds of children, and I feel I need to point out that it is not just the “challenging” children who may end up with a diagnosis of ‘schizophrenia.’ In fact, IMO, they may be in the minority, but they are the vocal Majority of people who blame their condition on childhood trauma. Consider, the quiet, obedient child who challenges nobody. The guy or girl who passes under the radar. There’s a lot of stereotyping at MIA that it’s the rebels who become schizophrenic because they’ve been at the receiving end of their parents anger. Not necessarily the case. Perhaps these quiet ones “wake up” around their late teens and decide that being a passive observer of life is now their biggest challenge to overcome.
Just my thoughts, based on my experience.
…Rossa
Report comment
Excellent point; thank you for giving voice to quiet sufferers.
Best wishes, Steve
Report comment
Point taken, Rossa.
I guess I was talking about kids that do challenge their parents–not just with aggressive behavior and the like, but simply by choosing a different path than what parents intended and expected. That was my situation, and I speak from that experience. I also know a lot of people–both in person and also a lot of people that I’ve read about, famous people–who tell about going against the grain of their parents’ wishes for them, and the problems that it caused in the family.
Am I saying this causes something which could be DSM diagnosed? Not necessarily, but often it is, and at the very least it causes distress that can manifest and play out in a variety of ways.
I hear this is not your experience, that you are coming from a different dynamic. I appreciate your experience.
I don’t feel I’m blaming anything on anyone, simply providing a perspective from my own experience and from what I know about others, my work with clients, my friends, etc. Sorry if it comes across as blaming. I do feel parents play a role in how their kids embrace adulthood, but that is a long and complex discussion of generational patterns and contracts, cause-and-effect, and how we influence each other energetically.
Thanks for your feedback, I’ll keep in mind how I express myself.
Report comment
And not just a different path, come to think of it, but who develop different values, etc. Really, going against the grain of the family value system and choosing one’s own way of doing life, is really what I’m talking about–being made to feel guilty or selfish for being independent from the family. That’s a very common double bind which, indeed, causes internal emotional conflict, and potential suffering for the adult child, until they claim their freedom by simply not caring about the naysayers.
Report comment
Hi, Alex,
I don’t feel you were parent blaming in what you wrote. I just felt I had to point out that it’s often the quiet ones, the ones who never rocked the boat, who end up the dreadful “S” label. So, no need to write with everyone in mind. You’re experience is what counts for you.
Best,
Rossa
Report comment
Ah, ok, thanks Rossa, I did misinterpret, thanks for clarifying and of course I totally agree with you, that there is a wide spectrum here. Indeed, all voices need to be heard, from these different perspectives and experiences.
I’m kind of chuckling to myself, here, because I can have trouble discerning here online whether I’m being accused of being or saying something, or if something is being added to the conversation in a neutral way. I’m just so accustomed on here of being called out for something. Especially this topic, regarding families and parenting. I totally understand the challenge of that.
I guess some people know I made a film about stigma and discrimination. My assertion is that, for a lot of people, (not all, but still common, I think), this begins in the family. So for the film, I asked everyone about their family relationships (given that my family dynamic was totally instrumental in my falling into the psychiatric pit), and I got some very interesting answers.
These are 6 diverse voices–different walks of life, different personalities, different experiences, different perspectives– and in fact, one of the women in the film was what you are calling ‘the quiet one,’ and she talks about what happened to her when she was hospitalized in a very articulate and moving way, I think.
Our experiences of childhood turned out to have some overlap and also a lot of differences, we were on a continuum.
Check it out if you wish, this is all about family influence on our mental health, and then what happens when we give it over to the system. And yes, some people have trouble sitting through this, specifically because the family issues make them uncomfortable. Still, it is without a doubt vital to explore this, so I broached it without apology, as directly and sensitively as I knew how–
https://www.youtube.com/watch?v=AtDGxJWmj5w
Report comment
My thoughts too, based on my experience, and Laing too seemed to think that the good obedient child was more likely to have problems along the road. I understood from his writings (Divided Self) that although the teenage years make evident the problem, the problem started way back in the formative years i.e. conception to age two or three. If the self isn’t formed properly then (yes, because of faulty parenting) then there is no strength for rebellion later. Open rebellion is so much healthier than rebellion turned in, attacking the fragile self – not just psychosis but also anorexia and probably other examples too.
It’s particularly tragic because these are the children who so longed for acceptance throughout, tried their best to be good, and then in the end, still can never measure up and on top of everything, when they finally fall apart under the strain, are blamed for bringing disgrace, expense, worry etc. to the family and told that they’re crazy.
Jewish tradition teaches that parents are supposed to look at the things in their children that bother them the most, and see them as reflections of their own imperfections – i.e. the parents are the ones who are supposed to change as a result. This is also true between spouses.
So, i am not so quick to exonerate parents and say, “Poor things, they did the best they could.” Maybe they did, but when the tragic results become evident and they still don’t examine themselves to wonder how such a thing happened, then they deserve, to my mind, a measure of condemnation.
Report comment
Great piece! Thank you to the author and all those that took the time to make useful comments. Very useful.
Report comment
Dear Paris, I really love the depth, research and innovative thought that you have put into your work. Since you are being so thorough, I can’t help but wonder if you are skipping too quickly over particularly extreme context of today’s society for young people.
The use of psychoactive drugs, both recreational AND psychiatric/prescribed is not just a common response to distress used to provide temporary relief but it’s increasingly part of young people’s culture of experimenting, gaining street cred and even “independent” economic support through “disability” for those who feel little hope for finding meaningful work with fair wages. Are you aware of the way the Hunger Games books and movies speak to younger people. These are extreme times in their reality and imaginations.
Report comment
Hi Diana,
I’m glad to hear you’re enjoying the article, and thanks for your insightful comments.
As I mentioned above, it’s a bit tricky breaking the article up into 3 parts like this, as much of the comments are pointing to issues I discuss in the later parts, such as yours here. If I’m understanding you correctly, you’re wanting to make sure we acknowledge the importance of the broader social networks and how they impact families and the development of youth. I couldn’t agree with this more. Although I’m primarily discussing the nuclear family in this article, families are embedded deeply within the broader social networks–so just as a child is embedded in a family, the family is embedded with the community, the community within the nation and broader human societies. In order to support the individual who is really struggling, we have to recognize that this individual is really just a canary in a coal mine, pointing not only to the problems within the family, but also to those within the broader society (and they are many!). I discuss this further in my article here, which you may enjoy:
https://www.madinamerica.com/2015/06/can-madness-save-the-world/
Best wishes,
Paris
Report comment
Your theory that psychosis is caused by distress alone does not explain why many people experiencing extreme distress do not become psychotic. If psychosis was caused by distress alone, one would expect high levels of psychosis in war fields and refugee camps but this has never been the case. Distress is known to be a factor in many illnesses including heart disease and cancer. It appears to be a factor in mental illness but is certainly not the only cause, maybe not even a primary cause in many cases.
In my many years of meeting with people who suffer from mental illnesses and their families I have met some who were traumatized but also many others who had very normal, mundane lives. Some became psychotic after suffering from viral illnesses or using certain drugs such as SSRIs. Others became psychotic after going without sleep or going on extreme diets. Some have family members who have mental illnesses, others do not. There appear to be many causes of mental illness and endless debates about causes seem to be doing little to alleviate suffering.
I would love to see more research on what works to give sufferers relief rather than more debate on the causes of the suffering.
Report comment
“I would love to see more research on what works to give sufferers relief rather than more debate on the causes of the suffering.”
You might check out the link I gave in my comment above, to Gottdiener’s metaanalysis of psychotherapy for psychosis. Also, check out the books Treating the Untreatable (Steinman), The Infantile Psychotic Self (Volkan), Recovery Sanity (Podvoll), and Weathering the Storms (Jackson) for some fabulous case studies of chronically schizophrenic individuals who were healed. You can get them used on Amazon.
Regarding your comment, I think Paris’ studies linked above are quite convincing in making the case that trauma, abuse, neglect, and poor parenting in general are one of the main, if not the main, factor contributing to psychosis / getting a schizophrenia diagnosis. John Read has many more of these studies if you look up his work.
I would say the idea that “psychosis may be caused by distress alone” may be misleading or out of context. I believe that distress alone is not enough; there also needs to be preexisting vulnerability – this can be the case for a developing child or young person simply by virtue of the emotional stage they are at. Or there also needs to be distress/trauma that is long and severe enough to wear down a strong personality to the point where it is vulnerable. If you read the developmental theorists like Searles or Volkan, I think it helps to understand these processes of personality development or regression better.
In a war zone or refugee camp, many of the people will have had relatively stable families growing up, and although they are suddenly thrust into an overwhelming situation, their previously non-psychotic personality organization is usually strong enough to weather the extreme stress, as long as it doesn’t go on too long. On the other hand I think that many, many of our veterans do get given serious diagnoses of whatever “mental illness”, misnomer as that is, when the return from the war zones.
By contrast, perhaps you are aware of the studies that show that almost anyone, if kept in solitary confinement / supermax prison conditions long enough without any access to their fellow human beings, will begin to show signs of schizophrenia after several months of complete isolation. This shows that even the strongest personality can break down into psychosis given long and severe enough neglect and isolation.
Also, we should be clear that psychosis is not an illness, but a complicated syndrome or related constellation of psychic experiences. As far as we know currently, there are no illnesses that are mental. Real brain diseases on the other hand are things like Alzheimer’s and dementia.
Report comment
Very well stated, BPD
Report comment
I think I see where you are going. While it’s true that many, many people who experience psychosis have suffered trauma, to assume that ALL have would not explain the phenomenon in its entirely. (I have not, personally experienced anything I would consider traumatic but I have certainly departed from consensus reality. I didn’t consider these to be learning experiences, though I understand they can be.) If I had to shoehorn myself into the model in the article, I suppose putting “trauma” on a spectrum, maybe my threshold for being traumatized was extremely low given my basic personality and temperament, and my rather average childhood (which produced siblings that are well adjusted) was somehow devastating to me subconsciously? Then again, trying to fit the details of my life into models that don’t apply is how I got stuck in psychiatry in the first place.
Report comment
I totally agreed with you until I experienced an extended period of extremely distressful experiences; thereafter, I realized that we have little understanding of the experiences of others. Prior to trauma, I believe that my experiences were “average” and that my successes in life were substantially attributable to a better “inherited” mind/brain. I considered distressful “events” as small hurdles to overcome in an exciting journey through life. After trauma, my experiences took a different path and became predominately distressful. Distressful “events” became part of a pattern of painfully distressful experiences that exemplified my painful plight with an increase in emotional pain. People perceive of distressful “events” differently because of personal histories of experiences that are impossible to qualify or quantify for research.
Understanding that distressful experiences cause of mental distress (emotional distress) is the key to improving “mental health” care. Believing that emotional distress is a “mental illness” is the reason that mental health “care” is so harmful.
Best wishes, Steve
Report comment
Good points, madincanada and BPDTransformation,
A particular framework that I think really speaks to this is that of an holistic organismic one. In other words, I think that we (the collective we, as a society) make a mistake by trying to compartmentalize various kinds of experieces (mind vs. body, environmental vs. biological, physical toxins vs. relational toxins, etc.). If we consider the organism as a whole, then we recognize that any state of distress (whether it be “biological” illness or “psychological distress”) represents that this organism is struggling to meet certain basic organismic needs, and is simply responding in the best way that it can to try to meet these, to survive and hopefully thrive. So whether someone is experiencing cancer or a flu, or so called “psychosis,” “depression,” “autism,” etc., we can say that what we are basically seeing is a desperate organismic response to some barrier(s) that are interfering with it meeting its basic needs; and the challenge as supporters is to support the person in idenetifying where these barriers are coming from (often from more than one domain) and in working with (rather than against) this basic organismic wisdom of the being to facilitate recovery. What makes what I’m calling psychosis a bit different than the other kinds of organismic responses is that I believe psychosis represents the organism’s attempt to radically transform its basic cognitive constructs (its lens through which it perceives and interprets self and the world) in order to surive what is experienced as an overwhelming threat to the self at a very core existential level–yes, certainly a very risky and haphazard strategy, but one that I believe does have potential to lead to very powerful healing and transformation if successful, and not only for the individual, but also possibly for the larger social networks (indigenous cultures generally understand this, and therefore value individuals who go through such paradigm transforming experiences).
