“Depression is a serious medical condition that may be due to a chemical imbalance, and Zoloft works to correct this imbalance.”
Herein lies the serotonin myth.
As one of only two countries in the world that permits direct to consumer advertising, you have undoubtedly been subjected to promotion of the “cause of depression.” A cause that is not your fault, but rather; a matter of too few little bubbles passing between the hubs in your brain! Don’t add that to your list of worries, though, because there is a convenient solution awaiting you at your doctor’s office…
What if I told you that, in 6 decades of research, the serotonin (or norepinephrine, or dopamine) theory of depression and anxiety has not achieved scientific credibility?
You’d want some supporting arguments for this shocking claim.
So, here you go:
The Science of Psychiatry is Myth
Rather than some embarrassingly reductionist, one-deficiency-one-illness-one-pill model of mental illness, contemporary exploration of human behavior has demonstrated that we may know less than we ever thought we did. And that what we do know about root causes of mental illness seems to have more to do with the concept of evolutionary mismatch than with genes and chemical deficiencies.
In fact, a meta-analysis of over 14,000 patients and Dr. Insel, head of the NIMH, had this to say:
“Despite high expectations, neither genomics nor imaging has yet impacted the diagnosis or treatment of the 45 million Americans with serious or moderate mental illness each year.”
To understand what imbalance is, we must know what balance looks like, and neuroscience, to date, has not characterized the optimal brain state, nor how to even assess for it.
A New England Journal of Medicine review on Major Depression, stated:
” … numerous studies of norepinephrine and serotonin metabolites in plasma, urine, and cerebrospinal fluid as well as postmortem studies of the brains of patients with depression, have yet to identify the purported deficiency reliably.”
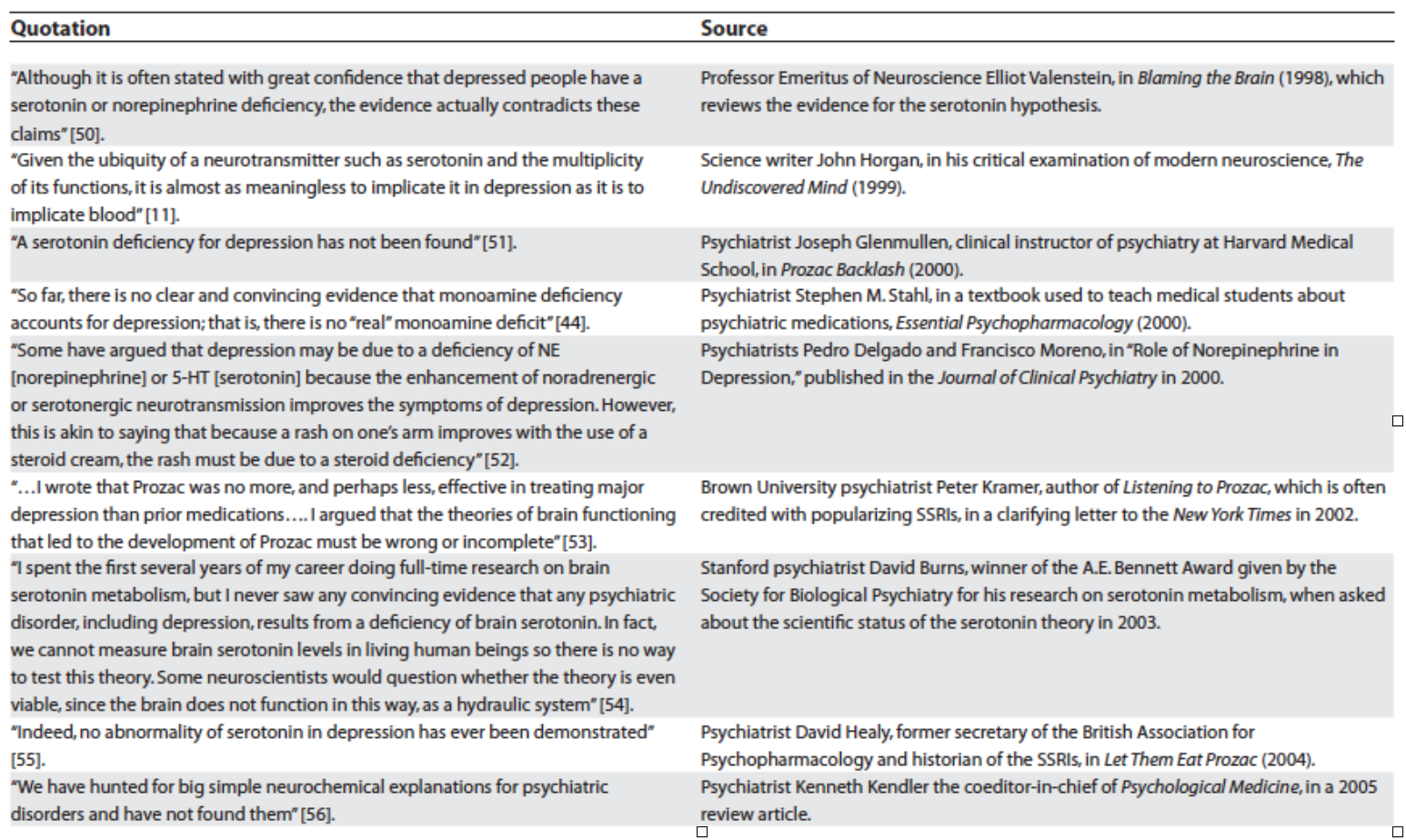
The data has poked holes in the theory and even the field of psychiatry itself is putting down its sword. One of my favorite essays by Lacasse and Leo has compiled sentiments from influential thinkers in the field – mind you, these are conventional clinicians and researchers in mainstream practice – who have broken rank, casting doubt on the entirety of what psychiatry has to offer around antidepressants:
Humble Origins of a Powerful Meme
In the 1950s, reserpine, initially introduced to the US market as an anti-seizure medication, was noted to deplete brain serotonin stores in subjects, with resultant lethargy and sedation. These observations colluded with the clinical note that an anti-tuberculosis medication, iproniazid, invoked mood changes after five months of treatment in 70% of a 17 patient cohort. Finally, Dr. Joseph Schildkraut threw fairy dust on these mumbles and grumbles in 1965 with his hypothetical manifesto entitled “The Catecholamine Hypothesis of Affective Disorders” stating:
“At best, drug-induced affective disturbances can only be considered models of the natural disorders, while it remains to be demonstrated that the behavioral changes produced by these drugs have any relation to naturally occurring biochemical abnormalities which might be associated with the illness.”
Contextualized by the ripeness of a field struggling to establish biomedical legitimacy (beyond the therapeutic lobotomy!), psychiatry was ready for a rebranding, and the pharmaceutical industry was all too happy to partner in the effort.
Of course, the risk inherent in “working backwards” in this way (noting effects and presuming mechanisms) is that we tell ourselves that we have learned something about the body, when in fact, all we have learned is that patented synthesized chemicals have effects on our behavior. This is referred to as the drug-based model by Dr. Joanna Moncrieff. In this model, we acknowledge that antidepressants have effects, but that these effects in no way are curative or reparative.
The most applicable analogy is that of the woman with social phobia who finds that drinking two cocktails eases her symptoms. One could imagine how, in a 6 week randomized trial, this “treatment” could be found efficacious and recommended for daily use and even prevention of symptoms. How her withdrawal symptoms after 10 years of daily compliance could lead those around her to believe that she “needed” the alcohol to correct an imbalance. This analogy is all too close to the truth.
Running With Broken Legs
Psychiatrist Dr. Daniel Carlat has said:
“And where there is a scientific vacuum, drug companies are happy to insert a marketing message and call it science. As a result, psychiatry has become a proving ground for outrageous manipulations of science in the service of profit.”
So, what happens when we let drug companies tell doctors what science is? We have an industry and a profession working together to maintain a house of cards theory in the face of contradictory evidence.
We have a global situation in which increases in prescribing are resulting in increases in severity of illness (including numbers and length of episodes) relative to those who have never been treated with medication.
To truly appreciate the breadth of evidence that states antidepressants are ineffective and unsafe, we have to get behind the walls that the pharmaceutical companies erect. We have to unearth unpublished data, data that they were hoping to keep in the dusty catacombs.
A now famous 2008 study in the New England Journal of Medicine by Turner et al sought to expose the extent of this data manipulation. They demonstrated that, from 1987 to 2004, 12 antidepressants were approved based on 74 studies. Thirty-eight were positive, and 37 of these were published. Thirty-six were negative (showing no benefit), and 3 of these were published as such while 11 were published with a positive spin (always read the data not the author’s conclusion!), and 22 were unpublished.
