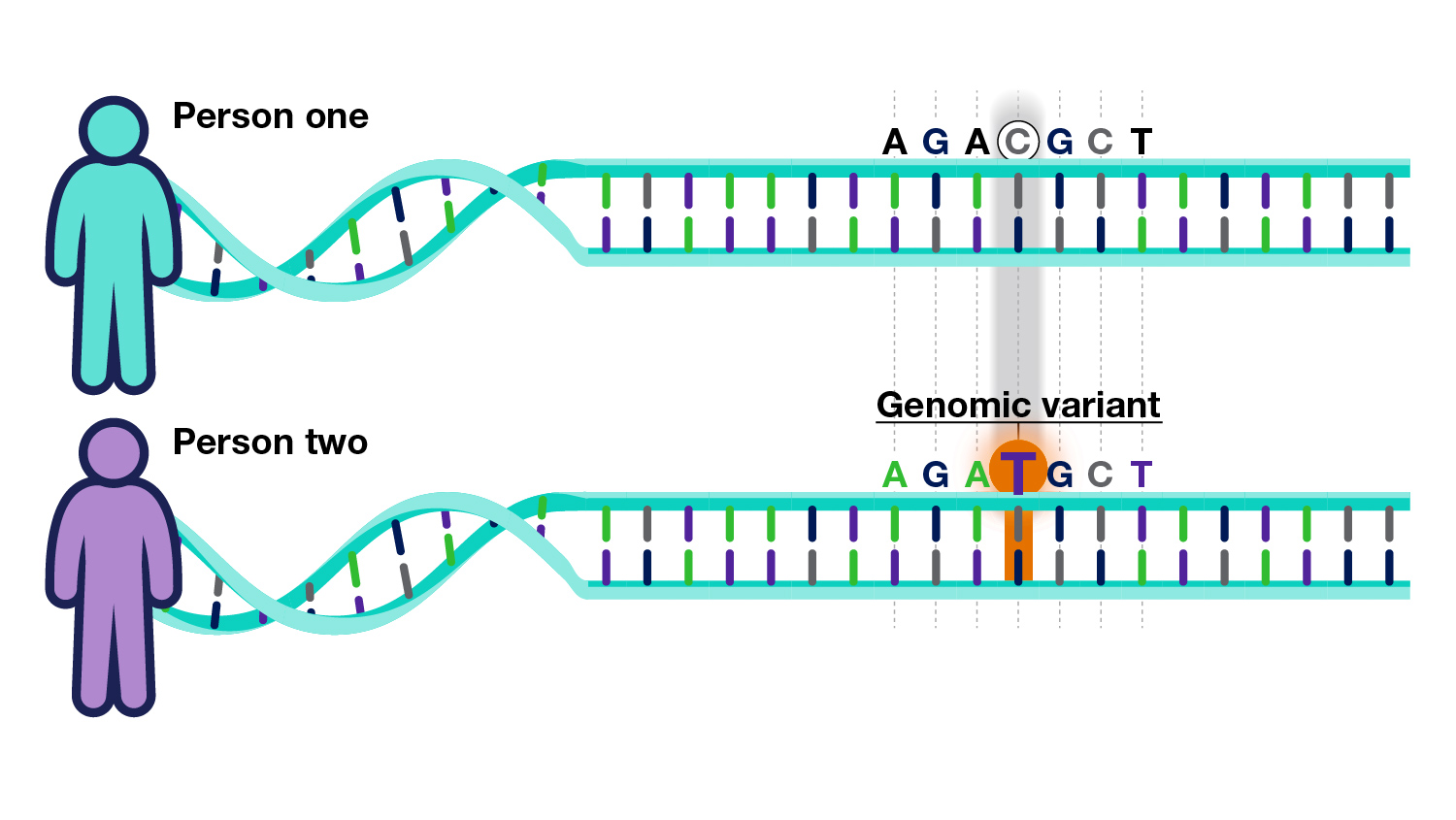
The “polygenic risk score” (PRS) is a metric used to calculate the potential impact of combinations of thousands of genetic variants on health. It could theoretically improve the detection and treatment of various health concerns if they are dependent on lots of small increases in risk rather than driven by one or two powerful genetic factors.
Researchers theorize that “mental illness” is based on such a polygenic risk—that is, thousands of genetic variants combine to increase the likelihood of a person being diagnosed with a psychiatric disorder.