For more of my exploration on the “holistic organismic paradigm,” see:
http://www.madinamerica.com/2013/06/rethinking-mental-health-part-1-from-positivism-to-a-holisticorganismic-paradigm/
…and
http://www.madinamerica.com/2013/07/rethinking-mental-health-part-2-towards-a-needs-based-system-of-diagnosis-and-support/
Paris Williams
Report comment
Paris,
This is a interesting set of ideas about organismic reactions… it is basically the same theory, in slightly different language, to what is in with Vamik Volkan’s book The Infantile Psychotic Self. Volkan called the response to existential terror “organismic panic” and the attempt to reach a better equilibrium “psychobiological push”, if I remember it correctly.
His book has great analyses of the relational and psychological-defensive factors that prevent the self structure, in “schizophrenia”, from reaching a healthier non-psychotic equilibrium. Unless the psychotic fears are exposed and worked through, they tend to reoccur in a circular manner and to keep killing off the possibility for having better relationships by maintaining a close psychic system of distorted self-other perceptions… in psychoanalytic language, the self and object relations of a psychotic person do not evolve/mature but instead remain stuck in a cycle of fusing with and separating from other distorted all-bad self/other images.
In a successful therapy an initially psychotic person can reach a symbiotic (borderline) level of relationships and then later a neurotic/healthy level of object relationships. At a certain point in the process they are able to face the original terror and conceptualize it in a healthier, less infantile way; this brave step dissolves the infantile psychotic self and allows for progress to the “crucial juncture”, the psychological place at which all-bad and all-good perceptions can become more integrated.
In Searles’ language, they can progress through the early developmental phases, from out of contact to ambivalent symbiosis to therapeutic symbiosis to individuation, in this way retracing and reversing the pathological regression that occurred after the trauma, when the person who wanted their needs met was instead traumatized and retreated in terror into ambivalent symbiosis and/or out-of-contact phase (also called “autism”, meaning something different from the DSM label).
I encourage you to check out the books by Volkan, Searles, and their colleague Bryce Boyer, it can add another dimension of understanding to your writing and your practice.
Report comment
Paris,
Thank you for this history and analysis of the family’s role in extreme experiences. One of my sons went through a 2 week extreme experience 18 months ago using an Open Dialogue approach. He has not returned to this difficult state which seemed to have been related to extreme worry and stress, a history of bullying, parental divorce, difficulties related to some developmental challenges and severe existential concerns. You helped me with some suggestions at the time and I will be forever grateful for your support.
I agree with you that family experiences and dynamics are a big factor in the development of psychosis and that they need to be included in our understanding and response to these experiences. Furthermore, trauma is pervasive and come in many forms, often beyond the nuclear family. I am convinced that trauma in all it’s forms must also be considered as a cause. Beyond these, development, growing up and life itself are difficult. Psychosis may be an attempt to cope with and make sense of something beyond comprehension.
Your work is so important. Thank you
Report comment
Thanks for your comments, “Truth in Psychiatry,”
I am really glad to hear about your son’s successful working through of his crisis. Thanks for sharing this.
I also appreciate your wanting to make sure we acknowledge the broader context and social systems, and as I just mentioned in my comments to others above, I couldn’t be in more agreement with this(!) as I’ve discussed elsewhere, such as in the following two articles:
https://www.madinamerica.com/2013/05/the-mental-illness-paradigm-itself-an-illness-that-is-out-of-control/
https://www.madinamerica.com/2015/06/can-madness-save-the-world/
I am focusing primarily on the nuclear family in this particular article, but we absolutely need to acknowledge the severe limitations and stress placed upon such families trying to survive in a broader society that is so profoundly troubled (I’ll discuss this a bit further in Part Three).
Best wishes,
paris
Report comment
Truth in Psychiatry,
I agree with what you say.
Your son was out of the extreme experience in 2 weeks – if he had gone through psychiatry he might have been collared as a “schizophrenic” for the rest of his life (depending on the treatment and how he reacted to the ‘medications’).
I think there are probably lots of people that suffer terribly but don’t externalise, theres enough in normal life anyway to drive a person to crisis.
I think “schizophrenia” as a ‘diagnosis’ should be withdrawn because it’s use is very dangerous and open to manipulation (anyone could be diagnosed as a “schizophrenic”, if they were to confide their private thinking, from time to time).
Good luck in the future!
Report comment
Hooray! More of psychiatry’s and NAMI-families’ greatest nemesis: the TRUTH! Thank goodness for the Internet and social media. This may be Mad in America’s first article to go viral. Way to go, Mr. Williams!
Report comment
“Hooray! More of psychiatry’s and NAMI-families’ greatest nemesis: the TRUTH! Thank goodness for the Internet and social media. This may be Mad in America’s first article to go viral. Way to go, Mr. Williams!”
The TRUTH means or should mean “the whole truth and nothing but the truth.” Notably missing from the article is any mention of epigenetics.
Report comment
Hi GetItRight,
Thanks for bringing in the idea of epigenetics. While of course a complex and still far-to-be fully understood field, my understanding of what it essentially has been successful in doing is further reduce the viability of bio-reductionism (the idea that we are born with a rigidly constructed genetic “blueprint” and are fated to developing certain characteristics and/or “illnesses” according to this). And it further reinforces the viability of the role that trauma and core beliefs (often closely related to each other) play in determining the particular qualities we develop and the likelihood of cultivating wellbeing in our lives (or lack thereof). What I find is particularly fascinating with regard to the discoveries of epigenetics is that it reveals that Lamarck was probably a bit more right on than Darwin in recognizing that certain environmental experiences of an organism (i.e., trauma and other powerful experiences) can modify the organism at the cellular level (i.e., epigenetically) in a way that allows it to pass on certain learned responses/”core beliefs” to its offspring purely via genetic/epigenetic transmission. In other words, this field is reinforcing the long held common sense wisdom of intergenerational trauma—that it is passed down not only environmentally but also probably genetically. So rather than undermining our understanding of the importance of family (and broader systems) dynamics, I see the field of epigenetics actually soundly reinforcing it. Whatever trauma, neglect, discrimination, extreme distress we experience within our own lives, if not adequately dealt with and resolved, are likely to change us at a very core level (including cellular level) and then be passed down to our offspring (if not by the actual transmission of certain behaviour patterns and “core beliefs” about self and the world directly, than probably epigenetically to some extent). Btw, I think that quite a good book on these ideas written for the layperson is Bruce Lipton’s, “The Biology of Belief.”
Paris Williams
Report comment
Hi Paris and thanks so much for your comment. I agree that epigenetics puts environment and environmental insults front and center as the cause of mental distress or suffering. (I am familiar with Bruce Lipton’s work and attended a fascinating lecture by him earlier this year.) And, yes, epigenetics will most likely rehabilitate Lamarck and his work. But epigenetics also validates certain aspect of the biological perspective as well, showing that the environment does change one’s biology and those changes are passed on. Epigenetics shows that altered gene expression is transmitted to future generations, and not just through the modeling and repetition of dysfunctional parenting (which, I am sure, does happen), but genetically as well. So, the original sin, or the trauma that originated from the environment, people, life, etc. becomes embedded in one’s physical body and in each subsequent generation, the person with altered gene expression becomes more vulnerable to new environmental insults, bullying, rejection, exclusion, social defeat, etc., leading to further degradation of gene function until, several generations down the road, someone breaks down. Does it follow that the parents did it, or probably did it? I do not believe this is what you intended to say. I actually liked your article very much and I am totally against making parenting issues a taboo subject. I am just arguing for balance and for being open to the whole truth.
Report comment
Hi J,
To me what Open Dialogue proves is that it’s not an ‘illness’. I think that family or no family problems can be sorted out.
What turns a person into an expensive psychiatric patient is the medication. I would definitely accuse the medication.
Prior to medication most longterm hospitalization would probably have been due to discrimination and neglect – Ireland would have been a good example of this.
Report comment
“Prior to medication most longterm hospitalization would probably have been due to discrimination and neglect.”
Hi Fiachra:
Discrimination and neglect are certainly bad and unhelpful to anyone’s well being, but are these in and of themselves sufficient to cause serious mental illness? Common sense, to say nothing of science (epigenetics), answers this question in the negative. How is it that the the Holocaust survivors, who witnessed, endured and suffered the unimaginable did not as a group become psychotic or serious mentally ill? Actually, as a group, they were a pretty resilient bunch. Often migrating half across the world and starting news lives, they led functional and productive lives, personally and professionally. By the same token, this population does have a higher rate of suicide and their descendants have higher rates of mental illness. That’s epigenetics at work. Environmental factors (e.g., trauma, abuse, starvation, etc. etc) do change one’s biology and those changes are passed on to future generations, making each succeeding generation progressively more vulnerable to new environmental stresses, until, down the road, someone does break down. Does that follow that the family caused it? Does that warrant playing the blame game?
Report comment
I don’t see how we can compare people, cultures, and generations, as far as how people respond to various degrees of life’s hardships. That would seem rife with projection and conjecture. We don’t know another until we walk around in their skin.
And when comparing in terms of who becomes or does not become ‘mentally ill,’ is vague at best. No one can even agree about what mi is or is not. This is all so subjective and in the eye of the beholder.
However, when we discern by when we feel inner peace vs. when we feel internal chaos, then there is a bit more clarity about what this means.
Discrimination and neglect, indeed, can cause serious mental chaos and emotional upheaval, especially if it is a repeated pattern since childhood. That tends to pile up and become rather dramatic in our minds as it snowballs, until we shift our perspective to present time and address the post traumatic stress head on.
I imagine Holocaust survivors experienced extreme post traumatic stress that manifested in a variety of ways. A lot of successful people can be suffering from many things, and keep defenses high out of survival. I think it’s remarkable what humans are capable of doing and overcoming, when the chips are down.
Different people, different generations, different cultures, different social influences, different individual personalities, perspectives and beliefs, all influence our internal experience. I believe the goal is to alleviate suffering by increasing understanding and awareness of others, without judgment–including of self. That is what will move us forward as a humanity, to my mind.
Report comment
“I think it’s remarkable what humans are capable of doing and overcoming, when the chips are down. ”
Quite so. On the other hand, people do break down without having been abused or neglected. The difference is that some people are more resilient and others are more fragile. The issue of predisposition is missing from the discussion,
Report comment
While I’m not convinced these are ‘fixed,’ but rather along a very flexible continuum, I do agree that the discussion of ‘predisposition’ would be most relevant. There are so many factors that define our individuality at birth, and this continues on in life. Fragility can be strengthened and resilience can be tested. That pole can shift at any time.
Resilient vs. fragile is a dualistic perspective which can so easily tilt into judgment and evaluation, that can in turn, tip into stigma. I feel this more than likely an illusion.
“Sensitivity” means ‘easily picks up energy,’ which is not necessarily a bad thing, and in fact, can be a gift and extremely valuable and powerful tool in life, yet we tend to project it as being a weakness that doesn’t allow a person to ‘measure up.’ This is where I get stuck in the discussion because I don’t at all accept that.
In my practice, I help people to navigate their sensitivity to their advantage. It’s pure inner guidance. Clarity.
Report comment
Hi GetitRight,
What I’m saying here is that (prior to medication) most of the longterm ‘locked up’ people were more neglected than ‘mentally ill’.
I think research bears this out :- Look at the beginnings of Open Dialogue in Finland, and Dr Peter Breggins initial experience with longterm hospitalised people in hospitals in America. In both cases when they went into the back wards, they found people could be brought back to life with healthy social contact.
They could be described as victims of discrimination because nobody acknowledged them, and they were certainly institutionalized (as anyone would be in their situation).