In 1998 tour de force, Dr. Irving Kirsch, an expert on the placebo effect, published a meta–analysis of 3,000 patients who were treated with antidepressants, psychotherapy, placebo, or no treatment and found that only 27% of the therapeutic response was attributable to the drug’s action.
This was followed up by a 2008 review, which invoked the Freedom of Information Act to obtain access to unpublished studies, finding that, when these were included, antidepressants outperformed placebo in only 20 of 46 trials (less than half!), and that the overall difference between drugs and placebos was 1.7 points on the 52 point Hamilton Scale. This small increment is clinically insignificant, and likely accounted for by medication side effects strategically employed (sedation or activation).
When active placebos were used, the Cochrane database found that differences between drugs and placebos disappeared, given credence to the assertion that inert placebos inflate perceived drug effects.
The finding of tremendous placebo effect in the treatment groups was also echoed in two different meta-analyses by Khan et al who found a 10% difference between placebo and antidepressant efficacy, and comparable suicide rates. The most recent trial examining the role of “expectancy” or belief in antidepressant effect, found that patients lost their perceived benefit if they believed that they might be getting a sugar pill even if they were continued on their formerly effective treatment dose of Prozac.
The largest, non-industry funded study, costing the public $35 million dollars, followed 4000 patients treated with Celexa (not blinded, so they knew what they were getting), and found that half of them improved at 8 weeks. Those that didn’t were switched to Wellbutrin, Effexor, or Zoloft OR “augmented” with Buspar or Wellbutrin.
Guess what? It didn’t matter what was done, because they remitted at the same unimpressive rate of 18-30% regardless with only 3% of patients in remission at 12 months.
How could it be that medications like Wellbutrin, which purportedly primarily disrupt dopamine signaling, and medications like Stablon which theoretically enhances the reuptake of serotonin, both work to resolve this underlying imbalance? Why would thyroid, benzodiazepines, beta blockers, and opiates also “work”? And what does depression have in common with panic disorder, phobias, OCD, eating disorders, and social anxiety that all of these diagnoses would warrant the same exact chemical fix?
Alternative options
As a holistic clinician, one of my bigger pet peeves is the use of amino acids and other nutraceuticals with “serotonin-boosting” claims. These integrative practitioners have taken a page from the allopathic playbook and are seeking to copy-cat what they perceive antidepressants to be doing.
The foundational “data” for the modern serotonin theory of mood utilizes tryptophan depletion methods which involve feeding volunteers amino acid mixtures without tryptophan and are rife with complicated interpretations.
Simply put, there has never been a study that demonstrates that this intervention causes mood changes in any patients who have not been treated with antidepressants.
In an important paper entitled Mechanism of acute tryptophan depletion: Is it only serotonin?, van Donkelaar et al caution clinicians and researchers about the interpretation of tryptophan research. They clarify that there are many potential effects of this methodology, stating:
In general, several findings support the fact that depression may not be caused solely by an abnormality of 5-HT function, but more likely by a dysfunction of other systems or brain regions modulated by 5-HT or interacting with its dietary precursor. Similarly, the ATD method does not seem to challenge the 5-HT system per se, but rather triggers 5HT-mediated adverse events.
So if we cannot confirm the role of serotonin in mood and we have good reason to believe that antidepressant effect is largely based on belief, then why are we trying to “boost serotonin”?
Causing imbalances
All you have to do is spend a few minutes on http://survivingantidepressants.org/ or http://beyondmeds.com/ to appreciate that we have created a monster. Millions of men, women, and children the world over are suffering, without clinical guidance (because this is NOT a part of medical training) to discontinue psychiatric meds. I have been humbled, as a clinician who seeks to help these patients, by what these medications are capable of. Psychotropic withdrawal can make alcohol and heroin detox look like a breeze.
An important analysis by the former director of the NIMH makes claims that antidepressants “create perturbations in neurotransmitter functions” causing the body to compensate through a series of adaptations which occur after “chronic administration” leading to brains that function, after a few weeks, in a way that is “qualitatively as well as quantitatively different from the normal state.”
Changes in beta-adrenergic receptor density, serotonin autoreceptor sensitivity, and serotonin turnover all struggle to compensate for the assault of the medication.
Andrews, et al., calls this “oppositional tolerance,” and demonstrate through a careful meta-analysis of 46 studies demonstrating that patient’s risk of relapse is directly proportionate to how “perturbing” the medication is, and is always higher than placebo (44.6% vs 24.7%). They challenge the notion that findings of decreased relapse on continued medication represent anything other than drug-induced response to discontinuation of a substance to which the body has developed tolerance. They go a step further to add:
“For instance, in naturalistic studies, unmedicated patients have much shorter episodes, and better long-term prospects, than medicated patients. Several of these studies have found that the average duration of an untreated episode of major depression is 12–13 weeks.”
Harvard researchers also concluded that at least fifty percent of drug-withdrawn patients relapsed within 14 months. In fact:
“Long-term antidepressant use may be depressogenic . . . it is possible that antidepressant agents modify the hardwiring of neuronal synapses (which) not only render antidepressants ineffective but also induce a resident, refractory depressive state.”
So, when your doctor says, “You see, look how sick you are, you shouldn’t have stopped that medication,” you should know that the data suggests that your symptoms are withdrawal, not relapse.
Longitudinal studies demonstrate poor functional outcomes for those treated with 60% of patients still meeting diagnostic criteria at one year (despite transient improvement within the first 3 months). When baseline severity is controlled for, two prospective studies support a worse outcome in those prescribed medication:
One in which the never-medicated group experienced a 62% improvement by six months, whereas the drug-treated patients experienced only a 33% reduction in symptoms, and another WHO study of depressed patients in 15 cities which found that, at the end of one year, those who weren’t exposed to psychotropic medications enjoyed much better “general health”; that their depressive symptoms were much milder”; and that they were less likely to still be “mentally ill.”
I’m not done yet. In a retrospective 10-year study in the Netherlands, 76% of those with unmedicated depression recovered without relapse relative to 50% of those treated.
Unlike the mess of contradictory studies around short-term effects, there are no comparable studies that show a better outcome in those prescribed antidepressants long term.
First Do No Harm
So, we have a half-baked theory in a vacuum of science that that pharmaceutical industry raced to fill. We have the illusion of short-term efficacy and assumptions about long-term safety. But are these medications actually killing people?
The answer is yes.
Unequivocally, antidepressants cause suicidal and homicidal behavior. The Russian Roulette of patients vulnerable to these “side effects” is only beginning to be elucidated and may have something to do with genetic variants around metabolism of these chemicals. Dr. David Healy has worked tirelessly to expose the data that implicates antidepressants in suicidality and violence, maintaining a database for reporting, writing, and lecturing about cases of medication-induced death that could make your soul wince.
What about our most vulnerable?
I have countless patients in my practice who report new onset of suicidal ideation within weeks of starting an antidepressant. In a population where there are only 2 randomized trials, I have grave concerns about postpartum women who are treated with antidepressants before more benign and effective interventions such as dietary modification and thyroid treatment. Hold your heart as you read through these reports of women who took their own and their childrens’ lives while treated with medications.
Then there is the use of these medications in children as young as 2 years old. How did we ever get the idea that this was a safe and effective treatment for this demographic? Look no further than data like Study 329, which cost Glaxo Smith Klein 3 billion dollars for their efforts to promote antidepressants to children. These efforts required ghost-written and manipulated data that suppressed a signal of suicidality, falsely represented Paxil as outperforming placebo, and contributes to an irrepressible mountain of harm done to our children by the field of psychiatry.
RIP Monoamine Theory
As Moncrieff and Cohen so succinctly state:
“Our analysis indicates that there are no specific antidepressant drugs, that most of the short-term effects of antidepressants are shared by many other drugs, and that long-term drug treatment with antidepressants or any other drugs has not been shown to lead to long-term elevation of mood. We suggest that the term “antidepressant” should be abandoned.”
So, where do we turn?
The field of psychoneuroimmunology dominates the research as an iconic example of how medicine must surpass its own simplistic boundaries if we are going to begin to chip away at the some 50% of Americans who will struggle with mood symptoms, 11% of whom will be medicated for it.
There are times in our evolution as a cultural species when we need to unlearn what we think we know. We have to move out of the comfort of certainty and into the freeing light of uncertainty. It is from this space of acknowledged unknowing that we can truly grow. From my vantage point, this growth will encompass a sense of wonder – both a curiosity about what symptoms of mental illness may be telling us about our physiology and spirit, as well as a sense of humbled awe at all that we do not yet have the tools to appreciate. For this reason, honoring our co-evolution with the natural world, and sending the body a signal of safety through movement, diet, meditation, and environmental detoxification represents our most primal and most powerful tool for healing.












