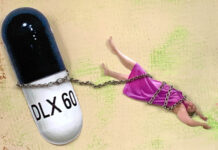
A new study, led by Joanna Moncrieff, a faculty member at University College London and co-founder of the Critical Psychiatry Network, explores symptoms associated with the discontinuation of antidepressant drugs. Results of the study, published in the International Journal of Risk & Safety in Medicine, indicate that discontinuing SSRIs and SNRIs can result in significant and long-lasting withdrawal symptoms. The authors write:
“The reported maximum duration of withdrawal symptoms was far in excess of the upper limit that is commonly quoted to patients, with both drug classes but particularly with SSRIs. Clinicians and patients need to be aware of this possibility when considering starting or stopping antidepressants.”

Prescriptions for antidepressant treatment have doubled in both the UK and the US over the past two decades, with 13% of the US population taking antidepressants. The authors note, “there is now clear evidence that a variety of symptoms can result from the discontinuation of all antidepressant classes.” For selective serotonin reuptake inhibitors (SSRIs), these symptoms include “dizziness, nausea, fatigue, headache, electric shock-like symptoms, sweating, insomnia, and nightmares.”
Less research has been done on withdrawal symptoms from serotonin and norepinephrine reuptake inhibitors (SNRIs). Withdrawal symptoms can occur whether antidepressant medication is discontinued abruptly or the dosage is gradually tapered and symptoms may last for weeks, months, or years.
According to the authors, “this study examines self-reports of SSRI and SNRI withdrawal symptoms by users of an online forum designed to help people withdraw from antidepressants” with the aim to increase knowledge about SSRI and SNRI withdrawal symptoms and duration. The authors analyzed information from 174 individuals who discontinued SSRIs or SNRIs based on their posts to the online forum, survivingantidepressants.org.
On average, participants had taken antidepressants for almost 5 years prior to discontinuation. Results suggest that withdrawal symptoms last longer for individuals taking SSRIs (average = 21 months) than SNRIs (average = 12 months). The researchers also found that duration of withdrawal symptoms was positively correlated with the length of the taper, which “is likely to indicate that people experiencing difficult and protracted withdrawal symptoms reduce their antidepressants more slowly.”
Individuals most commonly reported psychological withdrawal symptoms. Sexual and genitourinary effects were more common with SSRIs and neurological effects were more common with SNRIs. The researchers report:
“Users’ descriptions of neurological and psychological symptoms indicate experiences that are hard to classify using standard medical technology. Some, such as ‘brain zaps’ and electric shock-like sensations, have been noted before, but some are less familiar, such as ‘brain sloshing,’ ‘vision lagging behind eye movements’ and ‘head like cotton balls stuffed in’.”
The authors note that the source for the study was a website designed to help people withdraw from antidepressants and therefore individuals who are having more significant withdrawal effects are more likely to use the site. Thus, this study should not be used to estimate the prevalence of withdrawal symptoms in a general population of antidepressant users.
Given the high prescription rates of antidepressants and poor outcomes when they are taken long-term, users deserve more information about how and when they can safely and effectively discontinue these drugs. More research is needed on withdrawal from antidepressants, including effective supports during withdrawal and how to alleviate prolonged withdrawal symptoms.
****
Stockmann, T., Odegbaro, D., Timimi, S., & Moncrieff, J. (2018). SSRI and SNRI withdrawal symptoms reported on an internet forum. International Journal of Risk & Safety in Medicine, 29(3-4), 175-180. doi:10.3233/JRS-180018 (Link)














“dizziness, nausea, fatigue, headache, electric shock-like symptoms, sweating, insomnia, and nightmares.”
I’m afraid that only scratches the surface. What about suicidality? Violent urges coming out of nowhere? Tremors? Akathisia? Personality changes?
Coming off of SSRIs wasn’t just unpleasant for me. It was a drug state unlike anything I’ve experienced in my life, and I can understand why some do not survive it. Also, the brain zaps continued for 2 and a half years after my last dose.