Report comment
Hi again, Fiachra:
Stress, trauma, suffering, abuse are, regrettably, all too common and take their toll. Some people succumb, others endure unspeakable horrors and do not break down. Why? Obviously, there is more to it than one’s own life experience. It is an issue of predisposition (greater resilience vs. greater sensitivity), and the emerging science of epigenetics bears this out.
Report comment
Hi GetItRight,
I believe the medication is the culprit.
I’m not saying that the longterm hospitalized people didn’t have had an initial ‘crisis’ – I’m saying that without medication the crisis would have resolved itself (most of the time).
Take myself, when I tried to come off medication I ended up in hospital very quickly, because I couldn’t survive without medication (even though I had refused medication Initially).
But I was eventually able to (carefully) stop the medication and become independent of the system.
If I had had suitable help at the start (as I asked for) the disability and expense would have been avoided.
I’ve been hit with many life problems since but I’ve survived (as a result of the non drug help I received).
Report comment
Hi Fiachra,
I could not post a reply to your last comment, so I am responding to my own last comment and hope that you will see this. I have no doubt that medication is the culprit in a great many instances; that’s the conclusion of Robert Whitaker’s work, and I buy it. But does it follow that it is always true, in each and every case? I do not believe so. Mental illness (real mental illness, not just life problems that we all have) existed long before meds made their appearance. I do like your inspiring story very much but I do not think you can generalize from your own experience and conclude that it will be true of everyone else. Why do you think the majority of psychoanalysts (at least here, in the U.S.) rely on meds?
Report comment
Great article! Thank you very much! I wish more people had the courage to talk about this topic. We could save a lot of pain and suffering for a lot of people. As a researcher and a mother of a person diagnosed with “schizophrenia” I am in 100% agreement with you. I have shared my research and personal perspective on the topic in my book, A Theological Interpretation of Mental Illness. We have also started a program in our church to help the families of those suffering from madness. We are in early stages, but we are seeing confirmation of the research that you have noted in almost every case. It is amazing what a difference it makes when the families are enlightened about the root of the problem!
Look forward to reading your follow up segments.
Report comment
Hi Elahe,
I’m glad to hear you resonate with the article. And it’s always heartening to hear from others such as yourself who are willing to do the hard work of looking honestly at what are sometimes uncomfortable truths, and supporting troubled families in doing the same.
Best wishes,
Paris
Report comment
Thank you for this wonderful explanation of how to create toxic double bind relationships, which so closely describes what happened to me. My child was sexually assaulted, outside our little home, but this resulted in a cover up of the abuse, by my larger former religious family, my ex-religion. This is how the ELCA religion, and possibly all the paternalistic mainstream religions of today, at least that’s what I was told, have historically covered up their “zipper troubles.”
“[T]he authority figures within a [religion] [the pastors, bishops and doctors] place the [person] in a double-bind by setting up conflicting injunctions so that it is impossible for the [person] to satisfy [them] without violating [God], then a situation can result in which the [person] experiences such overwhelming distress that they are forced into a kind of psychotic reaction as a kind of extreme strategy to tolerate this otherwise intolerable situation.
“… R.D. Laing suggested that these kinds of interpersonal and intrapersonal binds that develop within dysfunctional [religions] go on to create an incompatible knot, or untenable dilemma within the [person] that forces her to essentially ‘go mad,’ which he saw as a profound transformation of the self resulting from a desperate attempt to resolve this otherwise irresolvable dilemma.”
Although, when gas lighting parishioners to cover up child abuse, the ELCA pastors, bishops, and their “Christian” therapist and doctor friends go all the way, including “the staging of bizarre events by the abusers with the intention of disorienting the victim.” They delude psychiatrists, with a bunch of lies, so the psychiatrist will disorient the victim and create psychosis, via the central symptoms of poly pharmacy induced anticholinergic toxidrome, 14 distinctly different ways, according to my medical records. Today’s “gold standard” treatment recommendations for “bipolar” are known to cause “psychosis” via anticholinergic toxidrome, so they should be changed.
And when one does discover that these child abuse covering up tactics are condoned by all the bishops of the ELCA religion, one does leave that Satanic religion. Thankfully, lots of pastors have now left this insane religion also, biggest mass exodus from any religion in history. And disgusted former pastors of the ELCA are now also writing books about this appalling pedophilia covering up problem within today’s ELCA Chicago synod headquarters. I’m apparently merely only one of the many widows disgusted by “the religious authorities who devour the widow’s purse while hell bent on making sure the church suffers such agonizing theological carnage that it is no longer recognizable.” From this book, the chapter on evil is a good one, too:
https://books.google.com/books?id=xI01AlxH1uAC&printsec=frontcover#v=onepage&q&f=false
And I will mention that the anticholinergic toxidrome induced psychosis is an absolutely disgusting type of psychosis, one in which the person gets the voices of the child molesters pumped into her head, bragging incessantly about their sexual abuse of children. I understand this is very common.
But, once one escapes these appalling psychiatric / religious gas lighters, and starts to heal. She will suffer from a drug withdrawal induced super sensitivity manic psychosis, which the psychiatrists really do have a moral obligation to forewarn patients and their families of, but they do not. This can be a healing psychosis, however, as mine was, albeit bizarre. It introduced me to the theory that there may exist a web of connectivity between all people, what Jung calls the “collective unconscious.” And via a midlife crisis type remembrance of all the wonderful people I’d known in my life, who were smart enough to comprehend that it is not a-okay for any human, of any profession, to profit off of covering child abuse by turing concerned mommies or children into “psychotics” with drugs. These wonderful “souls” reminded me, via a manic, but staggeringly serendipitous lyrical libretto love story that I was not, in fact, “irrelevant to reality,” as my disrespectful boob of a psychiatrist had claimed. I went through some sort of weird seemingly Hermeticism inspired ceremony, where I supposedly obtained eternal life, and all the souls who’d died before were supposedly released from the seventh heaven or some such thing. It was bizarre. I supposedly became ‘of the bride’ of Jesus. It was a spiritual born again story of sorts. Then Jesus supposedly claimed it was time for the eternal judgement. And, according to my ongoing semi lucid dreams, God is in the process of dividing the decent from those who will not be written in the book of life at this point in time. Which I have a gut instinct is all those unrepentant hypocrites still profiteering off this “dirty little secret of the two original educated professions.”
My ex-religion believes “repentance is a ‘work,’ thus irrelevant and unnecessary” since they believe salvation will be based upon “faith alone.” But they’ve put their “faith” in psychiatrists, rather than God, which strikes me as stupid. If anyone knows of any ELCA ministers who do not believe it’s okay for pastors, bishops, and doctors to cover up child abuse in this manner, I’d love to find one. Been looking, haven’t found one yet. They just get embarrassed and run away, because they run child drugging organizations in your neighborhood and want to continue profiting off of turning abused children into mental patients for profit, or they deny, deny, deny.
I understand 2/3’s of all so called “schizophrenics” today are actually child abuse victims. And the neuroleptic drugs do indeed create both the negative and positive symptoms of “schizophrenia” all by themselves. The negative symptoms of “schizophrenia” are created via neuroleptic induced deficit disorder.
“Neuroleptic induced deficit syndrome is principally characterized by the same symptoms that constitute the negative symptoms of schizophrenia—emotional blunting, apathy, hypobulia, difficulty in thinking, difficulty or total inability in concentrating, attention deficits, and desocialization. This can easily lead to misdiagnosis and mistreatment. Instead of decreasing the antipsychotic, the doctor may increase their dose to try to ‘improve’ what he perceives to be negative symptoms of schizophrenia, rather than antipsychotic side effects.”
And increasing the neuroleptic dose can result in psychosis, and the other positive symptoms of “schizophrenia,” via the central symptoms of neuroleptic (or poly pharmacy) induced anticholinergic intoxication syndrome. Which also gets misdiagnosed by psychiatrists as “the classic symptoms of schizophrenia” “there must be someone in her family.” Yes, grandma was allergic to one of the old neuroleptics, too. But back then the psychiatrists were smarter, they just took people off a drug that made one sick, rather than trying 32 other toxic drugs on a patient, prior to finally figuring out I was allergic to all the psychiatric drugs.
What a sick, twisted lunacy fest today’s psychiatric industry is. I really hope they get out of the business of profiting off turning child abuse victims into “psychotics” with their drugs soon. To my knowledge, covering up child abuse is still a crime in the US, although apparently not for today’s corporate religions.
Report comment
Hi Someone Else,
I’m really sorry to hear about your going through such a difficult situation. I think you speak to some very important social network extending beyond the typical nuclear family (religious groups, mental health systems, etc.) who certainly have the power to do great harm, even to the point of pushing people “over the edge.” I lived for several years myself in a fundamental religious foster home as a child, with physical and sexual abuse occurring within it (fortunately, I wasn’t sexually abused, but was physically and emotionally abused), and there is no doubt that this played a role in my own breakdown/breakthrough madness process that occurred many years later. I count my blessings that I managed to avoid getting caught up within the psychiatric system.
Sending my best wishes,
Paris
Report comment
Thank you, Paris, and I am grateful it was me, rather than my child that got caught up in today’s mental health system’s profiteering off of child abuse cover ups. I was wise enough to escape, my small child would not have been.
Nor would I have been wise enough to likely prevent him from being captured into the “mental health system” that has taken over our public school system. Due to his 8th grade public school social worker’s desire to have him drugged, for surprising his public school system with his ability to heal from the common symptoms of child abuse, one of which is, of course, trouble in school after the abuse. Which was occurring at his entrance into the public school system. But it is a shame the public school systems of our country today actively cover up child abuse concerns, when informed of them.
My child did largely, hopefully, recover. He went from remedial reading in first grade, to getting 100% on his state standardized tests by eighth grade, graduated as valedictorian of his private prep school high school class, and is doing very well in college – all based upon my theology that love and mutual respect is the cure for evil life events, rather than psychiatry’s theory drugs cure such.
He’s studying psychology, a bit to my dismay, but since the “mental health professionals” are currently the “thought police” ruling our world, it’s likely not a bad major for him. And those who suffered extreme injustices in their youth, no doubt, are the ones who go into psychology and psychiatry, so they may try to understand their own problems.
But since this is the logical reality, it does make sense these insecure people, were so easily bought out by the stupidity fest of the psycho / pharmaceutical industry’s iatrogenic illness creation system. We’ll see where this undergrad leads my son, I think he’d rather teach, than practice psychology. And I think this would be wiser. But he is reasonably aware of the stupidity fest that is the current psychiatric industry’s iatrogenic illness creation system of today.
I do absolutely agree with much of what I’ve read of your theology, and would love some proper guidance for my little love, if you you have any suggestions. He is a brilliant and wonderful soul.
Report comment
Thanks both for this, Paris – as well as your book – very helpful. Glad someone is calling out the taboo topic.
Wish to emphasize the impact of ACE’s/trauma contribution to psychosis – particularly the developmental traumas that occurs at very young ages (0-3), pre-verbal, that undermine attachment and ability to self-soothe. I believe this really lays an often unrecognized foundation for later “psychotic” experiences .Also noting, that the since the diagnosis of psychosis has such little validity – that there are probably several different etiologies, manifestations – that currently all lumped together. It makes these conversations difficult, as we attempt to compare apples with watermelons.
Report comment
Hi Wayne,
I’m glad to hear you enjoyed the article. Yes, I don’t seem to mind “sticking my neck out there”–perhaps all those years doing wild things on hang gliders 😉 Great point about the very early developmental traumas. I’ll be going over exactly these points in greater detail in Parts Two or Three, so stay tuned…
Best wishes,
Paris
Report comment
It’s certainly fun to watch psychiatry re-invent the wheel, over and over again. And then forget what they re-invented and go back to cruelly persecuting people. Ad nauseum.
Report comment
I have walked the talk and don’t buy half of the overly researched bull spawned here. Take the clothes pin off the dogs tail so he can stop researching on how the pin got there.
Report comment
Thank you for your thoughtful, brave, and well-researched article.