The manufacturers have been very successful at medically marketing these products (even though they are useless) so I suppose they’ll carry on at least while the money is in it. It’s amazing how they do it.
Report comment
Serotonin poses definitely some serious problems for one’s health but what remains unacknowledged by the alternative health community is that trytophan supplements are similarly problematic because the intake of this natural product is linked to many of the adverse effects of serotonin such as o brain dysfunction, stress hormone release, inflammation, impaired blood circulation in the brain, cancer, and so on – see: http://www.supplements-and-health.com/tryptophan-side-effects.html
Report comment
(Thank you for this excellent and informative article)
Report comment
Hi Kelly Brogan MD, A simple paradigm works for me. Allostatic overload (Bruce McEwen, neuroscientist) effects epigenesis For me, ‘mental illness’ is a description, a maddening metaphor, a pejorative psychiatric label for the stresses and strains in my life beginning at conception (allostatic overload) that I reacted to unconsciously, and was given a descriptions of that lived madness, by a ‘professional’, a diagnosis. To continue to call me ‘mentally ill’ is to insult me and be obtuse, ignorant of the facts of my life. Thank goodness I was given a simple, yes, holistic solution-Mind (affirmations), Body (whole food plant based nutrition, and Breath, Spirit (aerobic exercise). Who knew?! Not traditional psychiatry, traditional medicine, and traditional religion. I am well from the description, ‘ocd’, chronic, severe. I got off psychotropic medications and had No symptoms of the description within 6 months of starting that simple mirepoix. Also I no longer have prediabetes, high cholesterol, high blood pressure and have lost over 80 pounds. There are better paradigms than management and control of a description with psychotropic drugs which have potential harmful side effects as listed in the PDR and ECT, even animals avoid electric fences, much less put their heads on a pulsing electric wire. However, Voltaire remarked, Common sense is not so common. For me the simple is profound, however in being profound that does confound most. Happy New Year Dr. Brogan, great article! Kurt E. Wilkens
Report comment
Thank you for speaking the truth, Kelly. As a person who had the fairly common withdrawal effects of the “safe smoking cessation med,” Wellbutrin, misdiagnosed as “bipolar.” And a person who found dealing with psychiatric practitioners completely insane, due to their delusions about the adverse effects of the psychotropic drugs. I’m very grateful the truth is starting to emerge. Thank you.
Report comment
I wonder why the psychiatrists and drug companies never consider that people may be depressed as a result of being told (by psychiatrists, social workers, case managers and other) that they will need to be on these drugs for life, be considered an incompetent, have a high likelihood of going to prison, being homeless, will find great difficulty finding a job, and oh yes – have people in government and others wanting to hunt you down, force medication on you, and be a scapegoat for all the problems in society. Now why aren’t you happy that ‘we are going to take care of you’?
Report comment
Good comment, mhadvocate. And thank you for this article, Dr. Brogan.
Report comment
Divide, (defame,) and conquer was psychiatry’s goal during WWII, and they’re still seemingly playing the same game. Will they ever learn that defaming people with fititious “mental illnesses,” torturing, and killing other human beings is inappropriate and unethical behavior?
Report comment
People are not depressed because their shrink tells them they are. If you have major depressive episodes you know it. Balderdash.
Report comment
You didn’t read the rest of the post from mhadvocate. This was not the point at all of what was written.
Report comment
As a Doctor (D.Sc, not M.D.) it really bothered me when reading the info for Zoloft, Effector etc. basically the pharma company comes out and says “Hey, we have no clue how this drug works, just trust us that it does.” And of course they always suggest combining it with talk therapy.
Like the author I always wondered just what is an optimal brain state and why don’t they measure my blood to figure out just how low I am when it comes to the chemical balance.
I’m not really sure where I stand on this issue, I do know that I feel and function better on the drugs, but do the drugs really help? i guess that is the question.
Oh and I LOVE the author for pointing out all the Meta-Analysis research!!!! That’s what my dissertation was all about!
Report comment
I’M SHOCKED that the writer of this article failed to mention that ALMOST EVERY SCHOOL SHOOTING in the country in the last TWENTY years involved a teenager with a prescription for anti depressants. From Columbine to Newton, either they were in withdrawal, or in a state of chemical psychosis and mania induced by SRI drugs.
Look it up.
Report comment
Thanks a bunch for reminding us of this sad truth that tragically never gets reported in the main street media.
Anthony
http://www.wholelifehypnosis.com
Report comment
It’s ironic that I should read this article and find this site just after having an experience with my doctor that left me feeling humiliated and bereft of trust. Every morning I sit and look at the handful of medications that has accumulated over the years as I have aged; and every morning there is a feeling in my “gut” that I should not be taking all this stuff. I have suffered depression since I was very young; and I’m quite old now. I’ve been on these antidepressants since they came on the market. Now you have me questioning. I hate being misled and frankly, I feel our medical system has reached a point where it is no longer at all concerned with “me” as an individual, nor has it been for sometime. I am a lab rat, who earns them a tremendous amount of profit every year. I am ready to bust out of my cage. I already had planned to start searching today for alternatives. Like I said, ironic. Thank you for one the most intelligently written and informative articles I have read in a long time.
Report comment
Hello and thanks for this wonderful article. My history with shrinkage spanned over three decades but I wasn’t often given antidepressants. I was only truly suicidal three times in all those years. The first time was right after I started Imipramine, age 26. The second was the consequence of far too many shock treatments. The third time was in 2011 and I was again given Imipramine. I had terrible side effects including the “black box warning” feeling like I was jumping out of my skin. I also had high blood pressure, racing pulse, and enlarged breasts due to prolactin increase. I reported all this to my shrink who said “Don’t worry about it.” After a number of months I was in a hospital (of course) and asked the NP to please take me off Imipramine. She took me entirely off in three days and then I was released. Oops. That was 2012. Thankfully I am alive. I am off all meds after being on as many as seven or eight simultaneously over the years. I am amazed at how well I am doing now that I am out of MH’s clutches. Physically I am so much better and emotionally much happier. I am thrilled to be starting life over. May we all have that second chance we deserve. Go grab that chance ASAP.
Report comment
This is excellent. Well done. Unfortunately, it doesn’t go quite far enough in question commonly held assumptions. Of course it is true that Big Pharma lies, that psychiatry coerces and oppresses, and that pscyhotropic drugs cause irreparable harm and often death. But we need to go a step further. Where do all of our notions about “mental illness” actually come from? How can we even talk about “root causes” of “mental illness” when the whole concept of “mental illness” is based on lies to begin with? It is well that we research and write about all of the 21st century studies, but in order to understand the myth of mental illness we need to go back further in time. We need to ask ourselves how a society could produce a Kraeplin, a Freud, and eventually a Hitler. If we haven’t read the works of Thomas Szasz, Laing, or Foucault; if we have not yet read Robert Whitaker’s books Mad in America and Anatomy of an Epidemic; if we haven’t confronted the age old question “What is mental illness?” then I’m afraid that we have only begun to scratch the surface of the problem that is before us. Again, great article. I applaud these efforts, and am grateful for such contributions. Slay the Dragon of Psychiatry.
Report comment
Depression is an awful disease and there is no one size fits all, but I do know the times when my spouse has tried to ween himself off medication or messed with the doses he has ended up in the hospital. I believe the homeopathic approach may work for some, but for others, anti-depressants, ECT treatment, etc. are literally life savers. I think it’s difficult for anyone to pass judgement unless you have seen it or lived it first hand and adding to the stigma of mental illness is learning to accept that some people need different, more or less treatment then others. Acceptance is key.
Report comment
BAA, you are very correct on this point. Not all leopards have the same spots. Perhaps they are only dealing with people with mild mood disorders. “Oh boy I am bummed today the mail is late”. But if you actually need the medication they are life savers. This disease runs in my family and no amount of exercise, fresh air, meditation and organic food is going to cure it. They are good but not a cure for the cause.
Report comment
BAA and HappyHounde
If you want to take the toxic drugs and if you want to believe that they help you that’s your choice. However, I myself do not need any of the myriads of real scientific studies that prove these toxic drugs to be extremely dangerous to know that they are harmful. I almost lost my life to the damned things. I’m lucky to be alive and here today.