However, despite large-scale research, the PRS has, as yet, shown no clinical utility in psychiatry.
In a new article in JAMA Psychiatry, researchers review the potential use of the PRS. The article’s lead writers were Graham Murray and Naomi Wray at the University of Queensland, Australia.
 Murray and Wray based their review on the assumption that current high-end estimates of PRS influence on psychiatric diagnosis risk are correct (i.e., that the PRS score can explain 11% of the risk for schizophrenia and 4% of the risk for depression). However, other studies have found much lower explanatory power for the PRS.
Murray and Wray based their review on the assumption that current high-end estimates of PRS influence on psychiatric diagnosis risk are correct (i.e., that the PRS score can explain 11% of the risk for schizophrenia and 4% of the risk for depression). However, other studies have found much lower explanatory power for the PRS.
For instance, a recent study found that PRS predicted about 0.5% of the risk for schizophrenia. In that study, life experiences, social circumstances, family history, and pain were all far better predictors of whether someone would receive that diagnosis (in total, these factors could explain 17% of the risk for schizophrenia).
Another recent study, also in JAMA Psychiatry, found that genetic testing could explain less than 1% of whether someone would receive a diagnosis. Another study found that even sequencing the entire genome explained only 2.28%. On the high end of the estimates, one study found that genetic causes explained 3.4% of whether a person received a diagnosis.
Some researchers have looked farther afield, to the “exome”—but they also found that their genetic results provided no useful data, even when looking at genes traditionally associated with psychiatric disorders.
Nonetheless, Murray and Wray proceeded with the assumption that the PRS could explain 11% of the risk for schizophrenia. With this assumption, they calculated the risk for the people who had the highest PRS: the risk was three times higher for people in the top 10% of the PRS and six times higher for those in the top 1%.
However, these relative risk numbers are clinically useless, as Murray and Wray explain:
“These statistics, while impressive in terms of relative risk, are unlikely to affect public health strategies, given that nearly all of the people in each stratum will never get the disorder (low absolute risk).”
This is because the prevalence (how many people actually get the diagnosis in the general population) is low. For instance, about 1% of people get a schizophrenia diagnosis in the general population. Those with the highest possible PRS score are at a sixfold higher risk—meaning that about 6% of people with the highest possible PRS score will receive a schizophrenia diagnosis.
That means that even assuming the highest possible risk score, and assuming that the PRS is more accurate than other studies have found it to be, it is still clinically useless—94% of the people who have the highest possible score will not go on to receive a diagnosis of schizophrenia.
Again, this is because psychiatric diagnoses are far more correlated with experiences like trauma, abuse, deprivation, poverty, and pain than they are with actual genetics (for instance, a study in Lancet Psychiatry found strong effects for a number of life experiences, but no detectable effect of genetics on risk for schizophrenia.)
Nonetheless, Murray and Wray conclude that “Polygenic risk scores will contribute to risk assessment in clinical psychiatry as it evolves to combine information from molecular, clinical, and lifestyle metrics.”
They advocate for including the PRS along with other metrics, such as stressful life events and trauma. It is unclear what benefit the PRS would add to those metrics.
Murray and Wray write that the utility of PRS is clear in some areas of medicine (heart disease and cancer) for which there are specific screening and effective preventive strategies.
However, they acknowledge that “In psychiatry, there are no such screening programs, and so an immediate utility is not as clear.”
They also note the risk of the “nocebo” effect: that people who are told they are at high risk of a psychiatric disorder may have a worse experience, even if it is untrue:
“Participants in a study who were told they had a high genetic risk for depression reported more depressive symptoms in the previous 2 weeks than people told they had tested low for genetic risk of depression, even though no test took place and test results were randomly assigned.”
Because of the potential harms and the lack of clinical utility, the researchers suggest that population screening is not warranted at this time. “We do not believe that population screening is the appropriate place to begin the investigation of PRS in psychiatry,” they write.
The researchers then begin to theorize about some potential uses for the PRS, despite its flaws. They write that it may someday be used to provide guidance on differential diagnosis: that is, if the person’s “symptoms” do not fully match the criteria for specific diagnoses in the DSM, the PRS could be used to tell the clinician which slightly-similar diagnosis is the best match. However, since the PRS overlaps considerably between different diagnoses and has low predictive value, it is unclear how this would be an improvement.