Report comment
recovered—good post…my biggest withdrawal problem is FEAR…i still am stuck with 5 mg of celexa..
Report comment
littleturtle,
I know what you mean!
Report comment
Recovered: How long did it take for you to withdraw? Did you experience suicidality, violent urges, tremors, akathisia and personality changes?
Report comment
Yes, I experienced all of those things many times. It’s hard to give an exact timeline, because it depends on how you count. I spent a few years attempting cold turkey because no doctor talked about withdrawal. Then a year or so halving pills as much as they would go. From there I switched to liquid and spent approximately 5 years weaning off liquid, decreasing as slowly as possible. I still had withdrawal. Then 2 years with neurological issues before feeling more normal.
I should mention I hear the Recovery movement in psychiatry referred to here sometimes, and criticized. I’m not actually so familiar with what that is. I very specifically mean recovered from psychiatric drugs.
Report comment
Yes, the physical symptoms are really unpleasant, but the emotional/psychological symptoms are more frightening.
What about intense agitation and anxiety, worsening depression, panic, AKATHISIA, suicidal ideation, derealization? This is far more serious and debilitating.
Report comment
For me the emotional problems even though caused by Chemical Brain Damage, were the ones I could adapt too (thankfully, or I would never have gotten off the chemicals).
Report comment
Fiachra: Have the emotional problems gone away for you?
Have you gone back to previous state?
Report comment
truth: How long did it take for you to withdraw? Did you experience intense agitation and anxiety, worsening depression, panic, AKATHISIA, suicidal ideation and derealization?
Report comment
Missed TWO doses effexor. Tripped me into all the symptoms listed. Reinstating the evil poison my GP prescribed for 12 years for an initial two week situational depression did not “work”.
Multiple “drug trials” caused increasing sickness, which led to ECT, which destroyed 20 years of memory, left me brain damaged and suicidal.
Report comment
There is this idea that “withdrawal” symptoms will eventually “end” in a year, or two years or when the drug is reinstated.
As Dr. Shipko has pointed out, sometimes the reinstatement fails to restore a patient’s well-being and neither do other drugs introduced. He speaks of patients suffering for 5 years, 10 years, mostly suicidal, suffering often from akathisia triggered by disruption of their nervous system. What then?? He has found no solutions.
With this as a potential outcome, the prescription of these neurotoxins can’t be justified.
Report comment
Sometimes a tendency like “anxiety” remains but it’s possible to adapt to it, over time. Other problems like Nonspecific Neurological Damage can remain without any solution.
Report comment
In the context of pharmacogenetics and all the common food stuffs herbs and spices that inhibit and induce metabolising enzymes there is no such thing as one size fits all dose. Now put that with this :
https://www.healthline.com/health/depression/celexa-alcohol
https://www.gov.uk/drug-safety-update/citalopram-and-escitalopram-qt-interval-prolongation
And as people have already pointed out, the utterly horrific Akathisia. What you find is MH professionals who prescribe the drugs refuse point blank to accept any of this. The word Akathisia is not on any SSRI or any other psych drug in the UK.
Well if you want to find out Dr Moncrieff, take an SSRI and block your CYP450 enzymes with Nytol and you will experience Akathisia.
Report comment
The most disturbing thing about this study is how they had to do it. Forum posts in the internet!!
Why aren’t the supervising Doctors collecting monitoring information? From what I understand, coming off AD’s is as dangerous as going on them, so they should.
Report comment
Because they are determined not to let people come off them. They want us on their drugs for life. Period.
Report comment
Actually, the website was founded as a reference tool for doctors – since the clinical evidence was being so broadly ignored.
Niall McLaren did a study of his own patient base, which is here: https://www.madinamerica.com/2018/05/questioning-integrity-psychiatry/ But he is a rare bird.