Taking blame out of the equation is essential in order for families to heal. Some parents have great difficulty giving what they did not receive themselves, and unresolved trauma that becomes trans-generational is often at the root of young people entering into extreme states.
I have found Atwood, Stolorow and Orange’s essay Shattered Worlds/Psychotic States
A Post-Cartesian View of the Experience of Personal Annihilation
helpful in my efforts to understand “psychosis”.
http://www.georgeatwood.com/uploads/7/3/4/6/7346190/shattered_worlds_psychotic_states.pdf
Report comment
I agree,”unresolved trauma that becomes trans-generational is often at the root of young people entering into extreme states.”
I think this is also why the baby boomer generation in general have proven themselves to be such poor, and fiscally irresponsible, leaders. Their parents were traumatized by WWII, resulting in a bunch of “baby boomers,” people who never matured to the realization that life is not all about themselves, thus they’re called the “me generation,” too.
I know all the people who had me defamed, poisoned, and tortured were about 10 to 15 years older than me, and they behaved like a bunch of disrespectful and stupid children. When did it become acceptable for a deluded doctor to declare a patient’s life, “a credible fictional story,” after he has his delusions pointed out. How pathetically immature, not to mention unethical and plain stupid.
No doubt, “trauma that becomes trans-generational” is the root behind many of today’s problems. The baby boomer generation’s greed and immature philosophies have fiscally destroyed this nation, and they’re destroying the entire world with their moronic never ending wars now. War is not the answer, that’s a childish and self serving belief system. All of humanity needs to learn to grow up, coexist peacefully, with mutual respect, instead.
Report comment
Hi dcharles and “someone else,”
I appreciate your bringing in the importance of transgenerational trauma, and I appreciate your thoughts and personal sharing about this.
Many (most?) indigenous societies maintain strong connections with their ancestors, really acknowledging and honoring the deep connection of one’s current and societal experience with the experiences of one’s ancestors, and I think it’s a shame that, for the most part, we in contemporary society have lost this. Therefore, I think that this leads to a kind of intergenerational blindness we so often find as parents, we keep repeating the same problematic behaviours and inflicting the same kinds of wounds on our own children as those that we experienced as a child, and we as societies continue the cycle of war, oppression of trauma. The descendants of an oppressed people often go on to become perpetrators/oppressors themselves. But by letting go of the concept of blame (which essentially doesn’t acknowledge systems dynamics and the importance of things like shared responsibility and intergenerational trauma), I think we then have the capacity to look honestly and openly at our own behaviour and the behaviours and lessons of our ancestors, and make some real change.
A famous poem that I think speaks to this well is Thich Nath Hanh (this link has a compelling intro by the author): http://wtf.tw/ref/nhat_hanh.html
Best wishes,
Paris Williams
Report comment
Thanks for the comments and poem, I like that it ends with a prayer for compassion. I do pray we end the cycle of violence and unjust profiteering, and now know our current leaders and country are definately not the great leaders we were taught, and absolutely our country is a part of the problem, not behaving as part of the solution. We all need to repent, ask for compassion, and work towards coexisting with mutual respect instead. Thanks, Paris.
Report comment
What a timely article that you’ve authored since I too have been considering this very subject lately. I was diagnosed with an “unspecified psychotic disorder” three years ago and later with paranoid schizophrenia. The experience was absolutely devastating in all aspects of my life, and I puzzled over exactly why, suddenly at 33 years old, I would develop such a horrible disorder. It seemed unlikely to me that this could be a physiological mental disorder.
It wasn’t until I became acquainted with the work of Bertram Karon that I discovered that hallucinations and delusions have metaphorical content. When I reflected on this, I realized that my hallucinations and delusions were, without exception, expressions of certain KINDS of past trauma that originated in my family, particularly with respect to my mother’s treatment of me.
Both Fromm-Reichmann and Bateson were mostly correct, though the latter, I’ve recently learned, really wasn’t trying to explain the mechanism behind schizophrenia at all but rather the ecological relationships in the patterns of communication in the context of schizophrenia. Bateson was, after all, an anthropologist and not a psychiatrist.
The double bind practiced verbally isn’t quite the mechanism behind schizophrenia, but it’s definitely a psychologically dysfunctional adaptation that relates to it. Instead, a parent who practices the double bind verbally also practices other behaviors, both verbal and nonverbal, that ultimately prevent their children from achieving psychological needs like love and affection. This is ultimately the trauma of the double bind and other behaviors like it that it implies which predisposes one to schizophrenia, and this trauma occurs not just in childhood but also during infancy and onward since the parents, particularly the mother, were psychologically dysfunctional at that point as well.
This trauma is terrifying because, for the schizophrenic, it incited in the past fear of death. When we’re very young, we instinctively seek out love and affection from our parents, particularly our mother. If a mother is ultimately rejecting (though unwittingly), as according to Fromm-Reichmann and her theory of the schizophrenogenic mother, then this, for the child, implies no sense of safety from danger. And without that safety from danger, the child, from his perspective, is in danger of death.
To understand schizophrenia well, one has to understand Karon’s interpretation: schizophrenia is caused by terror brought about by that trauma. Schizophrenia is completely involuntary, and it shouldn’t be characterized as a means of escaping intolerable circumstances. What’s really happening is that perceptions that are equivalent in meaning, expressed metaphorically, to the original trauma and traumas related to it are intruding into the conscious mind to warn it of danger.
I’m writing an article about this myself which, while incomplete at the moment, should give some further insight into this and exactly how hallucinations and delusions develop. If anyone doubts that hallucinations and delusions are metaphorical expressions of past trauma, please read the accounts of some of my own hallucinations and delusions at the end of the article:
https://docs.google.com/document/d/1_law0rdNMm92CHvDy3hJjUAPAkzf1Yn1AWSKEAbhdc4/edit?usp=sharing
Report comment
Good comment. I’ve seen a few commenters urge caution because “we don’t know what causes psychosis” and “trauma doesn’t always cause psychosis”, etc. But I find these ideas to be mistaken and far too timid. It’s time to be more bold in stating that we know a lot about what causes psychotic states of mind.
Experienced therapists like Bert Karon, Vamik Volkan, Murray Jackson, who work with psychotic people for years and understand their histories, virtually always find experiences of serious abuse and neglect between people who become psychotic and some aspects of their early environment (usually, not always, coming from the parents). The key thing is that the person who will later become psychotic is vulnerable enough at the time they experience these traumas, or becomes vulnerable enough after enough stress, that they experience these interactions with the environment as terrifying, horrifying, and self-shattering. Strong negative emotions are always involved in psychotic disturbances, and emotions are, in the first instance, a reaction to the surrounding environment; later to internalizations of that environment.
So, it’s important to see that the person who becomes psychotic experiences some series of interactions with the environment as traumatic, terrifying, or horrifying. It doesn’t just happen out of nothing. These overwhelming all-bad emotions then lead to the attempt to escape the intolerable emotional state via primitive defenses including denial, splitting (self-fragmentation, i.e. non-autonomous alters), fusion (confusion of self and other), and hallucinations/delusions (i.e. externalization of intolerable experience).
Through case studies of psychotherapy – and we will never glean a full understanding of this from quantitative research – there are many accounts of this type of trauma/abuse/neglect causing psychosis. Some I can remember off the top of my head would include Ping-Nie Pao (Chesnut Lodge therapist) and his writing about how organismic terror causes a regression of the personality to a schizophrenic state; Vamik Volkan’s (University of Virginia psychoanalyst) writing about how a childlike delusional self forms to ward off feelings of horror and terror in poeple who undergo trauma, Murray Jackson (British psychotherapist) and his many case studies of psychotic young people in which he explored their early family relationships, James Grotstein (American psychoanalyst) writing about the black hole states and defenses against black hole states (meaning how psychotic people cling to fantasized all-bad inner relationships so as not to fall into a horrifying nothingness or void), Harold Searles (Chestnut Lodge analyst) accounts of dedifferentiation and identity confusion between the schizophrenic person and their significant others in early life, Donald Rinsley’s (Menninger Institute psychiatrists) studies of the horribly negative relationships between psychotic young people and their families, and Silvano Arieti’s (New York psychoanalyst) study of early traumatic family relationships of young people who became psychotic. I think Harold Searles’ writing about how the psychotic-to-be young person and their parent-figure commonly have intense ambivalence about engaging in a secure close loving relationship (for whatever reason) is particularly powerful.
A careful review of these authors’ books doesn’t support the notion that we don’t know what causes psychosis. Psychiatrists who say that old psychoanalytic notions of trauma or abuse causing psychosis have been debunked are full of shit. These ideas have never been debunked, and after being prematurely buried they are now being resurrected in the ACE study and all the other studies Paris cited. Experienced therapists of psychotic people have known and written for some time about the causes of psychosis, which are essentially deficits of positive relationships or resources (neglect, poverty), and active negative relationships and environmental experience (abuse, trauma).
Let us not be too cautious, but instead assert that from the ACE study, John Read’s research, and the many other sources cited in Paris’ essay, that we have a good idea about what causes psychosis, and thus can be enabled to make progress in addressing and understanding these causes and helping people who’ve undergone these terrible experiences to repair the damage.
Report comment
In my opinion, there are several difficulties in overcoming the medical model of schizophrenia and psychotic disorders. First, antipsychotic medication is effective in arresting psychosis which gives the impression that psychotic disorders are analogous to genuinely physiological diseases like diabetes treated with insulin is effective in controlling its symptoms. Of course that’s only because it literally tranquilizes the mind of the psychotic patient rather than correcting some deficiency in the brain.
Second, parents of schizophrenics are likely to resist (again) explanations that inculpate their parenting in their children’s developing schizophrenia. NAMI itself was, of course, founded by two mothers of schizophrenics, Harriet Shelter and Beverly Young. The irony and tragedy in their efforts to overcome psychological explanations for schizophrenia in favor of physiological explanations is that it prevented genuinely effective treatment from being delivered to their own children and to future schizophrenics through psychotherapy.
Third and possibly most importantly, schizophrenics, like all who have been reared in dysfunctional families, usually do not have insight into the dysfunction of their families.
However, the Achilles’ heel in psychiatry is that the symptoms of psychosis in psychotic disorders are metaphorical expressions of past trauma. Most anyone would admit that this precludes the possibility that psychotic disorders are physiological and that their symptoms are random errors in perception. This should be the point that’s emphasized in reaching the truth of schizophrenia and other psychotic disorders along with the success in treating patients that’s been achieved by psychotherapists who understand them.
Report comment
t4nk:
You write: “schizophrenics, like all who have been reared in dysfunctional families, usually do not have insight into the dysfunction of their families”
My daughter is one of the exceptions to your rule. She has been diagnosed as ‘schizophrenic’ yet she seems to have more insight about our family than anyone else in our family. I value her counsel greatly because her insight is a lot more spot on than counselors who have years and years of university training.
At times my daughter seems clairvoyant; at other times, she has the uncanny ability to expose hidden truths. She can apply logic to the most tangled up situations, liven up a conversation with a fruitful train of thought or poetical comment, and inspire very productive self reflection. Obviously, she is very equipped to light on our family dysfunctions.
For whatever reason, she is generally unwilling or unable to couch her insight in a gentle or diplomatic fashion. This is a problem I would categorize under ‘social graces.’
Her episodic departure from consensual reality, has left her with a legacy of ‘bluntness’ which I hope is not permanent. Her delivery as well as her timing can only lead to ‘relational suicide’ as very few friends and family members can withstand years of unsolicited advice, when it is delivered in caustic and barbed tones or dripping with contempt. And quite often, whether due to dissociation or past trauma, she directs the right message at the wrong person or the wrong message at the right person.
So, she has the insight but not the means to deliver the insight in such a way as to be an effective agent of change or as Carnegie would say, ‘win friends and influence people’
Report comment
t4nk, thanks for your thoughts. You identify some factors that do make it difficult for (some) people to admit that trauma and poor parenting contribute to psychotic breakdown.