So-called “depression” is not a disease but a normal human response to difficulties in life. Psychiatry and the drug companies have convinced the world that it’s a disease so that they can sell their respective products to the rest of us. The chemical imbalance idea is now being debunked even by many biopsychiatrists who once supported it vehemently. Society needs to wake up and smell the coffee and find out how we’ve all been duped on a massive scale merely for the financial gain of psychiatrists and the drug companies.
Report comment
BAA,
As an FYI, if you taper too quickly off of psych meds which could have been what happened to your husband, you will suffer rebound symptoms that look like a return of the condition but aren’t. Next time he decides to go off of his meds, he might want to visit http://survivingantidepressants.org/index.php?/index. It is a support site and helps people slowly get off of the meds at around 10% of current dose every 4 to 6 weeks. The site is supported by financial contributions and is not dependent on any commercial outfit.
Report comment
Dr. Kelly, You are very young and yet to have too much experience with patients. Believe me if you need medication you need it. Period. Holistic is just another form of medication. Whether it be of plant or animal origin. If you have major depressive episodes they do not just go away by food, exercise, organic food and talk therapy. Until a real answer to the cause can be discovered it is the difference between being able to function and not function. If you ever have the misfortune of having a major depressive disorder you will know that you are living in hell. It is NOT just a mood it is physical. It does not go away after 10-12 weeks. I am speaking from experience and am a level headed no nonsense person.
Report comment
I actually have the diagnosis of schizophrenia, bipolar and severe depression. I don’t really agree with prognosis and whatever you have. I’m not using any drugs, such as neuroleptics, etc. It’s possible for some people to live without the drugs… for some the drugs help. It’s OK if some people like to take the drugs. I just take the issue when some idiots or assholes come and try to force the drug to me.
Report comment
Thank you. Your article explains what I’ve seen with my patients for over 30 years that depression is more a marketing term than a medical or psychological term.
Every “depressed” patient I’ve seen was chronically fatigued. When the body released it’s chronic stress and exhaustion, the depression would magically leave.
Report comment
Hello, i think and hope you are right but how to release all this stuff from the body??
Report comment
This article is simply wrong. I’ve had panic episodes since I was 10 nor 12 years old. Some people call it depression, anxiety, panic whatever you call it, it is real. Zoloft saved my life. I am 55 years old and tried everything. Hiking, exercise, Diet, meditation etc. The only thing that made it so that I didn’t crawl back into my shell of anxiety was Zoloft. I’ve taken it for over 15 years with NO side effects. Don’t present it like it is bad or doesn’t work. You do an extreme injustice to people who would seriously benefit from an S.S.R.I. They don’t need to be filled with more confusion over a choice they need to make and you don’t understand
Report comment
I had severe panic attacks when I was young, etc. I got diagnosed with schizophrenia, bipolar, etc, in my thirties. I had been on SSRI on and off for a long time. Actually, what I really feel bad about is the use of neuroleptic drugs. The prescription that you mention was actually almost exactly what worked for me. Hiking, exercise, diet, meditation. The really worked for me, in combination, but it may not work for everyone. SSRI may work for some people, for some time, who denies that?
Report comment
I understand completely emotional/Mental illness sucks because people don’t take it serious if you have diabetes people are ok with your medication. If you have depression people think you can think good thoughts or weird stuff like that. Zoloft is a real medicine that really works and it’s too bad it is not understood by even professionals like the lady that wrote this article.
Report comment
I think there’s nothing wrong as such in taking Zoloft, etc. Taking it may be useful for you. At the same time, I think it’s amazing how much your body and experience of life can change through proper practice, etc.
Report comment
@Bossco, none of what you have described actually proves the Zoloft is effective due to its chemical properties. It’s just as likely that the Zoloft is effective because you expect that it will be effective (placebo response.) Obviously I can’t prove that, either, but I think it’s a possibility you should consider. I mean, how great would that be to discover you didn’t even need to be taking the Zoloft?
For about a decade I was just as convinced as you that “antidepressants” saved my life. I was equally convinced that I needed to take a benzodiazepine to cure me of anxiety. But eventually I learned that wasn’t true, and now it seems very much like it was my belief that the drugs would work that made them seem to work. Getting off the benzo actually reduced my anxiety level dramatically, and now that I’m halfway off my “antidepressants” and still doing great I am persuaded that I don’t need those either.
Now, exercise and talking openly with people about what’s going on in my life have become my real antidepressants. Maybe that’s just because I expect them to have that effect, but hey, at least they have positive rather than negative sideeffects 🙂
Report comment
The recent comments remind me of the kinds of things I was saying 20 years ago, even five or ten years ago. I was so sold on the brain disease theory. I defended it endlessly even to my parents, who were naturally worried and had no clue about any “brain disease.” They ended up joining a NAMI support group. My dad was president of the Massachusetts chapter of NAMI. In 2012 a friend of mine suggested that there was no brain disease. I got very defensive. How dare she? This is what had “worked” for me for decades. Hadn’t these medications saved my life?
But…what life? I’d spent a good deal of it in and out of hospitals. My chances of getting anywhere at the rate I was going were next to nil. In, out, in, out…Why? I looked around me. I was in eating disorders care and on roughly four or five medications at that point, or shall I say, down to four or five. I was sitting in the dining room hoping I could get away with not eating, even though I was starved. I saw the faces of the other patients. These were those who had no voice. They’d been silenced, censored, and now, were locked up in this facility just like I was. Truth was, we were all starving people. Starved kids, starved men and women. We were all now forced into slavery at this place. At that very moment, a light bulb went on in my head. I promised myself I would make a change, a dent in the world, and I wouldn’t allow myself to be silenced anymore. That’s when I picked up a morself of food, put it in my mouth, and because of this, lived.
Once you realize the fallacy, you can’t go back, and you won’t. Walking out was the toughest thing I ever did. It was a wildly unpopular move. I lost many friends, especially those still in “treatment.” I even got threatened by my shrink. She became my ex-shrink and I vowed I’d never see another.
Of course I was depressed. I tried suicide three times. That doesn’t count the times I nearly died of starvation. I am not trying to boast, only to say that my life was certainly similar to those that state that depression was disabling. It is, undoubtedly.
My kidneys are nearly destroyed from meds. They’re half the size they should be. My thyroid is totally gone. But now, sans “diagnosis,” which I simply ditched, my life is much, much improved!
Know something? My dad would be mighty proud of me right now. I would wish the same for anyone.
Report comment
Hello Dr.Brogan,
As a clinical neuroscientist,teacher of neuroimmunology,a practitioner CAM, practicing psychiatrist and having worked on modeling of major depression, your piece struck my curiosity.
It is true all that you write.It is equally true that it is as flawed because of its conceptual simplicity.
And I find it vacuous and destructive since it is written in a pseudoscince “down to earth”style.
Where is the science to support your “holistic” approach? What does that even mean? Have you yourself done a study on “your method” that could be scrutinized by the scientific community? Have you published your “countless patients” who became suicidal from medication? Do you have a theory that can separate worsening symptoms from medications from worsening of the illness?
Since many myths that needed to be destroyed,fortunately are,were or will be,your column leaves nothing to replace them but hyperbole and vitriol.For the perhaps 4 people in the world whose life have been saved by these medications, you have now possible planted the seed for maybe one of them to stop them.I hope there is no negative repercussion for your tacit encouragement for them to do so.
In summary,you attack everything and leave not a shred of scientific data,theory or evidence to replace what truly needed to be replace.Run and eat well and meditate?And the scientific basis of that helping …….everyone?A hyperbolic ,vapid piece that sadly will be taken to heart by those who do not realize you provide nothing better-based upon science.Only hyperbole.
Report comment
How many people you helped of to get off these meds ultimately curing the cause of their states.
Report comment
Dr Brogan,
Than you for being part of MIA, and for your wonderful video, ‘From Gut to Brain, and Back Again’ –
https://www.youtube.com/watch?v=pKKG869s8oo&list=UUrd5zW6kiV52XuvOvIeYrEQ
This should be seen by all psychiatrists.
Duane
Report comment
theloniusmonk: You wrote, “It is true all that you write.” Presumably that means you do not dispute Dr. Brogan’s thesis that the chemical serotonin imbalance story of depression is a myth, that the efficacy of antidepressants over placebo is minimal and grossly exaggerated in the published literature, and that these drugs produce well-documented adverse effects that have been systematically suppressed by the pharmaceutical industry and medical community. As a clinical neuroscientist, teacher, and practicing psychiatrist, I would have though these revelations would be of principal concern to you. However, after “pulling rank” as an expert on the topic, you ignored the science she cited and it’s implications for the credibility of psychiatry and its bread and butter theory and treatment for 20+ years, and instead attacked her for observations that are largely tangential to the primary message of her blog. It also seems you are offended by Dr. Brogan’s tone, and that she has not offered an adequately valid alternative approach to replace the myth she debunks.
