When you get a diagnosis of depression, the first line treatment is often antidepressant medications. Unfortunately, initial treatment with antidepressants fails to resolve depression approximately two-thirds of the time. Once that treatment fails, doctors turn to other strategies—often including switching medications, or adding on additional medications, often antipsychotics.
Now, a new study has examined what treatment strategies are effective when initial antidepressant medications fail to work. The researchers found that while antipsychotics may be slightly more effective than alternative antidepressants, they come with a much higher side effect burden.
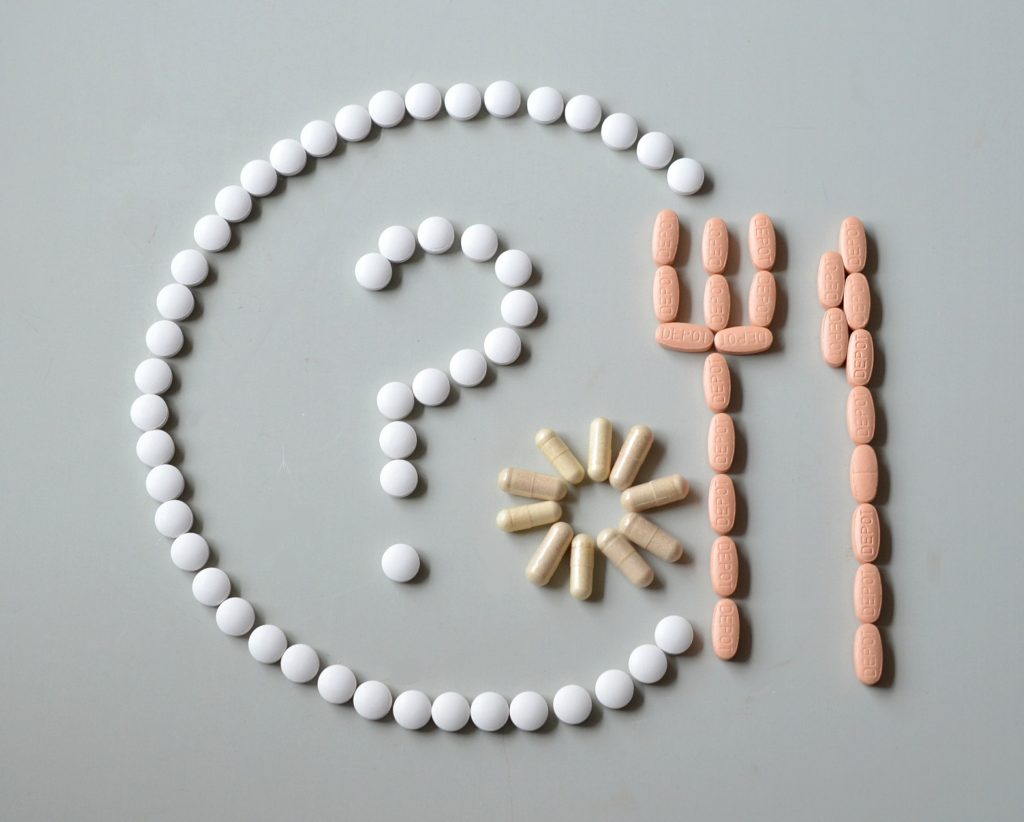
The researchers investigated whether bupropion (an alternative antidepressant, brand name Wellbutrin) or aripiprazole (an atypical antipsychotic, brand name Abilify) was more effective at reducing depressive symptoms. They also identified the side effect burden of each approach. While bupropion increased anxiety, aripiprazole was associated with more serious side effects such as akathisia (involuntary movement disorders) and weight gain (which indicates metabolic problems).
The data comes from a new large, randomized study called the VAST-D trial, which ran from 2012 to 2015. The 1,522 participants came from 35 Veterans Health Administration sites, and all had a diagnosis of major depressive disorder. Participants had an average of around 2.5 previous trials of medication, which had not resulted in remission (scoring below the clinical threshold on the measure of depression).
The VAST-D trial randomized participants to one of three groups:
- Switching to bupropion (the alternative antidepressant Wellbutrin)
- Adding bupropion to current antidepressant treatment (augmenting)
- Adding aripiprazole (the atypical antipsychotic Abilify) to current antidepressant treatment (augmenting)
The study followed participants for 36 months, providing a slightly longer term for outcome data than previous studies.