Stepping back, I have another perspective. America constitutes 4% of global population, and other countries do not revolve around America, no matter how much some Americans seem to feel America is the most important country in the world. In fact, America is gradually weakening in power and influence relative to other large nations. This is evident in the decline of our middle class economically and the responses we see to it in this year’s electoral process.
So NAMI is one group in a nation with 4% of global population. It would be interesting to know how family groups/political dynamics around psychosis work in countries like Brazil, Russia, China, India, Nigeria, Indonesia. Those are countries containing close to 50% of global population, i.e. over 3 billion people. Their voices should not be quieter than the voices of a few million mostly ignorant American parents. And I feel pretty confident that most parents in these nations, where antipsychotic drug use is less frequent and drug companies don’t market directly to the public, are not so tied to a biological genetic model of psychosis.
For me, believing that schizophrenia is a brain disease is another in a series of delusions that many Americans seem to hold… for example, that climate change is not real, that evolution is a myth, that invading Afghanistan and Iraq without valid pretext is just business as usual.
For some reason Americans seem to have great difficulty looking at real evidence and data, instead just willfully and delusionally believing whatever they want. I guess many people are this way, but for some reason it seems particularly bad in our country. The world does notice, if you read foreign newspapers, that American politicians (especially Republicans, it has to be said) are particularly ignorant and delusional relative to other countries’ when it comes to things like climate change and evolution.
Now this is starting to sound like an anti-American polemic. But America does hold much responsibility for spreading the most destructive and pessimistic approach to human problems ever devised, the brain disease model (and now, even propagating it into other countries with no respect for their views). And NAMI parents and people like Tim Murphy who spread this misinformation should be called out for their ignorance and for spreading evidence-less myths. Americans should admit that there is no known brain disease called schizophrenia, that drugs have not been proven to be an effective long-term treatment for said illusory condition, and that psychosocial approaches to psychosis show much more promise.
I agree with Madmom that it is mistaken to say that psychotic people don’t have insight into the dysfunction in their families. Psychotic people are not psychotic all the time and, during more lucid periods, traumatized people can be very insightful observers of the dynamics of their relationships. However, for those who take antipsychotic drugs (which again in the US is far too many) this may be less the case, since the drugs reduce the ability to think clearly and reflect/observe.
Report comment
I experienced psychosis recently. Poverty from Table 1 explains my childhood, as does emotional neglect. It was just my mom raising 4 kids… I feel that my family is dysfunctional. I don’t have a major trauma, but I’m 27 still living with my mother in poverty, so maybe that works on my brain chemicals negatively. I say emotional neglect because I’m a loner with no social group outside of my house, and that started in childhood. Because she was the only parent I really never was allowed much socialization with friends. I don’t have many. Even now the only time I get out to socialize is when I go to work. I’d be interested to see if there is correlation between size of friend group and risk of developing psychosis as well. I wonder if there are changes in the brain that arise because of social activity, or lack thereof. (Including family.)
Report comment
Hi M.W.,
Thanks for sharing a little about your story. It sounds like life has been quite a challenging journey for you! That’s unfortunate that your were hindered in developing satisfying social connections. As social beings, there is no doubt that healthy connection is extremely important to our wellbeing (I’ll talk about this much more in the next 2 parts); and so I think there’s no doubt that if our basic social/connection/belonging needs aren’t met, we’ll experience a lot of distress, and I think that everyone has a threshhold of tolerance, in which our psyche (our organismic wisdom, much of which we are not directly conscious of) may resort to the kind of desperate haphazard coping/growth-oriented strategy often called “psychosis.” While of course all mental experiences have biological correlates and vice versa (so surely extreme emotional or mental states correlate with “unusual” activity with the brain and body), I think it’s important that we remain very skeptical when we hear the preaching that such extreme states of mind/body automatically a pathophysiological disease. So yes it does appear that there are certain anomalous states of mind and body/brain associated prolonged trauma, but rather than seeing this as disease, we can see it as our organism adapating to difficult circumstances in the best way that it can; and that if are able to change those circumstances and/or our relationship to them in a way that more conducive to wellbeing, then there’s every chance that our physiological and mental states will both improve accordingly. The “lifelong disease” hypothesis promotes hopelessness, disempowerment, and thus a self fulfilling prophecy; the “natural adaptation” hypothesis promotes hope, empowerment, and possibility. Which of these do we want to feed?
Best wishes,
Paris Williams
Report comment
As usual, Paris’s articles are meaty, absorbing and very well researched. And he’s hit on a very raw nerve here. In Ireland, Tony Humphreys wrote an article two years ago in The Irish Examiner in which he suggested that family might just have a teeny weeny bit to do with subsequent child development. A veritable witch-hunt ensued with the media rowing in shamefully, in a disgracefully populist way. I do hope he reads your piece. You cannot squeeze everyone in, but I do think that Virginia Satir deserves a star mention – not just because I did a great sculpting workshop with her, and she trained my sister! And I do think that the imposition of psychotropic drugs on children has to rank not only as an ACE, but as one of the great crimes against children: every time I look at a photo of little Rebecca Riley, and think of her case, my entire being revolts in anguish and disgust.
Report comment
It’s a fantastic article – I’m wating for the next instalment.
You can’t beat an Irish family for skrewing up the head anyway – this goes back to the famine.
But it’s possible to get better with the right kind of basic and inexpensive help. I blame the neuroleptics and the longterm ‘illness mentality’ (and diagnoses).
Report comment
Hi Redmond,
I’m glad you’re enjoying the article. Thanks for sharing these valuable comments.
You say: “I do think that the imposition of psychotropic drugs on children has to rank not only as an ACE, but as one of the great crimes against children: every time I look at a photo of little Rebecca Riley, and think of her case, my entire being revolts in anguish and disgust.” I am in full agreement with you about this. It’s hard to imaging anything more assaultive to one’s mind, body and spirit that forcing mind-altering drugs into you against your will, and even if a child assents to such an act, I don’t think they can truly give “informed consent,” given their natural lack of life wisdom and power in their world (not to mention the ethics of experimenting so haphazardly with a developing organism).
I didn’t formally include any drugs (recreational or psychiatric) as a a formal ACE on the list, though it’s clear to me that they are correlated with the onset of psychoses and extreme states of mind, as generally speaking, one or more of the other factors occurs first, and the drugging is often secondary to this. However, I realize that with the way things are going, with parents being so radically misinformed and drugs increasingly being handed to kids as freely as if they’re lollies, I’m sure there are many cases now in which the drug use itself is best seen as the primary trauma or ACE.
Best regards,
Paris Williams
Report comment
This is an excellent article that does much to highlight the role of the familial environment as a factor in psychosis. Too often family involvement has been ignored when it comes to how to help someone through psychosis, although it has often been accused of being the contributor to psychosis. In my far too many years of involvement with the recovery movement, I’ve had a lot of trouble trying to figure out if the recovery movement views psychosis as a good thing or a bad thing. It has a foot in both camps. In a quasi-medicalized version of psychosis, it’s always a bad thing, caused by trauma (bad). The individual is therefore seen as a damaged being, along the lines of a war veteran undergoing rehab. You know that he was hit by a shell, you know when it happened, etc. and you try to repair the damage. In the non-medicalized version of psychosis, which some say is the ‘romanticized version, the person has special gifts, experiences an existential/spiritual crisis. He or she is not damaged. He/she is on a mission. No one should be blamed for the spiritual path that the person is on. The idea is to encourage that spiritual path, not to fix it. I’m struggling to express what I mean here. To be somewhat humorous, was Jesus Christ a trauma victim or carrying out a spiritual mission?
Our family has done its time with Family Constellation Therapy, which was an insightful look into the family dynamics of previous generations that shapes our presence. I don’t at all regret doing it, and it was very helpful for all concerned, but it was not the whole picture. It only offered one possible explanation for why my son went psychotic. Numerology has been helpful, too. No trauma there, just the way his numbers added up hinted at who he IS. Homeopathy offered its own explanation (a most insightful one) for his personality and the remedy given pointed to the possible cause of his breakdown (who he IS). No trauma involved there, either. I guess all of this to say is that the family environment may offer some clues as to what happened to the person AFTER birth, and it’s easy for our fact oriented Western minds to grasp these connections, but it’s only one factor amongst many.
Report comment
But don’t you think that, regardless of what causes the ‘psychosis’ (which I view as an initiation that is intended to awaken a person to their spirit and spiritual path, and after that, integration and grounding, then they’re on their way), if the family, itself, were to take a neutral-positive view of things, that would be the most helpful and supportive thing for the kid, and would help them greatly to integrate all of this in a productive way?
Whereas when the family is demeaning and stigmatizing, just as we know the system is, then the chance for integration is pretty nil, unless the kid wakes up and takes the path of Siddahartha, leaving family and all else behind, in search of meaning.
What I want to get across–and this is from my experience, and also from what makes logical and reasonable sense to me–is that whether a family causes psychosis or not, either way, the family can be INSTRUMENTAL in the healing, if they were to choose to seek healing and integration, too, we all grow and when our children experience something like psychosis or anything that presents itself as dramatic and potentially threatening to their well-being, that’s a perfect opportunity for personal growth for everyone concerned. Whether or not it’s a ‘family illness,’ it can still be a family healing, and I think that’s a more productive focus. I think the question of root causes emerge naturally, when everyone is on their rightful healing path, and then it’s not so resisted, if it’s a challenging discovery of truth, it just is and from that awareness, we move on a different and more enlightened way. That is spiritual growth.
Families can heal together, or they can be divisive about the whole thing. I believe those are two ways of responding, and it makes a difference in how well the child can heal, and clarity is achieved all around.
Report comment
Btw, the update of my story of healing is not about my family of origin but about my relationship with my partner of 30 years now. By the time I did the family healing work, I was an adult, living with my partner, so a lot of that was long distance, and also through the voice of my film, that was central to it.
But my partner was my family during my time of disability from the psych drugs withdrawal, and still is. We’ve had dialogue after dialogue about this over the years, to get straight on exactly what happened, it all became such a mess so quickly, and I knew it wasn’t just because I was ill and disabled. People around me were literally driving me to the edge with their suddenly overpowering, insensitive, and controlling behavior–which is what I discovered from the inside, is what happens toward people who are obviously having some kind of challenges, even when they aren’t doing any harm to anyone.
But apparently, we confuse people, or perhaps make them strain to actually pay attention to what we are trying to communicate, and they resent that; and perhaps we frighten them from the unfamiliarity of it, or worse yet, the stigma of it, and that’s enough to make people be harshly impatient and downright mean to people as they are trying to recover, being blatantly and utterly disregarding.
I wish I had had a video cam attached to my forehead during this time, I’m sure people would be shocked at themselves with how their attitude and demeanor changes to utter lack of regard and respect when it comes to someone who is hard to understand to the point we call them ‘psychotic,’ especially if they are marginalized. That would be a mirror of truth that would horrify.
Respect these days seems to come with the expectation of something, not for the sheer social grace of it. I think that’s way too bad, makes a difference in our society, to all of us, collectively.
Point being, my partner had to find his healing path for me to continue on mine to fruition. He became kind of a monster at the time (let’s say his shadow emerged and he had to deal with it) which he readily admits. He was scared to death and the doctors and therapists had us both extremely confused and despondent. Being alone with this in San Francisco, one of the homeless capitals of the world, was, indeed, scary as all get out. We were wracked with worry, uncertainty, and desperation. And this was just after I finished grad school, so it was the last thing we expected.
As you know, Rossa, I eventually turned to energy healing and chakra work, and my partner followed in my footsteps when he saw the result this was having on me. It was night and day. I’m the healer in the family, now. Textbook transformation, and it just unfolded that way, the most obvious path to wellness. We really had no other choice if we were to survive this and get on with our lives without this albatross of ‘mental illness’ around our necks.
We both had to take full responsibility, and in so many ways, he was suffering from his own ‘mental illness.’ Again, he’s be the first to own that, that’s our story. His healing has been as spectacular as mine, his changes have been remarkable.