Those who debunk myths are not obligated to offer valid alternatives to them. Neither are myth debunkers obliged to adopt a deferential tone when debunking myths that have caused direct harm to so many. What you call vapid and vitriol and hyperbole, other people familiar with the science and/or lived experience of antidepressants call astute and long overdue critical analysis.
You wrote, “Do you have a theory that can separate worsening symptoms from medications from worsening of the illness?” Such a question from a self-proclaimed expert like yourself is cause for serious concern. The answer to your question is well-known to the scientific community and should be to you as well.
Antidepressant-induced suicide is a valid phenomenon. Significantly more suicide attempts occur in patients randomized to antidepressants than placebo in clinical trials. This conclusion is the basis for the FDA black box warning. There are bloggers on this site who have lost their children to antidepressant-induced suicide, in circumstances where the prescriber failed to inform the family that the antidepressant increases suicide risk. I wouldn’t expect them to be overly concerned with the “tone” of those who would expose the antidepressant myths discussed by Dr. Brogan. Let’s not lose sight of what matters most in this discussion: the facts.
Report comment
Academic,
Thank you, I agree with your assessment of the loniusmonk’s attack on Kelly’s blog. And loniusmonk’s, I’m your perfect example “that can separate worsening symptoms from medications from worsening of the illness.” I had the adverse withdrawal symptoms of an antidepressant (given for smoking cessation, not depression) misdiagnosed as “bipolar.” Or do you, as my former doctors believed, think a desire to quit smoking is the etiology of bipolar? The antidepressants are known (it’s on the black box warning now) to cause the bipolar “mania” symptom – even in people with no prior mental health issues.
Report comment
“long overdue critical analysis.”
Simply not the case. The chemical imbalance hypothesis has now been formally challenged and criticized plenty of times. In fact if you just look through the archives of the MadinAmerica echo-chamber, I’m sure you’ll see plenty of articles that mirror this one to some degree.
Nothing new here. More mischaracterizing the the scientific community’s current thinking on the chemical imbalance hypothesis, similar to how drug companies mischaracterize, but to a different end.
Report comment
You are correct, the chemical imbalance hypothesis absolutely has been formally challenged and criticized – but almost entirely by people outside mainstream psychiatry, like the folks at MIA. Psychiatry at the highest level (APA, KOLs) has remained “above the fray,” choosing to ignore the issue or, alternatively, pretend that the hypothesizes is antiquated and was never taken seriously by thoughtful psychiatrists. The fact that the explanation of psychopathology that dominated psychiatric practice for decades is not valid, and never was, seems of little to no concern to organized psychiatry, NAMI, and others who peddled this myth. Nothing new here? Are you serious? Imagine you gathered a group of patients who have been prescribed antidepressants by a psychiatrists. If you informed them that the chemical imbalance hypothesis is not valid, and never has been, do you think the response would be disinterest? The chemical imbalance story is a major reason why people took the drugs. This story also causes people to expect their symptoms to be chronic, outside of their own control, and necessitating drugs for the long haul. If you actually care about this issue, I recommend you read MIA posts by Phil Hickey, and Jonathan Leo and Jeff Lacasse, on the chemical imbalance myth and psychiatry’s pathetic attempts to rewrite its shameful history in embracing it.
Report comment
The SSRI Medical/Pharmaceutical Fraud is probably the biggest money making scheme of all time. I think it’s days are actually numbered.
And it’s good to see it being scientifically exposed by proper doctors and professionals.
Report comment
Thanks, Academic, for making some great points about the chemical imbalance hypothesis/theory. I appreciate that calling it a theory or hypothesis gives it too much credit. Better to describe it as the
chemical imbalance STORY
and the
chemical imbalance MYTH.
I also appreciate those who dub it the
chemical imbalance FRAUD
and the
chemical imbalance LIE.
Report comment
And it is a “story,” “myth,” “fraud,” and “lie” that was told to many, which would imply the millions of us fed this lie have a right to justice for the malpractice based upon this lie. Since, no offense intended, WTF does the psychiatric industry believe is the purpose of malpractice insurance, if not to properly compensate those of us who’ve dealt with their malfeasence?
Report comment
A noble lie?
http://en.wikipedia.org/wiki/Noble_lie
And the mushrooms are still buying it.
Report comment
Those of you extolling the virtues of SSRIs, can you provide links that aren’t supported by pharmacy that prove these work long term?
By the way, I am not anti meds even though I feel taking psych meds was the one of the biggest mistakes of my life. I have taken sleep meds on a PRN basis. But as far as I know, there isn’t any evidence that says they work long term and I have to keep that in mind.
Report comment
Helpful article, thank you. Posted on our service blog (Exeter UK): http://palacegatecounsellingservice.wordpress.com/2015/01/01/depression-its-not-your-serotonin-kelly-brogan/
Report comment
“The Science of Psychiatry is Myth”
Here are some other myths to consider:
http://www.huffingtonpost.com/nada-logan-stotland-md-mph/psychiatry-myths-and-myst_b_840852.html
Report comment
Oh my. Thanks for the link to the blog on “Myths About Psychiatry.” This Stotland character really knows how pile on the hogwash, doesn’t she? E.g., she claims that brain scans can detect depression?! Yeah, right! And people treated for so-called schizophrenia can have “fulfilling lives” thanks to psychiatric drugs that she claims “unclutters their brains.” ha ha ha ha ha ha And – this one’s the most hilarious – prejudice against psychiatry goes back thousands of years!! Oh my goodness. What a load of crap.
That Stotland is a former president of the American Psychiatric Association speaks volumes about how intellectually bankrupt THAT group must be.
Report comment
Is there NO room for Christian Theology at MIA?
I have come to observe that the overwhelming majority of topics or postings here at MIA almost invariably revolve around one thing and one thing only. That is, the verifiability (and/or abuses) of a naturalistic-mechanistic based empirical science of “mind as brain” (outputs) and/or its naturalistic-environmental stimuli (inputs).
Accordingly, whatever medical-natural scientists do (or do not) empirically know about the brain, and/or its natural-physical environment, is thee fundamental basis for either treatment or non-treatment. At a core level it seems that there is absolutely no room whatsoever for the biblical-theological concepts of “soul” or “spirit” to inform anything substantial in our metaphysical understanding of human nature, madness, suffering and “healing of the soul” (i.e. as the true “psychiatry”) here at MIA. And any actual use of the word “spirit” or “soul” is simply relegated to a kind of metaphorical-linguistic (or a pseudo-spiritual or poetical-emotional) expression. Thus, there seems to be nothing else permitted into this sacred-closed MIA universe of materialistic cause and effect relations; as though it was simply axiomatic that there was no real “spirit” (or “ghost”) in the machine. And so, why bother!
As a Christian theologian it totally amazes me how approximately 80% of Americans can be professing Christian theists and yet at the very same time the epistemological center of gravity here at MIA always seems to revolve around the creeds of philosophical naturalism and the hymnbook of “evidenced based medicine”. In other words, the empirical-demonstrable facts (or absence or abuses thereof) reign supreme in virtually every topic or posting . These MIA devotees of rational-empirical science are constantly bowing down, with utmost deference, before the altar of logical positivism as if it were the only verifiable path to the purest scientia (knowledge). This evangelistic devotion at MIA to the creeds of scientism is nothing short of religious in its zeal.
However, or notwithstanding the perpetual offerings to the religion of materialistic naturalism at MIA, I would like to gentle (and loving) remind all professing Christians at MIA that the one and only and true epistemological foundation for the first principles of human nature (or the true foundations of psychology – as the study of the SOUL) are the Oracles of the Most High God. That is, the eternal Word of God “theópneustos” (“God-breathed”) into written form, through holy prophets and holy apostles, is the purest of “scientia” (knowledge): “The words of the LORD are pure words: as silver tried in a furnace of earth, purified seven times.” (Psalm 12:6)
Hence, for Christians there are essentially two ways in which the “facts” of life and reality can be discovered: 1.The facts discovered “by” us (i.e. rationalism-empiricism) and 2. The facts discovered “to” us (i.e. divine revelation). However, the facts of life and reality (e.g. the facts of human nature, madness, suffering and healing of the soul) discovered-revealed “to” us are infinitely more foundational (not to mention infinitely more encompassing and insightful) than the facts discovered “by” us. And so, let us engage the “facts”.