It is important to note that the study did not include control groups such as placebo groups or usual treatment groups, so the researchers cannot rule out placebo effects or state that their treatments would be better than usual care.
Aripiprazole treatment was slightly more likely to result in improvement in both depressive symptoms (measured by the clinician-rated QIDS-C16 scale) and global improvement (measured by the clinician-rated CGI scale). 74.3% of those who augmented with aripiprazole had improvement, compared to 65.6% of those who augmented with bupropion, and 62.4% of those who switched to bupropion.
However, both bupropion and aripiprazole augmentation resulted in similar remission rates (people who no longer met criteria for depression): 28.9% of people who augmented with aripiprazole experienced remission, as did 26.9% of those augmenting with bupropion, and 22.3% of those who switched to bupropion.
The results suggest that aripiprazole is perhaps slightly more effective than bupropion at reducing depressive symptoms in those who have previously tried other antidepressants.
However, aripiprazole was much more likely to induce serious side effects:
- Somnolence (14.5%). Somnolence is a type of sedation. This essentially equates to feeling so exhausted as to be unable to engage in activities.
- Akathisia (14.9%). Although researchers generally associate this movement disorder with earlier antipsychotic medications, its prevalence here demonstrates that current-generation antipsychotics carry a significant risk as well. Sadly, akathisia is often undiagnosed, as patients often have a hard time finding words for the overwhelming, painfully intolerable restless feeling. Researchers link akathisia to increased suicidality.
- Extrapyramidal Side Effects (19.2%). These reactions generally include akathisia as well as other movement disorders such as tardive dyskinesia and Parkinsonism. One in five people taking aripiprazole experienced some form of this.
- Weight gain (25.2%). More than a quarter of people taking aripiprazole experienced significant weight gain, which is often an early sign of drug-induced metabolic conditions such as diabetes.
Other symptoms, such as headache, dizziness, and nausea, were experienced by 15-20% of people in each group.
The authors note that the sample was overwhelmingly male (85%), and the average age was 54, making the sample very different from previous research. Additionally, participants were likely to have a comorbid diagnosis of post-traumatic stress disorder, and the researchers theorized that the benefits of aripiprazole might be due to that diagnosis, rather than depression.
Although some researchers tout the efficacy of antipsychotic augmentation for depression, these studies have been criticized for failing to account for the low quality of evidence and the risk of dangerous side effects. A meta-analysis by the Cochrane Collaboration described the data as “limited” and “based on a rather small number of randomised participants” and noted that antipsychotic augmentation was “associated with worse tolerability, mainly due to sedation, weight gain or laboratory values such as prolactin increase.”
In fact, recent guidelines in Finland and Germany have stated that augmentation with antipsychotics should not be recommended due to the high risk of adverse effects and the relatively slight evidence of benefit. According to the VAST-D researchers,
“Given the small effect size and adverse effects associated with aripiprazole, further analysis including cost-effectiveness is needed to understand the net utility of this approach.”
**
Editors’ Note: Peter Simons is also the lead author of “Antipsychotic augmentation for major depressive disorder: A review of clinical practice guidelines” (Link)
****
Mohamed, S., Johnson, G. R., Chen, P., Hicks, P. B., Davis, L. L., Yoon, J. . . . Zisook, S. (2017). Effect of antidepressant switching vs augmentation on remission among patients with major depressive disorder unresponsive to antidepressant treatment: The VAST-D randomized clinical trial. JAMA, 318(2), 132-145. doi:10.1001/jama.2017.8036 (Abstract)















Akathisia is not an involuntary movement disorder. A voluntary compulsion to move maybe an ostensible manifestation, but what it really is, is drug toxicity inducing toxic psychosis and a very serious condition indeed. As I recall Gwen Olsen said this augmentation BS, was just a marketing excuse via ‘treatment resistant depression’ (when the treatment doesn’t work in the first place and is fraudulently promoted) to pump people with anti-psychotics. We do not need any studies on it, we just need people to expose for what it is: very dangerous to human health fraud.
With regards the percentage figure for Akathisia, this can not be given because becoming toxic can also be contingent upon the common food stuffs, herbs and spices that block, inhibit and attenuate the CYP 450 enzyme system as well as the phenotypes. This is why it is important to know about pharmacogenetics.