In our case, we discovered that it wasn’t about one person to scapegoat, it was the relationship system which is off kilter–as there were power, control and fear/panic issues there. Same with my family, exactly. So much filtering of reality through personal issues, it was just so dense, and I could see right through it, being the visionary that I am. But that didn’t help me until I learned a lot more about communication and energy.
I spoke my truth, my mother resisted and felt guilty at the same time, to be expected. We discussed it as best we could, let some time go by, she learned all about forgiveness, self-forgiveness, self-compassion, and is now, at 83, quite healthy, totally independent as she’s always been, and with a new boyfriend after my dad passed away 7 years ago, having the time of her life, which she well deserves. Between an emotionally abusive husband (who later in life had a debilitating stroke, and she had to take over and care for him) and a mentally ill son, my mom carried quite the load for a while, got through it, learned, grew, and rose above it all. I couldn’t be happier.
But it wasn’t easy for her, and she didn’t make it easy for me, either. Ok, so we have a feisty relationship. I still love her and we talk about once a month. I admire my mother very much for how she faced life like the tough cookie she is. We come from strong stock I guess–Russian-Jewish-Argentian, we’re not kept down easily!
My partner is also happier and more grounded and at peace than he’s ever been. We’ve all grown and found our peace. And they all took the cue in my healing from what I was calling “severe mental illness,” sure is how it felt to me. That part was caused by the drugs and the subsequent withdrawal, from nine of them.
But the issues of my extreme anxiety and deep depressions most definitely started in the family, because my mother was angry most of the time, and quite judgmental, and rather ruthless about it. It was still the whole family group dynamic in its totally, though, which was the problem. Everyone enabled my dad’s rage because of fear and dependence, so when I spoke my truth, they all came down on me. That started when I was five, and I never gave up on standing up for myself, and I always paid for it, until I finally took myself to a shrink, which is where all that began.
I thought it was me, and the whole time, it was them. I realized this 20 years later, and took steps to resolve this internally, and shift my beliefs about virtually everything. That dynamic really did a number on my consciousness, and waking up to it was tough, but necessary for healing.
My partner had his own issues which he had to face, that he’d been totally projecting onto me in ways that became oppressive and abusive. We were both repeating family dynamics, we finally got this and came into present time, transforming all of that energy into all we have now, which is abundant, on a spiritual level.
So along with me, they’ve both transformed and found peace and happiness. My healing was their cue. I’m so grateful for their courage and authenticity, and their heartfelt desire to see me well. Humbles me to no end. I learned a lot from this, more than I could ever learn in any kind of school.
Report comment
Hi Rossa and Alex,
I appreciate your comments and responses.
To add a little here, I would emphasize the importance of shifing out of “either/or” “black/white” “good/bad”, etc., dichotomous thinking and instead consider what we’re calling “psyhosis” from a “both/and” perspective.
So the extreme organismic response we’re calling “psychosis” here can be seen as both a response to overwhelming circumstances and also a potential opening into the awareness of core existential/spiritual truths and universal human dilemmas that most of us are generally not particularly conscious of. The experience of deep existential overwhelm can trigger a desperate survival response that allows both a glimpse into the more raw fabric of existence while also opening the door to the possibility of great chaos as the persons’s psyche attempts to integrate the various domains of experience (existential/spiritual, personal/egoic, environmental, etc.).
It’s also important to recognize that the conept of “overwhelming circumstances” is entirely subjective. We’re each endowed with unique blends of various sensitivities and resiliences, and the kind of experience that may act as a kind of “psychosis catalyst” for one person may be easily shaken off by someone else. Sometimes it’s very clear what the catalyst was, and other times it’s not very clear at all, and may involve a kind of “perfect storm” of multiple catalysts working together synergistically.
Finally, I’ll add that even if a particular family system is generally quite harmonious, loving, “healthy,” etc., we are all currently embedded in profoundly dysfunctional broader social systems (imho). Many of us have been so desensitized to this broader dysfunction that we don’t even see it, or maybe see it as a problem “in other regions but my community’s pretty good.” However, some of us, for whatever reason, are much more sensitive to this, and all too clearly experience ourselves as being part of a species painfully out of control and hurtling itself towards a cliff at an accelerating pace, whether or not this awareness manifests consciously or on some other level; and deeply feel the confusion, futility, chaos, hopelessness, etc., that goes along with such awareness. So regardless of the health of a particular family, the dysfunction of these broader social systems is enough to catalyze a “psychotic” response (I’d say that in my case, both problematic family dynames and an all too keen awareness of the broader social dysfunction “pushed me over the edge”).
In John Weir Perry’s, “Trials of a Visionary Mind,” I think he makes a compelling case that in virtually all societies, particularly sensitive individuals are especially prone to going into such psychotic processes when the broader community/society is in trouble, so they act as a kind of canary in the coal mine, whose particular experiences, chaotic as they may be, may convey important information to that particular society, highlighting the most problematic areas that need to be addressed to regain/maintain the health of the broader social system. This is not a romanticization, as the individual’s often experience great suffering indefinitely, but simply a recognize of the potential benefits of this process, moving through this person as a kind of channel, opening up the possibility of profound transformation, both within the individual and within the broader social systems (family, community, society, species…)
Thanks for your willingness to explore these challenging issues,
Paris Williams
Report comment
Paris, thank YOU for the opportunity to get further clarity here about cultural dynamics vs. individual process. Of course this is going to start in the family, our first culture. Such subtle yet powerful information, which, personally, I feel is the key to evolving out of stuck situations and perpetual inner conflict.
I think we all have our cultures and preferences which, when we follow our truth, can unfold in a way that we feel copacetic with ourselves, our environment and our community. I believe it’s that synchronicity which we seek, to feel part of and valued by a culture, rather than driven to the margins via stigma.
I think It’s really a matter of knowing ourselves, and having the courage to pursue happiness and inner peace over anything else. Again, as always, that’s a matter of choice, discernment, and personal preference.
Best wishes on your important research!
Report comment
Thank you for your willingness to explore the challenges we all face to some extent or another. Being human is a difficult journey.
Report comment
Alex,
And yes, I couldn’t agree more. The canary in a coal mine is a good analogy for the effect of societal dysfunction.
Cheers,
Rossa
Report comment
Yes, I absolutely agree that “if the family, itself, were to take a neutral-positive view of things, that would be the most helpful and supportive thing for the kid, and would help them greatly to integrate all of this in a productive way? Whereas when the family is demeaning and stigmatizing, just as we know the system is, then the chance for integration is pretty nil, unless the kid wakes up and takes the path of Siddahartha, leaving family and all else behind, in search of meaning.”
Here’s a bit of a twist on that. Many people, from what I read, appear to believe that the families were demeaning and stigmatizing from the get-go, and that’s WHY the person had a break. Consider, though, that it is very easy for families to become that way AFTER the person has had a break. It’s damn hard to live with someone in an altered state. Families lose patience. They haven’t a clue what to do. The professionals tell them to leave it to the professionals and don’t seem to get that the family is often dealing 24/7 with their relative. That’s why I’m a big fan of Krista McKinnon’s online training program, Recovering our Families. It’s groundbreaking in that it empowers the family, not the system. Alex, I am half way through your healing voices documentary and loving it. I’m assuming it’s okay if I report on my blog, with proper credit given.
Report comment
I totally hear you, Rossa, it’s overwhelming, confusing, and terribly frustrating for all concerned. And indeed, the support can be dismal and leave us all feeling rather abandoned.
Whether we call it ‘demeaning and stigmatizing’ or just plain judgmental, I do believe we’re talking about family cultural norms. I imagine most families are a mixed bag of compassion and judgment; for the most part we tend to vacillate based on how we feel at any particular time.
But some families can be rather extreme in their snobbery, which is from where I come. I had to shift a lot of false perceptions to find peace with myself, but I let them be who they are, too. I just have to set boundaries when they start projecting that crap onto me, and they take it…begrudgingly, of course, but they’ve learned to be more respectful, which is what I wanted from them. Self-respect was vital to assert after traversing the system.
And I 100% agree with the goal of family healing over giving it over to professionals. As I know you know from having read about all that you yourself have discovered in this journey, there is so much to learn ourselves which are simply not part of the ‘mental health professional’s’ schema–perspectives, tools, and outlooks which make all the difference.
I think it’s so beneficial to explore the healing world at large when seeking healing of any kind. There’s a lot of stuff out there now which is clearly replacing the old, for all the right reasons. And it’s working for people, that’s the main incentive.
And thanks, Rossa, definitely ok to post and share Voices That Heal anywhere, thank you so much. I’m so happy that you are enjoying it! Speaking my truth like this, from the heart and so front and center, had a miraculous and transformational impact on my life, so I figured it was the way to go 🙂
Thanks for the fantastic exchange, this was very rich for me.
Report comment
I do apologize for calling your documentary by the wrong name. It’s difficult to navigate through all the threads here, and your Voices that Heal got lost in translation.
https://www.youtube.com/watch?v=AtDGxJWmj5w
Report comment
“Many people, from what I read, appear to believe that the families were demeaning and stigmatizing from the get-go, and that’s WHY the person had a break. Consider, though, that it is very easy for families to become that way AFTER the person has had a break. It’s damn hard to live with someone in an altered state.”
You raise a very important point, Rossa, that goes to the chicken/egg -which came first distinction. Here is what the book Suspicious Minds, co–authored by Joel Gold, M.D., a psychoanalyst, has to say about “expressed emotion:”
“High EE does not contribute to people developing schizophrenia, but it is an important aspect of life for those living with it. Ironically, high EE is often stimulated by schizophrenia itself. As Gillian Haddock and Will Spaulding put it, ‘this behavior is generally considered to be a result of a normal reaction to the incredible stress associated with experiencing a relative who has a psychotic illness.'”
An argument for more, better and more effective support for affected families, a support that helps educate caregivers about how family dynamics can make things better or worse.
Report comment
People in this thread are working overtime to distance themselves from the word ‘blame’. It looks to me like the taboo is still very much in place.
Report comment
Seriously.
from dictionary.com:
Report comment
In the neutral sense of the word “blame” – to identify someone as responsible, i.e. as a causative agent – it is sometimes correct to blame parents for causing psychosis.
The problem is that when people hear the word blame, partly due to the loaded nature of the word with its guilt and anger-laden associations, they feel that it is a moral judgment on the worth of the parent. This is the heart of the problem. Parents who cause psychosis – and there are many who do – are not bad people, but usually inadequate parents who through no fault of their own were neglected and/or abused by their own parents, the grandparents, or had some other ill fortune befall them such as poverty.
So what should be distanced from is not the neutral meaning of the word blame – if there still is one, given how negative it has come to be interpreted- but the pejorative negative meaning that gets ascribed to the individual who is blamed.
It might be easier to say that some parents are responsible for causing their children’s psychosis (in part), or that some parents play a role in causing their child’s psychosis. The idea is to describe or be objective about phenomena that are occurring, not to morally blame or attack parents.
I would say the taboo is in place largely because of simpleminded people like (some) NAMI parents who need to think of themselves as “good”. Many of those parents probably have serious character problems themselves – a likelihood that almost certainly correlates with the ACE study and its finding of far more abuse and neglect in those offspring receiving serious mental health diagnoses. More abuse and neglect comes more often from parents who are worse parents and therefore more immature themselves.
So the fact that what these parents are being “charged with” – that they are poor parents who contributed to their children’s breakdowns – is unflattering, but the parents are not mature individuals who can accept unflattering self-analysis, makes it even harder for these immature parents to reflect upon what they did to the child and admit their role, rather than delude themselves that the child has a brain disease.
I wonder if I should submit this theory as an article to be published in the Huffington Post.
Report comment
You should :). Surely DJ Jaffe will be quick to follow up with one of his anti-trauma articles, though.
Report comment
I was also going to write a very scholarly article and try to submit it to HuffPo, about two recent drugs I’ve been developing in my secret laboratory:
Humiladol, the drug to treat symptoms of Narcissistic Personality Disorder in academic psychiatrists, an affliction which is disproportionately frequent yet undertreated in this population… the drug, of course, yields clinically significant increases in humility. A problematic side effect is that it sometimes causes psychiatrists to leave their profession. I am trying to develop an augmenting drug to treat this side effect.