This is not to say that there is not a wonderful place for human reason and empirical methodology, when it comes to understanding human nature, madness, suffering and “healing of the soul” (i.e. as the true “psychiatry”), and which was, in part, demonstrated in this article by Dr. Brogan, but it must always play (i.e. for Christians) a supporting or subservient role as a “handmaiden” to Theology; as the “Queen of the Sciences”.
And so, or once again, to all the Christians here at MIA, I ask a gentle (or rhetorical) and hopefully encouraging question; a question to which I hope will stimulate some of our future discussions toward some of the larger biblical-theological concepts of “soul”, “spirit”, “heart” and “mind” etc. in “spiritual illness” (and NOT the erroneous teaching of “mental illness”) and “spiritual health” (and NOT the erroneous teaching of “mental health”):
With respect to human nature, madness, suffering and the “healing of the soul” (lit.”psuche/hiatria” or the true “psychiatry”), why would you ever start by walking or wandering in the dark (i.e. with hypothesis, theories, experimentation, etc.) when you can start by walking in the Light (i.e. with the “facts” of human nature, madness, suffering and healing of the soul discovered-revealed “to” us in the Sacred Christian Scriptures)?
Reverend Haynes
Report comment
MIA has INDEED published a Christian theologian, Elahe Hessamfar, who states “we certainly don’t suffer from a lack of medical treatment for [“those whose spirits are broken”] . . . In fact, if anything, we suffer from overmedication, and hurful treatments that may damage a person’s ability to make right and wrong decisions.”
Here’s a link:
http://www.madinamerica.com/2013/10/mental-illness-right-wrong-drugs-violence/
Reverend Haynes, I encourage you to submit your own article to Mad In America. I, for one, would love to hear more about your perspective on what role the church might have in healing those with broken spirits (aside from providing free meeting space for NAMI initiatives, of course).
Report comment
With all respect Reverend, the Christian groups that I’ve been part of are no more skeptical of “science” than the commentators on MIA. Most of their members are fully supportive of getting forced chemical “help” for relatives in old folks homes or children sitting submissively in the pews beside them. The belief in the holy spirit has become a private matter in today’s world, I think.
The churches should be leading the fight against psychiatry’s minimizing of the spiritual aspects of our lives, aspects such as purpose, morality, faith in life, and courage in death. The only church that seems even sporadically to do much in the way of objection to psychiatry is the Unitarian Church, a church so far from its Christian roots as to be almost universalist.
Personally, I would chose Scientology as a last resort for help today. In practical terms they represent the only group likely to offer any protection from the mental health system as it actually operates.
You can appeal to Christians in the abstract all you wish, but, when the only church willing to fight this Satan Psychiatry is that of Scientology, I believe you Christian people have some changing of your own to do.
Report comment
Anothervoice I agree with you. And I am a Christian psychiatric survivor. A lot of Christians reject science’s idea of how life started. Why can’t they reject psychiatry? Social Darwinism is at the root of it, along with a materialistic world view.
The Book of Christianity, the Bible, says we are more than bodies and brains with biochemical reactions. We are indeed animals, but we are in the image of God, meaning we’re free moral agents. Psychiatry says we’re machines without souls, just chemical balances, or in our case imbalances.
I hope I’m not offending you atheists unnecessarily. I’m just saying I can no longer reconcile Christianity and psychiatry. How others do is beyond me.
Report comment
Its a question I’ve pondered deeply Rachel.
I think that there are those who begin with the belief that they can conquer evil with good, but who are gradually led astray and begin to try and fight evil with evil. This gradual regression is not obvious to those within the system, but patently apparent to anyone thrown into the hell that is forced psychiatry. God leads astray who He will.
regards. Boans
Report comment
Reverend,
the church has a strong history of condemning difference…and in most instances still does with things such as homosexuality, and the ordination of women.
It also has a brutal history as far as exorcisms and “treatment” of a wide range of what may now be called psychiatric illnesses, blaming people’s evil or flawed nature or their sins for their difficulties. For many, the church is not much safer than psychiatry, for others it has proved even more dangerous and/or has delivered them into the hands of psychiatric “treatment” after traumatic experiences.
Here in Australia we are having a Royal Commission into institutional child abuse, and the churches are among the leaders in denying justice to those harmed and protecting perpetrating priests, going so far as to ship them to distant parishes or even overseas to hide their actions.
I believe this site should remain blissfully free of and from religion, as, while you believe religion has a place in healing, it is not an evidence-based solution and has the potential to cause divisions in what is generally a harmonious and supportive site.
Anothervoice notes above that Scientology and the Unitarian Church are pretty much the only churches taking a stand against psychiatry. If all churches did the same, then maybe there would be a place for them on here…but in my mind even then it should only for their stance against psytchiatry, not to promulgate their doctrines or seek souls.
Report comment
Hi folks. Friendly reminder of our guidelines (http://www.madinamerica.com/posting-guidelines) which ask that conversations remain relevant to the blog posts. A discussion of Christian theology does not seem particularly on-topic here (although I can see how it might be a response to Kelly’s question “So, where do we turn?”). If people would like to discuss this topic further, I suggest starting a conversation in our forums:
http://www.madinamerica.com/forums/forum/community/
Report comment
sorry. please feel free to delete my post.
Report comment
I think what you wrote is okay to leave up, I was just hoping to forestall a big debate/derail… religion can be such a hot-button issue.
Report comment
Reverend,
I agree a big flaw in psychiatric thinking is that it is a completely materialist viewpoint, solely left brain. Of course, intuitive Spirit guided inspiration is imperative for a true understanding of any subject matter. And, of course, when a specialty of science denies the existence of the Holy Spirit, as I have proof right in my medical records that a supposedly Christian psychologist did, well, denial of the Holy Spirit is the “only unforgivable sin” in the entire Holy Bible. So of course that industry will go off on a futile “mindless,” “soulless” quest, as it is now evident the psychiatric industry has once again done.
I do agree with others above that the mainstream religions should be actively working to discredit the fraud that is psychiatry today, but they are not. And it was confessed to me, and I have medical evidence of this issue, that the reason they are not is that historically, and still today, the psychiatric industry has been in the business of covering up sexual abuse of children for the mainstream religions. An ethical pastor of mine described this as “the dirty little secret of the two original educated professions.”
And I know from personal experience the ELCA Lutheran church utilizes psychiatric defamation and poisonings to cover up and deny medical evidence of child abuse. I’ve also spoken with Catholics, and had to recommend Whitaker’s book, because the Catholics are still offering psychiatric treatment as the only compensation for clergy child abuse offenses (and the couple I spoke with was dealing with their “depressed” child being turned into a “bipolar,” via the antidepressants.)
As a pastor, I hope you will work to change the mainstream religion’s support of today’s psychiatric industry. I’m trying to educate pastors and bishops, but the mainstream religions seem quite adamit about maintaining their “dirty little secret” way of unjustly covering up their sins and crimes via psychiatric discrediting and tranquilization.
Report comment
My sincere thanks to everyone who commented on my (somewhat) polemical post! I truly appreciate all of your thoughts, encouragements, references, suggestions as well as criticisms!
Also, I hope my comments will engender some healthy discussion (even healthy debate), here and elsewhere, and thus expand on Dr. Brogan’s description of the scientific limitations regarding depression (or rather “the spirit of heaviness”) that would “encompass … a curiosity about what symptoms of mental illness may be telling us about our physiology and SPIRIT”. (Emphasis mine)
Dr. Brogan’s question “So, where do we turn?” is not only indicative of the miserable ignorance of a positivistic devotion to Natural Science but has clearly open the door to a broader-theological discussion beyond the long hoped for, long awaited “medical materialism” of the 20th century. It reminds me of St. Peter’s rhetorical question to Jesus: “Lord, to whom shall we go? You have the words of eternal life” (St. John 6:68).
And so in the “spirit” of St. Peter, my answer to Dr. Brogan’s legitimate question, regarding the mystery of so-called depression, was to simply ask another question: Is there NO place for Christian Theology at MIA?
When MIA is dealing with the “essence” of human nature (including the essence of the human “mind”), together with the vast range of severe mental-emotional suffering of human beings, how is it even possible for MIA to exclude a Christian Theology (specifically a Biblical Psychology) from the main discussion? And even more importantly, from the main objectives-agenda of MIA when approximately 80% of the American “general public” (over 200 million Americans) are professing Christians?