Report comment
There you go – Gwen Olsen on SSRI/anti-psychotic augmentation :
https://www.youtube.com/watch?v=bMPTHy1GrYo&feature=youtu.be&t=2804
Report comment
Or when dysperceptive patients are misdiagnosed and get started on erroneous treatments that magnify side effects, but minimize the likelihood of therapeutic results.
Report comment
Very well said!
Report comment
All doctors learn in medical school that combining the antidepressants and/or antipsychotics can make a person “psychotic” via anticholinergic toxidrome.
“The symptoms of an anticholinergic toxidrome include blurred vision, coma, decreased bowel sounds, delirium, dry skin, fever, flushing, hallucinations, ileus, memory loss, mydriasis (dilated pupils), myoclonus, psychosis, seizures, and urinary retention … Substances that may cause this toxidrome include the four ‘anti’s of antihistamines, antipsychotics, antidepressants, and antiparkinsonian drugs[3] as well as atropine, benztropine, datura, and scopolamine.”
https://en.wikipedia.org/wiki/Toxidrome
Did they check for what percentage of people had a first “psychotic” break when unwisely combining the antidepressants and/or antipsychotics? And shouldn’t it be considered unethical to encourage giving people drug cocktails that are already medically known to make people “psychotic”?
Report comment
Just check where Abilify is advertised as an add – on (“If your anti-depressant isn’t working”…) People magazine, and many of the “women’s” magazines….just appalling!
Report comment
what a terrible problem with this abilify….the money that was made $$$$$$$$$$…and the dangers..
if a doctor wants to augment they need to recommend healthy eating and healthy exercise…
Report comment
Those negative effects are at appallingly high rates.
Report comment
This way of testing psychotropic drugs makes no sense and is thoroughly dishonest. There is no doubt that opiates would have “excellent results” on depression if they were tested in the way that antidepressants or now neurleptics are.
Turning people into addicts because they have had problems is a criminal social choice determined by the sordid rapacity of psychiatrists and the pharmaceutical industry. All drug dealers should be put in jail, especially psychiatrists and industry executives.
Report comment
No placebo? Big shortcoming of this study
Report comment
These are not “medications”, they are “drugs” or more specifically, neurotoxins.
They are often given after patients deteriorate on the basically dangerous and ineffective anti-depressants and anti-anxiety drugs they are
prescribed by inept doctors.
Report comment
Abilify was added on top of antidepressants by my psychiatrist when I was a teenager. I’m frankly surprised I survived it. My blood still runs cold when I see an Abilify ad.
Report comment
Note that this is not a recent issue. Also, wasn’t this horrible toxin just approved for compliance tracking with a microchip?
http://www.cchrflorida.org/abilify-side-effects-lead-to-law-suits/
Report comment
Yes, our wonderful FDA, tasked with watching over our safety, just approved the use of the microchip version of this awful drug. Go figure.
Report comment
The FDA is a totally compromised agency. One inside told me that they won’t place a warning on a label until “there are bodies in the street and front-page headlines about the side effects”. And it’s true.
Report comment
First of all, depression is not an illness. It is a reaction in our lives that tells us that something isn’t right and needs to be worked on.
Secondly, none of these drugs, neither the antidepressants nor the neuroleptics, actually cure depression. What they do is keep us from being in touch with our feelings and emotions so that we end up not being bothered by anything. These drugs basically change people into zombies who end up experiencing very little feeling for others around them and not even much feeling for their own selves. On top of this both types of drugs have all kinds of detrimental effects. I don’t refer to them as side-effects because that is doing nothing but playing word games in order to try and make the situation better than it really is. Some people placed on antidepressants actually experience suicidal and homicidal feelings which they often end up acting on, causing a lot of grief and hardship for others as well as themselves.
I see the effects of these drugs in peoples’ lives each and every day that I go to work. These are not medicines they are very addictive drugs with horrible effects, drugs you must taper off of very carefully because they cause terrible withdrawal. The use of these drugs is the cause of low recovery rates among those of us labeled as the “mentally ill”. Recovery for most people lies in getting off these damned drugs. We now have plenty of studies to prove this, no matter what psychiatrists or the drug companies say.
Report comment
I could not have said it better.
Report comment
How does a drug get approved that has marginal “benefits” and clear and dramatic adverse effects? Corruption is the only answer. Abilify should NEVER have been approved for this use. Taking neuroleptics for depression is like taking speed to help you sleep.