Additionally, the researchers theorize that the PRS may one day be used to distinguish who has a good prognosis for treatment and who does not. They note that it cannot yet do so, but they hope someday it could. Again, the nocebo effect could hamper its utility: if people are told they have a poor prognosis for treatment, it may actually cause treatment to become less effective. It’s unclear how this could be helpful.
****
Murray, GK, Lin, T, Austin, J, McGrath, JJ, Hickie, IB, & Wray, NR. (2020). Could polygenic risk scores be useful in psychiatry? A review. JAMA Psychiatry. Published online, October 14, 2020. DOI:10.1001/jamapsychiatry.2020.3042 (Link)














Szasz said and wrote that choices are not in the DNA. People make choices to behave good or badly.
https://youtu.be/Qj7GmeSAxXo?t=102
Report comment
Even assuming there is a genetically caused thing one could call schizophrenia, it would never be found, because the diagnostic process is such trash, that it barely improves upon monkeys assigning diagnosis by throwing darts. If even at all.
If most of the people called schizophrenic in fact aren’t, you’re not going to find what causes schizophrenia.
Assume schizophrenia is 100% explained by genetics. For a study of the entire genome to find only 2%, you’d have to have 98% missdiagnosis ratio.
Report comment
And don’t forget, all those misdiagnosed “schizophrenia” patients can have the symptoms of “schizophrenia” created with the “schizophrenia” treatments.
Since the neuroleptics / antipsychotics can create the negative symptoms of “schizophrenia,” via neuroleptic induced deficit syndrome. And they can create the positive symptoms of “schizophrenia,” via anticholinergic toxidrome.
I must say, however, all this continued spending and research into the “invalid” DSM disorders should stop at some point. DSM based psychiatric research was supposed to be defunded in 2013, according to the head of the NIMH at the time.
Report comment
“about 1% of people get a schizophrenia diagnosis in the general population.” It’s half less.
“Of the 132 core studies, 21 studies reported point prevalence, 34 reported period prevalence, and 24 reported lifetime prevalence. The median prevalence of schizophrenia was 4.6/1,000 for point prevalence, 3.3/1,000 for period prevalence, 4.0 for lifetime prevalence, and 7.2 for lifetime morbid risk. […] Several important findings emerge from Saha and colleagues’ analysis. For clinicians, the analysis indicates clearly that lifetime prevalence is 4.0/1,000 and not 1%, as reported in the Diagnostic and Statistic Manual of Mental Disorders, fourth edition, and other textbooks.”
Dinesh Bhugra (2015), The Global Prevalence of Schizophrenia
Since the diagnosis of schizophrenia is not based on biological but cultural observations, it does not make sense to look for genetic causes that are relatively fixed, to a cultural phenomenon that is changing. This is typically the kind of situation where one can find correlations without causality.
Example: Suppose that for cultural reasons, people with blue eyes inspire less confidence and are more likely to be diagnosed with schizophrenia. Blue eyes are genetically determined. We will therefore find a correlation between the genetic factors that determine the color of the eyes and schizophrenia. This correlation is not a causality.
Trustworthy-Looking Face Meets Brown Eyes
Genetics determine many traits in living things, but these traits are then interpreted culturally, often unconsciously. Schizophrenia is typically the interpretation of a cultural phenomenon, without biological observation. The limited correlations of schizophrenia with genetics do not therefore mean anything in particular.
Report comment
Sylvain,
I do not remember the syntax to embed links, to make things bold, italic, underlined etc. Could you please post it here? I can’t seem to find it anywhere on MIA.
Report comment
This is html.
Report comment
Thanks.
Report comment
If Im correct there is no proof that human behaviour is driven by genes.
Report comment
Human behaviour ( like animal behaviour) is driven by genes in a way, the urge to reproduce. If the animal or human doesn’t have the behaviour, you know the results, they don’t have offspring.
“The Contest” is the 51st episode of the NBC sitcom Seinfeld.
https://www.youtube.com/watch?v=wGhg-htVnJ0
seinfeldscripts.com/TheContest.htm
GEORGE: Oh boy..
JERRY: What are we doing here..?
GEORGE: ..Oh boy.
JERRY: This is ridiculous.
GEORGE: Do you believe this? We’re fighting. We’re fighting.
JERRY: I haven’t been myself lately. I’ve been snapping at everybody.
GEORGE: Me too. I’ve been yelling at strangers on the street.
REMEMBERING MASTURBATORY INSANITY
http://www.szasz.com/iol8.html
Report comment