In other words, how can anyone truly perceive “religion” as a “derailment” or “hot-button”, which ought to be relegated to the “forum” (the sidelines) for discussion, when these critical issues are, in fact, the very heart and soul and substance of religion itself? I am puzzled! And it would seem that I am not alone:
“Socrates was, and wished to be, hiatros tes psuches, a healer of the soul. These Greek syllables have been recast to form the word ‘psychiatrist’. But Socrates would hardly recognize the medical psychiatrist as a member of his fraternity. A scientific psychiatry indifferent to religion and philosophy is a new and strange phenomena. Whatever may be the future importance of this new science, it is abundantly evident that the role of the religious physician of souls is not played out.” (John T. McNeill, “A History of the Cure of Souls”, 1951, p.8)
Reverend Haynes
Report comment
I don’t see having a forum discussion as one that takes place from the “sidelines.”
Any number of these blog posts could be a segue for a good talk about spirituality, religion, faith… I would enjoy the opportunity to read what others have to say; participate in the dialogue.
Unfortunately, we don’t have a forum for Spirituality:
http://www.madinamerica.com/forums/
Duane
Report comment
Dr. Brogan thank you so much for this fantastic article. I am writing from both personal & professional experience, and therefore I so appreciate your clarity & detail. As I read in your article, I often read about the need for an alternative or more holistic approach, but rarely do I read about the efficacious use of hypnosis. Medical doctors began using and experimenting with hypnosis since the 1840’s, but it’s “existence” has been around since the dawn of time. Why? Because it is simply a natural, normal human phenomenon that we experience probably 60 – 70% of our day. Anyway, I wish more doctors were courageously honest like you, about the chemical imbalance myth & the dangers of these so-called “anti-depressants”.
Throughout the historical use of people’s own mind (hypnosis), it has proved to be the safest and on of the most effective approaches to emotional & psychological struggles. We must remember that the client’s or patient’s genius mind that developed their skill (depression, anxiety, etc.) out of their awareness, is the same mind that can just as easily create something different & more useful.
Again, thank you so much Dr. Brogan. I’m hoping to connect with like-minded MD’s here in MN.
My 2 cents,
Anthony Verderame, MA
http://www.WholeLifeHypnosis.com
Report comment
“The chemical hypothesis of depression suggests that mood disorders are caused by a chemical imbalance in the brain, which can be corrected by antidepressant drugs. However, recent evidence indicates that problems in information processing within neural networks, rather than changes in chemical balance, might underlie depression, and that antidepressant drugs induce plastic changes in neuronal connectivity, which gradually lead to improvements in neuronal information processing and recovery of mood”
But the antidepressants are credited with generating plasticity in the neuronal pathways which leads to mood improvement. It is a chemically induced modification of the brain! BTW, the results suggest a different application may be involved.
Report comment
Blakeacake
Nothing I have been able to find in the way of verified long-term studies which would be needed to show such relationships or even comments from the APA or drug compainies suggest that what you are saying here has been validated.
If you have access to such material, could you please post links and/or refute the material quoted with scientific evidence.
Your anecdotal evidence and/or a new theory of “chemically induced modification of the brain” (which I note is generally called brain damage) that makes people happy through the long-term use of antidepressants, would tend to fly in the face of the results of the material to which Dr Brogan refers above.
The bullying, coercion, condescension and forced and/or long-term drugging frequently inflicted on “mentally ill” patients with a “chemical imbalance” by the medical profession has generally not worked for people accessing this site, many of whom tend to adopt a more humanistic and evidence-based approach.
Just because you say anti-depressants work, doesn’t make it true, Blakeacake, no matter how many patients you have “treated” or how attached you are to the idea that anti-depressants generate “plasticity in the neuronal pathwways which leads to mood improvement”.
Share the actual evidence, please.
Report comment
start here
PMID: 15738959 [PubMed – indexed for MEDLINE]
The chemical hypothesis of depression suggests that mood disorders are caused by a chemical imbalance in the brain, which can be corrected by antidepressant drugs. However, recent evidence indicates that problems in information processing within neural networks, rather than changes in chemical balance, might underlie depression, and that antidepressant drugs induce plastic changes in neuronal connectivity, which gradually lead to improvements in neuronal information processing and recovery of mood.
Have you read much of the research of E Castrén and his group? Pretty interesting dude.
Antidepressants protect against hippocampal volume loss in humans and reverse stress-induced atrophic changes in animals thus supporting the hypothesis that the pathophysiology of stress-related disorders such as depression involves reductions in neuronal connectivity and this effect is reversible by antidepressant treatment. However, it is unclear which brain areas demonstrate such alterations in plasticity in response to antidepressant treatment. The aim of the present study was to examine the effect of antidepressant treatment on the expression of three plasticity-associated marker proteins, the polysialylated form of nerve cell adhesion molecule (PSA-NCAM), phosphorylated cyclic-AMP response element binding protein (pCREB) and growth-associated protein 43 (GAP-43), in the rat brain. To this end, rats were treated either acutely (60 min) or chronically (21 days) with imipramine (30 and 15 mg/kg, respectively) and the expression of PSA-NCAM, pCREB, and GAP-43 was assessed using immunohistochemistry. Initial mapping revealed that chronic imipramine treatment increased expression of these plasticity-associated proteins in the hippocampus, medial prefrontal cortex and piriform cortex but not in the other brain regions examined. Since PSA-NCAM and pCREB are expressed in recently-generated neurons in the dentate gyrus, it is likely that chronic imipramine treatment increased their expression in the hippocampus at least partially by increasing neurogenesis. In contrast, since chronic imipramine treatment is not associated with neurogenesis in the medial prefrontal cortex, increased expression of PSA-NCAM and pCREB in the prelimbic cortex implicates changes in synaptic connectivity in this brain region. Acute treatment with imipramine increased the number of pCREB positive nuclei in the hippocampus and the prefrontal cortex but did not alter expression of GAP-43 or PSA-NCAM in any of the brain regions examined. Taken together, the results of the present study suggest that antidepressant treatment increases synaptic plasticity and connectivity in brain regions associated with mood disorders. E Castrén
Eero Castrén group
Induction of neuronal plasticity the adult brain: mechanisms and applications
Eero Castrén
Professor, Director
P.O. Box 56, FI-00014 University of Helsinki
Phone: 57626 (internal), +358 50 5207974
E-mail: eero.castren at helsinki.fi
Our lab is investigating the role of neurotrophic factors and their receptors on neuronal plasticity and drug responses in adult brain. We have found that antidepressant drugs reactivate a developmental-like plasticity in the adult brain in rodents and we have coned this phenomenon iPlasticity. We first found that fluoxetine, a widely prescribed antidepressant drug, induces critical period-like plasticity in the adult rat visual cortex and brings about a recovery of vision in an amblyopic eye, when drug treatment is combined with patching of the healthy eye. We subsequently showed that fluoxetine treatment induces juvenile-like plasticity also in the amygdala, which may explain the enhanced effect of combined antidepressant drug treatment and psychotherapy in the treatment of traumatic memories. In iPlasticity, drugs have no functional effects of their own, but by inducing plasticity they promote the effects of rehabilitation and psychotherapy. We have shown that signaling of the neurotrophin BDNF (brain-derived neurotrophic factor) and its receptor TrkB is required and sufficient for iPlasticity and that several other drug classes also activate TrkB signaling. We are now focusing on the neuronal and molecular mechanisms underlying iPlasticity and investigating how adult plasticity could promote recovery in a variety of neuronal disorders. The lab is supported by the European Research Council Advanced investigator award and grants from Sigrid Jusélius Foundation and Academy of Finland.
Report comment
Pirta Hotulainen, PhD
Project leader
P.O. Box 56, FI-00014 University of Helsinki
Phone: 57606 (internal), +358 50 415 6606
Email: pirta.hotulainen at helsinki.fi
I wouldn’t mind doing some research with Ms. HOTullainen
The human brain consists of hundred billion neurons interconnected into functional neuronal circuits that underlie all our behaviors, thoughts, emotions, dreams and memories. The capacity of neurons to function within neuronal circuits is mediated via specialized cell junctions called synapses. Chemical synapses regulate the electric communication within neural networks and pass information directly from presynaptic axon terminals to postsynaptic dendritic regions. Precise control of the development and connectivity of synapses is critical for accurate neural network activity and normal brain function. Most excitatory synapses in the mammalian brain are formed at tiny dendritic protrusions, named dendritic spines (Bourne and Harris, 2008). Experimental evidence has shown that changes in spine morphology account for functional differences at the synaptic level (Kasai et al., 2003; Yuste and Bonhoeffer, 2001). It is now widely believed that information in the brain can be stored by strengthening or weakening existing synapses, as well as appearance or disappearance of dendritic spines, which subsequently leads to the formation or elimination of synapses. These functional and structural changes at spines and synapses are believed to be the basis of learning and memory in the brain (Kasai et al., 2010). During the last decade, numerous studies on signaling pathways demonstrated that the actin cytoskeleton plays a pivotal role in the formation and elimination, motility and stability, and size and shape of dendritic spines (reviewed in Hotulainen and Hoogenraad, 2010). In addition, modulation of actin dynamics drives the morphological changes in dendritic spines that are associated with alteration in synaptic strength (Cingolani and Goda, 2008). It has also been shown that various memory disorders involve defects in the regulation of the actin cytoskeleton (Newey et al., 2005).