And AntiDelusionol… this is a wonder drug I’ve been cooking up which can have the following effects on mental health workers:
– Make them stop believing that behavioral and psychological problems are brain diseases.
– Cause them to see people with problems as human beings on their level rather than “patients to be managed”.
– Lead them to realize that diagnoses are meaningless labels rather than a necessary lens for “understanding” someone.
The big side effect of AntiDelusionol is that drug companies tend to stop funding people who take this drug. So this side effect is intolerable to many people in the mental health industry.
But the problem is that when I test them out on human subjects, Humiladol and Antidelusionol keep failing to generate statistically significant results versus placebo. But I know that all I have to do is have 2 positive results to get them approved with the FDA. So I am still trying. I’ve done over 200 negative trials so far, but if #201 and 202 are positive then I’ll submit those and pretend the others didn’t happen.
If these drugs come out, I’ll trust you all on this comment thread not to leak the info about all the negative trials for Humiladol and Delusional. I could make a lot of money if this succeeds. Thanks.
Report comment
Don’t worry, our lips are sealed 🙂
Report comment
Thank you firewoman and Paris for your thoughts. Of course, I was joking about the Huffington Post… I need to remember to use my emoticons (the smiley face) to convey when it’s a joke in online writing.
It’s not that I wouldn’t submit an article, but because the politically correct editorial board there would never accept this type of article. Articles implicating family in causing serious emotional disturbance is too much for some people, and too much for almost all mainstream media. Sad, when it is so obvious.
As for DJ Jaffe, MIA guidelines prevent me from stating what I really think about him on this site.
Network causality and enemy images are interesting concepts. Enemy images (all-bad images of the other person) makes me think of all-bad splitting as a psychological defense. This is also a central defensive operation in the negative relationships between parents and children that can lead to serious problems, including psychosis, interestingly. Splitting is a normative response that humans use when they feel threatened both in early life (for example, the psychotic-child-to-be fearing the abusive mother and viewing her as an all-bad monster, rather than a complex person with her own history of problems) and also when they are threatened later in life (for example, NAMI parents threatened by the implication that they may be “bad” people who made their children, “ill”; they then reverse the situation to view themselves as “good” and the people making the suggestion become perceived “bad” people who “deny mental illness” and trivialize “brain disease”).
Report comment
I’m really appreciating hearing you all grappling with this important idea–how to both (a) take personal responsibility for the effects of one’s actions (and hold others accountable for such), while (b) not losing sight of network causality (i.e., the multiple factors beyond the individual that contributed to that behaviour–intergenerational trauma, oppressive social conditions, etc.). I think there are no easy answers, yet it’s essential that we find a way to do this–constructively without simply breeding more defensiveness and animosity. This is where I think it’s so important not to lose sight of the basic humanity of all involved (so note forming “enemy images” of each other), while also being willing to name the elephants in the room, speak truth to power, and invite all of us to become curious about the way that we all contribute to the social systems in which we’re embedded (family, community, nation, human society, biosphere,…). I’ll be discussing these ideas further in Part Three, and I hope to hear more from all of you then.
I think your thoughts on this are particularly well articulated, BPDTransformation (on this and the other topics on this post). That would be great if you could get some of your ideas onto Huffington Post(!)
Best regards,
Paris
Report comment
Blame is as toxic as the antipsychotic drug. Not at all helpful because it works in the past or on something outside ourselves. It is contrary to forgiveness, gratefulness, gratitude, and mindfulness. There is nothing healing about blaming your mother and backing that up with research, other than in extreme circumstances which would be rounding errors in this research. This is at the root of why madinamerica is important because it exposes the sellout in us. Why the mother…because Freud was a product of the times, maybe. Tom Cruise and Scientology make more sense than this and Scientology is way out there.
Keep it in perspective as you read it because providing a crutch can be disabling.
Report comment
“People in this thread are working overtime to distance themselves from the word ‘blame’. It looks to me like the taboo is still very much in place.”
It would be more accurate to say that writers and posters on MIA take pains to avoid using the word “blame” even as they blame away. There should certainly be no taboo on discussing the role that family dynamics (or anything else, for that matter) play in mental illness. As for blame, there are good reasons for restraining the blaming impulse absent evidence or basis for assigning blame or responsibility (think Bettelheim).
Report comment
I think to make change in this area, I think we do need to distance from the word “blame”. Is a single person to blame? In most cases, no, as early life trauma is typically a multigenerational problem.
Report comment
I’m not suggesting that a single person is to blame, and of course family issues are usually multigenerational. What I am saying is that people need to reflect on and take responsibility for the part – and it may be a limited part – they have played in the suffering experienced by others. In other words they do need to take part of the blame. Why is that so hard to say?
I’m not talking about the gossipy finger pointing that is rampant in our society; I’m talking about something responsible and constructive.
Report comment
I think blame is a such a loaded word in this context (going back to the days of refrigerator moms, etc) and will be interpreted in less than constructive way. It is the first thing about of many of the NAMI mommies mouth if you dare to touch on the topic and pretty much the end of the conversation with them, so I think it will not be helpful in making change, at least initially. I do like the idea of framing it more along the lines of taking some personal responsibility for not passing on the effects of bad things that happened to you.
Report comment
Fair enough, leave out the word ‘blame’ if you like and talk about personal responsibility instead. However I doubt that will make much difference to the NAMI mummies (and daddies). An entire industry has flourished because of these parents’ desire/need to attribute their children’s problems to faulty brain chemistry rather than anything remotely to do with them.
Report comment
Agree that it’s going to be an uphill battle with the NAMI crowd. But I do feel we have an obligation to try to change things, and should at least try to reach those who haven’t already been brainwashed. Just think it would be a good initial step to differentiate ourselves with our alternate perspective through some alternate language.
Report comment
I think it is correct that when a parent derives great benefit from viewing themselves as “good” via denying their input to the child’s problems (concurrently viewing the child as having a brain disease), that any attempt to shift the person’s perceptions is likely to be fiercely resisted at least initially.
One can enumerate the benefits that some NAMI parents – and also many non-NAMI parents – unconsciously gain from deluding themselves that their child has a brain disease:
– Being able to hold an image of themselves as a “good parent” while avoiding feeling guilt or shame for any abuse or neglect that actually occurred (this would, initially, cause the parent to view themselves as an intolerably bad “all-bad object”).
– Having the fantasy that their child’s problems can be “treated” with simple biological interventions, and thereby avoiding starting down the much more challenging but more rewarding road of having to grapple with difficult emotions and psychological conflict.
– Gaining the comfortable delusion that their child’s problem is something known and nameable (“schizophrenia”, the disease model), as opposed to something threatening, primordial, and unnameable, qualities which describe well the negative feelings that unconsciously torture the drugged children.
The psychopharmaceutical industry ably takes advantage of these parental vulnerabilities with its disease-model focusing on drugging. It’s a win-win-lose – a win for the drug company who make off with the cash, a “win” for the parent who feels it’s not their fault and is relieved from having to grapple with their children’s real problems, and a lose for the child who is sentenced to a lifetime of drugged nonfunctional misery.
In his writing, Harold Searles was struck by how families of psychotic children seemed to have great difficulty with uncertainty, always needing to “know” and be sure of reality, and rarely being able to hold ambivalent conflicting views. This covertly revealed the psychopathology and “borderline” way of thinking of many of these parents, who could only view things as all-good or all-bad. The same holds true of many NAMI parents today.
Report comment
“….the first thing about many of the NAMI mommies…”
I am no expert on the thinking of individual NAMI families (as opposed to the positions taken by the organization and its leadership). But the few mothers that I do know are disillusioned with the drugging paradigm, continue their search for answers, and keep asking themselves, over and over, what they may have done to cause their children’s mental illness. Some of them venture on this site, looking for answers, to encounter demonization about them and their motives. I do not see this type of demonization or wholesale indictment as helpful to the recovery movement. At some point, the discussion needs to go beyond MIA…to convince the larger society. If the NAMI parents, who, I believe, are for the most part, well motivated, are not on board, what hope is there to convince the larger society that the system of care needs to be rethought and reformed?
Discussing family dynamics as a factor in mental illness should not and must not be a taboo. Understanding mental illness must be a search for the truth, which means that nothing should be suppressed or distorted however inconvenient or difficult to face. By the same token, the sorry Bettelheim episode argues for some restraint in pointing fingers, without facts or basis. What exactly justifies the accusations hurled against “NAMI mommies” that is beyond the pale when it comes to parents of autistic children? It is now socially or politically beyond the pale to demonize parents of autistic children; rightly so. But research shows that some of the factors involved in autism (nutrient deficiencies, gut issues) are involved in mental illness as well. Most important, epigenetics shows how adverse environmental conditions (including abuse) changes people, and those changes are passed on making it that much more likely that future generations become successively more vulnerable to bullying, social isolation, parental neglect or abuse. Do family dynamics matters? Of course! How can they not. But questions that ought to be asked (and that argue for restraint when it comes to fingerpointing) include: does parenting or current life experience alone cause psychosis? Does this happen within a single generation, or does it take several generations before the successive harm manifests itself in psychosis or breakdown? There are too many instances of people with toxic childrehoods who did not lose their minds, and children of good parents who did break down. Taboo? No. But appropriate restraint? Absolutely.
Report comment
My experience has been the opposite of yours. i’ve seen a good number parents on places on NAMIs Facebook page/TAC/ people like Susan Inman and my non internet life who fiercely resist the idea that family dynamics are related to mental illness and that meds are the answer. I think of it as a form of not taking personal responsibility for their own adverse life experiences, by not even allowing the line of questioning that they may be passing down the fallout and contributing to their child’s problems . I have been accused of furthering stigma against those with “mental illness” by a relative ( who is heavily involved in NAMI) for relaying information about kids in foster care being at high risk of being drugged without any actual diagnosis and discussing the connection between child abuse and mental health problems. Note, the context of this situation was discussion of an article about using of antipsychotics in very young children, (not older teens, the age when her son started having problems…really this context was pretty far removed from her personally, yet she seemed to interpret it as an attack on her). Agree this is not all parents and I need to watch my stereotyping, but unfortunately this group of parents does exist and we need to think about how to relay this message effectively given their existence, particularly since a lot of them are heavily involved in outreach/promotion of these ideas .
Report comment
Discussing family dynamics as a factor in mental illness IS taboo in many circles, and in particular in any kind of event or posting I’ve ever seen from NAMI. There are many NAMI local chapters who are branching away from the national narrative, but the one thing you can count on is that “blaming parents” is 100% taboo, and all discussions of family dynamics are framed as parent-blaming. The “refrigerator mother”/autism concept is the one that is usually hauled out to make the speaker feel guilty and ignorant for raising the issue. The fact that every single “mental disorder” is highly associated with abuse history is not an allowable topic of conversation. “Trauma informed care” is starting to be allowable, but it appears that only extreme abuse is given credence as a possible contributing factor. Something as simple as a parent having unrealistic academic expectations or treating one child favorably over another can have long-term mental/emotional impacts of great significance, but this is not something we’re allowed to discuss.
There is unfortunately a conflict of interest for many parents who may not have done the best possible job raising their kids, in that it absolves them from responsibility if the “chemical imbalance” narrative were true. This is the bread and butter that NAMI was originally built around. The truth is unfortunately much more subtle and nuanced, but NAMI appears to allow only two positions: either you agree that parents play no causal role in mental/emotional challenges (unless they beat or sexually abuse their kids or something of the sort), or parents are “to blame,” i.e. 100% responsible for everything that happened. Both of these positions are absurd, of course, but that’s the propaganda that NAMI appears to put out there.
If all parties thought like you, we’d be able to have a rational discussion, but unfortunately, there are many (some on both sides of the issue) who aren’t willing to look at the actual facts of the situation and aren’t really interested in the truth.