Report comment
What this does not address is the difficulty in coming off “atypical antipsychotics” like Abilify, Zyprexa, and Seroquel. I have helped people with all three.
All of them hit a shotgun spray of neurotransmitters, depending on the level of drug. For example, at low doses, Seroquel hits histamine receptors, then serotonin receptors, then dopamine receptors.
At an equivalent dose, Zyprexa will be heavy on the dopamine and serotonin receptors, and Abilify will be also hitting norepineprine receptors.
What receptors they hit are dose dependant. So here’s the rub – when tapering, all of a sudden at 75 mg of Seroquel, the dopamine action drops out – and the dopamine receptors go into full blown withdrawal. You can still sleep (because the histamine receptors will still be hit), and there may be a mild serotonin effect – but – you’ve just gone all the way off your dopamine drug – even though you are still on the drug.
This is worse with Zyprexa, and worse still with Abilify, which hits on 11? neurotransmitter sites.
(though, the chart here, says Seroquel is the most complex, and Abilify the simplest – but – in my work with helping people taper, the opposite seems to be true. I am not a biochemist: http://cdn.neiglobal.com/content/practiceres/posters/50188_nei_009_bindings.pdf )
Additionally, some of them are agonist and some of them are antagonist – complicating the neurotransmitter soup significantly.
These drugs are hell to come off of.
Report comment
jancarol———-good info you are giving here…have you seen anyone benefit long term from abilify augmentation….
Report comment
I’m sorry littleturtle, I wish I had something good to say. My work is about getting people off of these drugs – and so – I see the ones who have trouble. I don’t know anyone who has augmented ANY neuroleptic (marketed as “antipsychotic”) who doesn’t regret it, but that may just be the field in which I work. And the longer term they are on it, the worse it is.
From where I stand, the risks are greater than the rewards. Peter Breggin calls them neurotoxins, and I’m inclined to agree. Rewards may be short term – but the longer you are on a drug, and the more drugs you are on, and the more drug changes you’ve been through – the harder it is to come off of them.
And when I say harder – think about how hard it is to come off your Celexa. Make it worse by a factor of 3-10. Heroin addicts have found that a heroin withdrawal was a piece of cake compared to antidepressant and / or benzo withdrawal. And the media isn’t reporting this, they’re more concerned with the “opioid crisis” than the people dying and disabled from these drugs.
If I were you, I’d learn how to taper the Celexa carefully and safely, and take up running or aikido or dancing or painting to express your emotions safely, and become friends with your emotions. Then at least you will be authentic, and off the rollercoaster.
Report comment
thanks jancarol
Report comment
janCarol – you are doing righteous work. Keep it up!
Report comment
I had a roommate who listened to his psychiatrist and took Abilify to “increase the effects” of the Zoloft he was taking. After only one dose he was hallucinating and hallucinated for the next four days. It was awful. The combination made him psychotic. He couldn’t sleep nor even lay down to rest and ran out into the snow without coat or shoes on. He heard the dog drinking water out of her water bowl and told me that his friend from another city was there (he wasn’t) and then called his friend’s name and told him to quit drinking out of the dog’s bowl. I knew then that he was in trouble and it only went downhill from there.
Report comment
There’s a **reason** that “akathisia is often undiagnosed”, as the article correctly states….
Akathisia is IATROGENIC.
It’s more correct to say that “akathisia is RARELY diagnosed”….
Honesty and medical ethics are obsolete concepts which have no place in the Brave New World Order
of PhRMA 2017….
Otsuka Pharma is the drug dealer behind Abilify, and they are also one of the leading payer$ of kickbacks to “doctors”/drug dealers known as “psychiatrists”…. Even a local shrink here in small-town New Hampshire, Dr. Shawn Shea, received over $10,000. in 2 years from them, as a “consultant”. Those facts can be found in the “Dollars For Docs” database which ProPublica has produced online….
God Bless you all, but we’re really chatting about a global-scale DRUG RACKET, which is harming, torturing, and even KILLING people for profit, and calling it “healthcare”.
The ironic thing, is that given the literally 1,000,000s of folks drugged by these neuro-toxins globally, there actually *are* some folks, – a very tiny percentage, – who do seem to be “helped” by these drugs….
Report comment