The main goal of our group is to elucidate the mechanisms of actin cytoskeleton regulation in dendritic spines and to reveal how regulation of cytoskeletal dynamics affects dendritic spine development, morphology and plasticity. Currently, we are studying the regulation of dendritic spine structural and functional plasticity from three different aspects. First, we are studying the roles of different actin-binding proteins. Second, we are studying the effects of a novel mechanism of actin regulation -actin phosphorylation. Third, we are studying the effects of intracellular pH. We have already shown that these regulatory mechanisms affect the actin treadmilling rate. Next, we will examine how that affects dendritic spine morphology, motility and synapse function. As model systems, we use cultured rat primary hippocampal neurons and living mice or rats. Spine morphology and motility, as well as actin dynamics in spines, are analyzed by using various microscopy techniques. In addition, we use electrophysiological approaches to study the role of actin regulation in neuron function. These studies will result in a comprehensive understanding on regulation of dendritic spine structural plasticity. This knowledge is fundamental in understanding cognitive processes such as learning as well as neurological diseases.
Report comment
Beyond fascinating. These processes and activities and cellular formation that make us who we are and which I rarely think about are magnificent.
The behavioral effects of antidepressants in animal models of depression and the therapeutic effects in humans typically take several weeks to develop. Upregulation of BDNF expression and enhanced TrkB receptor signaling in the dentate gyrus, hippocampus, and cortex is implicated in the mechanism of action of antidepressant drugs such as the selective serotonin reuptake inhibitors (SSRIs). While BDNF has diverse functions, it is commonly thought that TrkB signaling during antidepressant treatment promotes or restores plasticity in affected circuits through regulation of gene expression (Castren et al. 2006; Dagestad et al. 2006). As discussed, Arc has been identified as a critical effector gene for BDNF in the context of BDNF-induced LTP in the dentate gyrus. Several studies have reported upregulation of Arc in forebrain structures in which TrkB signaling is enhanced by antidepressants (Pei et al. 2003; Alme et al. 2007; Larsen et al. 2007; Molteni et al. 2008). A recent microarray study further identified a panel of nine genes that are strongly upregulated with Arc during BDNF-LTP and HFS-LTP in the dentate gyrus and five genes selected for validation by RT-PCR and in situ hybridization were confirmed upregulated in dentate granule cells (Wibrand et al. 2006). The gene set includes several genes with known synaptic roles, such as neuronal activity-regulated pentraxin (Narp) and neuritin. Interestingly, the BDNF-regulated genes exhibited a region-specific pattern of upregulation in the prefrontal cortex, hippocampus, and dentate gyrus, after chronic (but not acute) treatment with the SSRI fluoxetine (Alme et al. 2007).
Exp Brain Res. 2010 Jan; 200(2): 125–140.
Published online 2009 Aug 19. doi: 10.1007/s00221-009-1959-2
Report comment
So, the wonderful scientists might know quite a bit about the brain. I want to ask those who have posted their “research” supporting use of antidepressants the following: Have you ever been depressed, so deeply depressed that you were told you MUST take an antidepressant? Or been depressed enough that ECT was recommended? Have you ever been so deeply depressed that you didn’t care if you lived or died? I don’t think a person can speak to depression unless they know it. You may know what happens in the brain, but that’s not too useful compared to first-hand lived experience with depression. May I ask something else? That is, do you have first-hand experience taking antidepressants? I don’t mean knowledge about the brain, I mean feeling the effects of these drugs in your body. If so, have you ever experienced the “black box warning” effect? Do you have first-hand experience with the feeling that you are jumping out of your skin and you MUST do something to end that? I can tell you I experienced this myself, less than three years ago. It’s rather difficult to put to words, but I plan to take on the challenge shortly since I am a professional writer. I’d love to hear the scientific explanation for what happened to me in my brain and body, but these explanations are flat, dismissive, and meaningless compared to what I actually felt. I am not a lab rat. I am human. I was not an adolescent at the time. I can only imagine what an adolescent (under 30) must go through. During the time I experience the Black Box Warning effect, I was hellbent on killing myself. I am lucky to be alive at 57 today. I think you need to talk to people who have been through this, and maybe you will find that your talk of the brain is a far cry from reality.
Report comment
Baughman was incorrect. Zametkin’s conclusions have been duplicated.
Report comment
Neural Plasticity and Proliferation in the Generation of Antidepressant Effects: Hippocampal Implication
Fuencisla Pilar-Cuéllar,1,2 Rebeca Vidal,1,2 Alvaro Díaz,1,2 Elena Castro,1,2 Severiano dos Anjos,1,3 Jesús Pascual-Brazo,1,2,4 Raquel Linge,1,2 Veronica Vargas,1,2 Helena Blanco,1 Beatriz Martínez-Villayandre,1 Ángel Pazos,1,2 and Elsa M. Valdizán1,2,5
1Departamento de Fisiología y Farmacología, Instituto de Biomedicina y Biotecnología de Cantabria (IBBTEC), Universidad de Cantabria-CSIC-IDICAN, Santander, Cantabria, Spain
2Centro de Investigación Biomédica en Red de SaludMental (CIBERSAM), Instituto de Salud Carlos III, Santander, Cantabria, Spain
3Stem Center, Clínica Palmaplanas, Camí dels Reis 308, Palma de Mallorca, Spain
4The Research Group for Neurobiology and Gene Therapy, KU Leuven, Leuven, Belgium
5Department of Physiology and Pharmacology, School of Medicine, Cardenal Herrera Oria s/n, University of Cantabria 39011 Santander, Spain
Received 4 March 2013; Revised 1 May 2013; Accepted 8 May 2013
Academic Editor: Chitra D. Mandyam
Copyright © 2013 Fuencisla Pilar-Cuéllar et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
It is widely accepted that changes underlying depression and antidepressant-like effects involve not only alterations in the levels of neurotransmitters as monoamines and their receptors in the brain, but also structural and functional changes far beyond. During the last two decades, emerging theories are providing new explanations about the neurobiology of depression and the mechanism of action of antidepressant strategies based on cellular changes at the CNS level. The neurotrophic/plasticity hypothesis of depression, proposed more than a decade ago, is now supported by multiple basic and clinical studies focused on the role of intracellular-signalling cascades that govern neural proliferation and plasticity. Herein, we review the state-of-the-art of the changes in these signalling pathways which appear to underlie both depressive disorders and antidepressant actions. We will especially focus on the hippocampal cellularity and plasticity modulation by serotonin, trophic factors as brain-derived neurotrophic factor (BDNF), and vascular endothelial growth factor (VEGF) through intracellular signalling pathways—cAMP, Wnt/β-catenin, and mTOR. Connecting the classic monoaminergic hypothesis with proliferation/neuroplasticity-related evidence is an appealing and comprehensive attempt for improving our knowledge about the neurobiological events leading to depression and associated to antidepressant therapies.
As indicated in this review, the importance of either proliferation or plasticity, or both, is still a matter of debate. As the involvement of proliferation and plasticity has been mainly studied in hippocampus, we might be underestimating its role in the antidepressant effect. In this sense, as the hippocampus is responsible for the learning and cognition part of the depressive disorder, the fact that the impairment of hippocampal proliferation would not block the antidepressant effect of some drugs does not necessarily conclude that the proliferation is only dependent on hippocampus. In the last years, prefrontal cortex, a structure with a great importance in mood control and working memory, is gaining increasing relevance in the plastic changes linked to antidepressant effects promoted by drugs as ketamine. In this sense, hippocampal proliferation would be only a small part of the plastic changes that are taking place within the hippocampus, and other brain areas. Thus, we must not underestimate the implication of synaptic plasticity in those antidepressant treatments that are not accompanied with increased proliferation.
You are encouraged to share the research you find which refutes these arguments. Thank you
Report comment
I felt better when I first took a Zoloft. Unfortunately the happy buzz died away in less than a month. I wonder if being permanently drunk or high on marijuana would have had a similar effect.
Report comment
Yep! Spot on! There are so many other factors at play, including inflammation and nutrient deficiencies. In fact, there are 20 nutrient deficiencies that can cause depressive symptoms: https://www.optimallivingdynamics.com/blog/nutrient-deficiencies-depression
Report comment
Removed for moderation
Report comment