Report comment
And BTW, I think it is normal and healthy for a parent to search his/her soul as to what s/he might have done to contribute to a child’s eventual experiences, even if they ultimately decide it was out of their control to influence. I had that experience with my son who went off the rails on drugs for a year or so and went through exactly those machnations and doubts. It can be very painful, but can also result in some insights that can help figure out what to do. Ultimately, I think it’s not healthy to go to a place of self-blame, but neither do I consider it healthy to go to a place of self-protection. We all contribute in one way or another to our children’s mental and emotional wellbeing, and to deny that is the case is just plain childish. Normal adults work to take responsibility for what they control, and to let go of what they do not. This is a very different process from self-recrimination – it’s an effort to assume responsibility for healing whatever damage may have been done and to help the child move on from it. To deny that opportunity to both parent and child is truly unhealthy for both.
— Steve
Report comment
“Something as simple as a parent having unrealistic academic expectations or treating one child favorably over another can have long-term mental/emotional impacts of great significance, but this is not something we’re allowed to discuss.”
Steve:
thanks for a great comment. I am on-board with everything you said, but see a bit of irony in one statement (cited above). Having unrealistic academic expectations or putting pressure on one’s children is sadly, way too common in our competitive society. But if this type of parental ill treatment were enough to cause psychosis or serious mental illness, we would have many more people breaking down. I know people who were far too demanding (including the wretched Tiger Mother) and their kids thrived under the pressure. And kids with good parents have broken down. Something else is in play, and that would be the nature factor. So I firmly agree that discussion of nurture and family dynamics should never be taboo (and to the extent they are on NAMI or elsewhere, that is wrong, wrong wrong). But nature, biology, predisposition, etc. etc. should not a taboo either. Everything matters, above all, the truth, which means that nothing should be beyond discussion or investigation.
By the way, I could not reply directly too you comment, and made an inadvertent “report” of one of your comments. Sorry about that…I did not mean to do a report or complain (I liked your comment); I was just hoping to find a way to reply directly to your comment.
Report comment
My problem with confronting my mother especially, with the negative influence she had on my life, is that my mother, has carried on her behaviour to my children, and now her great grandchildren, while just labeling me as the bad egg.
Report comment
“I do like the idea of framing it more along the lines of taking some personal responsibility for not passing on the effects of bad things that happened to you.”
Yes, totally agree–to stop the generational abuse. That’s where our personal inner work comes in handy, rather than to try and change others, or anything outside ourselves. In the moment, we can each be responsible for what we put out into the collective. Is it helpful? Necessary? Truthful? Harmful? Sabotaging? etc. Each one of us can take personal responsibility in present time, for what we offer to others.
Whom do we blame when we, ourselves, hurt others? We can also forgive ourselves and know we’re human, and we can make changes within ourselves, to ease up and lose judgment, to be more understanding and compassionate, more in control of ourselves when we feel conflicted or angry, we can all make that intention…or not. It’s a choice.
Report comment
Well said, Alex. Great point that forgiveness is part of the picture too….I think it’s important that we try to find ways to frame things in a more positive way than simply blaming. Another concept that is important here is resilience/post traumatic growth. I believe the latter is especially important…if we have to go through the experience of trauma, can’t we find a silver lining to the situation and with our awareness of how terrible and crippling it can be, do something constructive so others do not have to endure the same experience? That has been personally helpful for me (and I think others here).
Report comment
I think what some people call blaming can really be just to identify the root cause or network of issues due to trauma that is keeping a person weighted down. The resistance to identifying this is usually related to judgment, which we needn’t have, we can shift out of judgment.
From these core causes, usually there is a false belief–or more–that became internalized, due to repeated trauma, as a defense mechanism. Up to the time we awaken to this, we are unwittingly operating on a false premise, which is how we repeat negative patterns.
In later years, however, as post traumatic stress flourishes, I think that’s the time we can do present time work to actually shift those beliefs and perceptions, changing our internal relationship dynamic, that is, our relationship to ourselves. That actually releases the energy of the trauma, which pings our nervous system, making it particularly sensitive to certain triggers. Our nervous systems can be strengthened in many ways, very naturally.
So if we can shift our beliefs, release past time energy, strengthen our nervous systems, and come into present time with ourselves, we will undoubtedly make wiser choices for ourselves and our life will unfold in an entirely new way.
This is my practice, both personal and professional. Indeed, it’s my intention to help others have an easier time of it than I did. I learned a lot doing family healing work.
Thanks for your great comments, firewoman! I think they’re spot on.
Report comment
Indeed, I think it is the opposite of blame to honestly re-examine one’s personal behavior and ask if there is something that needs improving or healing. Blame is hurtful and aims at pulling someone down. True healing can be painful, but leads to opportunities that don’t happen if we act out of the fear of being blamed. It is not a choice between blame and blamelessness. It’s a choice between assuming and avoiding responsibility. Very, very different questions.
Report comment
I definitely feel that, indeed, self-responsibility is what we’re talking about here–which is what adults are in the position of teaching their kids, by example.
But I think that, more than ‘improving behavior’ (which can be a sticky issue, because off-beat behaviors may be justified by a situation or simply how someone expresses themselves, we just never know a person’s process until we explore it with them), I believe it’s about examining our thoughts and beliefs. This is where reality can shift, when we understand that what we think about and what we believe is exactly what creates the energy that draws any experience to us.
Healing is about shifting beliefs more than anything else, to my mind. Which, indeed, can be challenging, because it puts our entire reality into question. But that’s the only way to create change (aka healing)–whether internally or externally–out with the old and in with the new, and that pertains to belief systems, perceptions, and paradigms.
Report comment
I think a missing piece of this picture lies in the function of the nuclear family within capitalist society, because that’s primarily the kind of family being referred to (though perhaps Mr. Williams alludes to this somewhat in his response about family & community). The family is a microcosm of the larger social structure in many ways, and serves as a little unit of production for the capitalist machine. As such, the violence inherent in this system is channeled and reflected in family dynamics, as are the inherent inequalities of racism, sexism, etc. And, as is commonly acknowledged by family counselors, the member of the family who reacts to unspoken conflict either by pointing it out or via more convoluted means of expression is often singled out as “the problem” when they are more like the lightning rod. Individuality is bad for the bottom line.
When the family is in addition unaware of the larger social function it serves we end up with a collection of millions of families, each one cell in the larger membrane of corporate conformity, each with an “us against the world” mentality; deviation from assigned familial roles (which are not recognized as assigned roles) is considered immoral, criminal &/or pathological. Collective struggles are battled out by individuals unaware of the political nature of their “personal” disputes and other conflicts. This whole dynamic is most effective at dividing the population against itself, and positioning it to be manipulated and dominated.
Report comment
^This.
Report comment
Right on. Right. the. fuck. on.
Yes. Roles that are not recognized as assigned roles. That’s huge. Reading Friere’s stuff about that last summer is one of the things I feel best about doing in a while.
Report comment
Paris, I have another thought for you. You are doing such a great job in writing your job and generating public discussion about trauma-informed approaches to psychosis.
But it occurred to me just now, reading through the comment thread, how many other professionals speak to the public about psychosis like you do? Very few.
In the United States alone, there are over 100,000 psychologists (I know you are from New Zealand). http://www.apa.org/monitor/2014/06/datapoint.aspx
Probably at least a few thousand of these work with psychotic people, given that in ISPS alone there are several hundred paying members. Yet I can almost count on my hand psychologists I’ve seen write publicly about how trauma and family contribute to psychotic breakdown and to healing psychosis.
Please tell your fellow professionals that I (and I think others here too, probably) encourage more of them to speak up, and write up. If they are self-employed, it shouldn’t be a big professional risk. Not everyone can write a book like you, but more professionals can write and advocate publicly for trauma informed approaches to psychosis. It could make a big difference and provide a lot of hope.
I’m sure Mad In America would publish from a wider range of sources, and other online news forums would too if enough submissions started coming in. http://www.aeon.co would be another interesting idea – I encourage you to look up its articles on madness/mental illness, too. Aeon is just full of fantastic ideas.
Feel free to post this on the listservs that I know you’re a part of, and which I’m a silent observer of too. I know that many other skilled therapists think very much like you do about psychosis, but relatively few speak to the public outside of their closed circles and professional-only meetings. Maybe it’s time to change that.
Report comment
Hi BPDTransformation,
Thanks for your kind words and important suggestion to MH professionals to be more vocal about the serious problems within the field. I’ve generally noticed two different camps with regard to those who are not being particularly vocal (please forgive the overgeneralization):
(1) Professionals who have some awareness of the harm caused by rampant misinformation and corruption, especially by Big Pharma and associates, but are afraid to speak out and/or generally “rock the boat”—not wanting to risk their job, professional status, get a “tainted name,” etc…
…and (2) professionals who are honestly oblivious about such harm, fully buying into the Medical Model hook, line and sinker. I admit I initially found it hard to believe that someone could have the intelligence and devotion required to acquire a PhD or an MD and yet have such poor critical thinking skills that they could fall for a model that is clearly so oversimplified and doesn’t stand up to the recovery research well at all, but I’ve come to recognize that many such professionals really are this way—I think it’s akin to believers of a fundamentalist religion, with the “eyes” simply being too clouded over by dogma to see what’s right in front of them.
As for my passing on your comments to other organizations, I would be willing to do that, but I think it would be more effective and authentic to share these comments yourself. I’m open to further thoughts…
Best regards,
Paris
Report comment
Paris Williams ( Michael Cornwall and Amos Meacham)
Thanks for sending us your Madness and the Family…” I am assuming that Michael and Amos
have also read it, though I know they both are extremely tight for spare time.
What follows is a quick reply.
1) May I share your paper with your colleagues outside of the ISPS and families that might find the information and opinion helpful? I find that you offer more than issues relating to psychosis, but general review of different approaches to familial dysfunction (mine for one).
Concise and flows easily.
2) A suggestion for some future efforts from you is next. It is gratifying that you mention the toxic nature of poverty and responsibility of people with greater power. However, for me, I would like to read more on that issue. What follows next comes from a valued member of the ISPS – Ann-Louise Silver. Dr. Silver gave an online seminar about Chestnut Lodge with a concentration on Freida Fromm-Reichmann.
Curiously, at the beginning a fellow member of ISPS asked if there were questions. If we had some, we should write him and then he would give them to Ann-Louise. My question was whether Chestnut Lodge offered scholarships. When the moderator read off the questions, he did not read mine.
However, at the end, Ann-Louise asked for more questions. So, I spoke mine. She replied that all the patients at Chestnut Lodge were pains in the buttocks of wealthy families.
So, I am curious, Michael Cornwall, were there scholarships for I-Ward? If so, do you recall the details?
Also, Amos Meacham, I have been deeply involved with several families in Vermont since the early 1980s. Several of those individuals are wonderful people that could have used Soteria and now they are struggling with a lifetime of intermittent hospitalization and medication. Further, knowing how I am a Permissive-Democrat parent (to use Paris Williams) and my wife can be a jack-boot Authoritarian parent, it is a miracle that our teenage son has not fallen into a Double-Bind. However, if he does, I assume that whatever subsidy comes to Vermont people to live at Soteria
would not be available to him since he is out of state and not even a U.S. citizen.
In short, we need to speak out how there is abundance of psychiatrists that will meet poor folk for 15 minute quickies to refill medication. There is also a fair amount mediocre group therapy for those that would be rejected from Chestnut Lodge, etc. For more than a half century, I have been a support person who is frequently admitted to psychiatric units. Recently he was months in a unit, in the center of Washington, DC, does not even have a room for ping-pong or any sort of patient lounge with a small library. The only activity outside of his shared room was hanging out at the Nursing station. Any optimism in your paper, Paris Williams, is reserved for those with a good deal of surplus wealth. Any positive aspiration for the future is tepid melodrama unless we carefully look at what is available to those with minimal income.
3) Lastly, I really appreciate pagination.
4) Your effort is appreciated and I look forward to sharing it with others!
-David Lee
Report comment