Talk to most doctors and they say “but they helped patient,” which basically means that patient did not return (for whatever reason), or patient then returned again and again for refills of script (now physically addicted).
Report comment
Psychological symptoms though… did anyone ever think those might be because now the symptoms were no longer being treated? I had a hella bad time when I went off Effexor after 6 years because I had been great for so long and thought I might not need meds any more. Brain shocks, lightheadedness, etc… But when the irritability and anxiety and rage and trouble sleeping came back, I certainly didn’t blame the withdrawal. Why? Because I suddenly remembered that I had been like that before the med during certain times. Now that I was off it, MY SYMPTOMS WERE BACK. Incidentally, I regretted going off it because it never worked the same again when I started back on it after 6 months. I am now in Pristiq, a reformulated version of the same drug, and completely healthy and happy again.
Report comment
sggriff: Yes that is true that symptoms after discontinuing can be the symptoms of your mental condition from pre-medication. But for some people starting a medication or quitting it or taper/increase dosage (any mixture with ADs) causes extreme side-effects – more adverse, or perceived more adverse than other reactions.
I would say it is very important to know how you feel pre-medication, post-medication and during any dosage-change. Really good to keep a mood journal to be up to date regarding feelings, thoughts etc.
The ultimate goal is to feel good – that is all we should feel <3
Report comment
These psychological changes I describe were NOT a return to a previous state. They were new. I had never experienced such a state prior to SSRIs. I have been off all SSRIs a few years now. The unnatural psychological changes slowly abated as the physical adverse effects like brain zaps improved.
I have never experienced anything like it since.
Report comment
Sadly Pristiq is even harder to come off of than Effexor, due to the time release formulation of it. If you want to come off, I know of some people who have had success with compounding pharmacies for this one (though some compounding pharmacies say “it can’t be done” due to the formulation of the drug – but keep trying until you find a “can do” compounding pharmacy).
I hope it holds for you, but in my experience, “healthy and happy” don’t really go hand in hand with these drugs, and especially not in the long term.
Report comment
For me nearly all my withdrawal problems were physical. I had to spend eleven months in a single wide with my folks. Only one melt down when Dad accused me of being manipulative. He meant no harm but I have been told repeatedly how manipulative I am and how that’s part of my disease (hopeless to change) by mental illness professionals. Already sick and headachey. That sent me over the edge. My mom did some things that could be construed as emotional abuse. She was on happy pills. I blame them for her insensitivity. I used to have melt downs every week so nothing new there.
I suffered horrible pain, muscular weakness, nausea and dizziness. No brain zaps or weird mental states till I had lowered the Effexor from 150 mg to 15. Took SSRI of one kind or another from November of 1994 to July 2016 when I began my taper. My last dose was on August 31, 2017.
My aches and fatigue are better. I can work again–as long as it’s not physically demanding. But teaching, writing, coaching can be done full time I believe. Applying for a tutoring job this week. Never could find gainful employment under psychiatry’s thumb. 🙂
Going to get off government handouts. Just chump change anyhow and I felt it was used for the caseworkers/therapists to put me down. “You could never take care of yourself. Totally helpless without us. Tsk tsk.”
My only really bad problem is my body is suddenly all acidic for no reason I know of. Putting a teaspoon of baking soda in my daily supply of drinking water to alkalize it. Coming off my SSRI probably altered my physical chemistry somehow.
All in all I think I’m a success story.
Report comment
Okay so has anyone experienced any of this while using a depression treatment that is not necessarily a drug? I hope I’m not too much off subject but I haven’t seen anything about these same sentiments for Transcranial Magnetic Stimulation. I have been getting treated for my depression at PelorusTMS. The sessions are very short and I do like it way better than the drugs because I honestly started to feel not like myself while on the meds. I have been going for treatment for the past 3 weeks now. Has anyone on this post tried this before or has it ever been suggested? If you’ve never heard of Transcranial Magnetic Stimulation heres some info https://pelorustms.com/faq/
Report comment