Some researchers have been arguing to reclassify all psychiatric disorders as diseases of the brain and nervous system, similar to epilepsy or Parkinson’s disease. Neuroimaging research, however, reveals that psychiatric disorders appear to be distinct from neurological disorders, according to a new study published in this month’s issue of the British Journal of Psychiatry.
“We acknowledge that the distinction between the fields of psychiatry and neurology involves multiple factors, ranging from social and historical to biological and that any new classification should ultimately reflect an improvement in clinical outcomes,” the authors wrote.
In recent years, noting that neurological disorders can often lead to symptoms similar to psychosis and that many psychiatric disorders have accompanying physical and motor symptoms, some specialists, known as “distinction abolitionists,” have pushed for eliminating the distinction between these two classifications.
For example, in 2012 psychiatrist Peter White and his colleagues argued in BMJ that “the current line of demarcation between disorders of the mind and brain is counterproductive for clinicians on both sides of the line.” Going further, White insisted that all “psychiatric disorders should be reclassified as disorders of the central nervous system.”
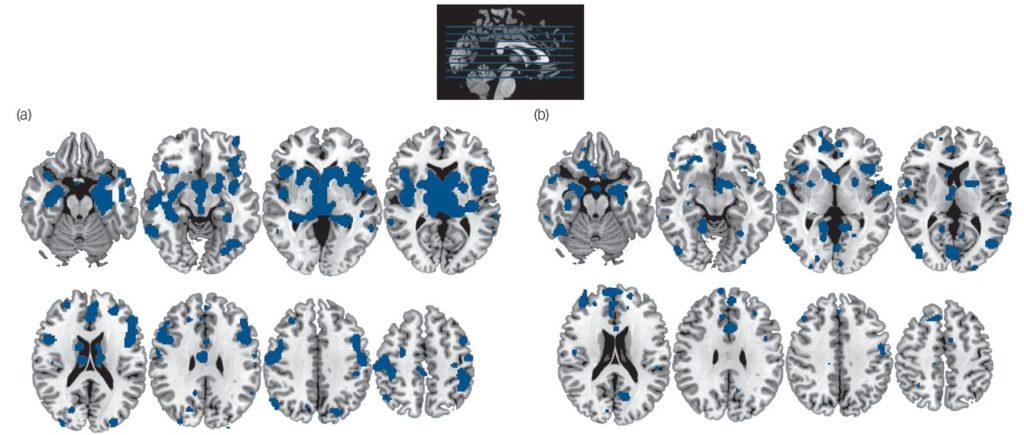
To investigate this distinction, a team of researchers, led by Nicolas Crossley from King’s College London, “examined whether the two classes of disorders affected different sets of regions, whether these regions were localized in different functional networks and whether neuroanatomical variability within each class of disorders is smaller than between classes.”
After analyzing 168 published brain imaging (sMRI) studies, the investigators that there were substantial structural differences between the two categories of disorders. “In conclusion, we have shown some divergent neuroimaging findings in neurological and psychiatric disorders; this suggests that neurological and psychiatric disorders represent two distinct classes of disorders from a neuroimaging perspective.”
This study is limited by the fact that the majority of participants in the studies of psychiatric disorders were currently taking psychotropic drugs, making it difficult to discern the structural abnormalities associated with long-term medication use and those that may be associated with a particular psychiatric diagnosis. Antipsychotic use, for example, has been linked with a decrease in gray matter in the brain.
*
Crossley, N. A., Scott, J., Ellison-Wright, I., & Mechelli, A. (2015). Neuroimaging distinction between neurological and psychiatric disorders. The British Journal of Psychiatry, 207(5), 429-434.(Full Text)















In a brain scan, if with a psychiatric disorder you don’t have a neurological disorder, the question becomes, what do you have? A psychiatric drug effect perhaps?
Report comment
There has been a study thst showed mentally ill people who were not on medicine had brain annormalities.when scanned.
Report comment
Care to give a source for that comment? Cause, you know, a friend of a friend of a cousin of an uncle once told me he saw a study showing santa claus is real.
Report comment
Stay classy Ragnarok:) I know, I am a fine one to talk:)
Anyway, I was going to ask for a link also so you beat me to it. Kaykay, I have seen many other studies that show the opposite so I am curious about your source.
Report comment
You have provoked me into writing, and defending my childhood friend, Santa Claus. As a child, I received MANY presents from Santa Claus. You know who I mean – he lives at the North pole, with his wife, and a bunch of elves, and some reindeer in the barn. The elves make the toys for all the world’s girls & boys, and Santa
delivers them all on Christmas Eve. It’s*MAGIC*. It’s Santa magic.
Presents from Santa have brightly-colored wrapping paper, and bows & ribbons, and tags that say, “To:(name of kid), and From: Santa.” I got LOTS of presents from Santa Claus as a kid.
Psychiatry & “mental illnesses” are just as real as Santa Claus.
So there! Thank-you for letting me PROVE to you, that Santa is real…..
Report comment
And, assuming you are accurate about the existence of that “study,” who decided that the guinea pigs were “mentally ill” to begin with? Did they also explain how an abstraction such as “the mind” can have a disease?
Report comment
There are no brain differences when people are first diagnosed – this is why doctors do not use (and do not have) any objective tests when diagnosing patients. They only use subjective check-lists. After a patient is given a label (based on subjective evaluations), having a label itself can be devastating, leading to more depression/worry and thinking that they are somehow different from others, etc. A label can also increase stigma making things even worse for the patient. All this mental proliferation and worry gradually bring about adverse structural changes in the brain (the mind’s ability to change brain structure = neuroplasticity).
Report comment
RE: “After a patient is given a label ” this is also in the context of voluntary VS involuntary “medical” treatment. Some people do seek a label from an official.
In other terms a psychiatric diagnosis is simply a description of the behaviour of the “patient”.
But with the magic of PAPER the diagnosis is written down to be remembered forever more. Never forgiven for your sins.
Such as the diagnosis of a broken leg is written down on paper. The difference between the broken leg diagnosis/description and the psychiatric diagnosis/description, is that everyone expects the mental illness is forever, but the leg to heal.
Report comment
Hi Frank
The drugs certainly damaged me, and left me dysregulated in a way I had never been before – but my recovery was through non drug help.
Report comment
I’m seeing this study as a wolf in sheep’s clothing insofar as its relevance to exposing psychiatric mythology.
To wit: What is being studied is people with actual diseases vs. people with alleged diseases. But part of the “given” in this is that the “psychiatric disorders” group has already been accepted as such rather than hypothesized as such. So, a likely disparate group of people who have been given this or that label are lumped together as those with “psychiatric disorders,” then their brain scans are interpreted as having some meaning in this regard. But in fact the whole approach appears to be bogus, and the study implicitly supports the idea of “psychiatric disorders” being somehow grounded in brain chemistry.
I was not predisposed to this conclusion btw as I was hoping we would have something concrete here to help blow Torreys’s own brain scan gimmickry out of the water.
Report comment
Interesting comments, oldhead. It is correct that the study’s results are, as usual, couched in the delusional language of distinct psychiatric disorders which are presumed to exist as separable entities a priori. As you and I both feel strongly about, that is ridiculous.
But, I think this study has value because it is another in a long trend of studies which keep challenging established psychiatric wisdom about diagnoses, drugs, etc. The positive thing here is that the results made psychological problems (speaking in everyman reality-based language) appear, correctly, to be qualitatively different in the way they affect the brain than those which are clearly caused by physical problems like dementia.
Report comment
It also makes the leap of faith, rather than logic, that the atypical brain areas or “dark spots” or whatever have anything to do with whatever issues ended up with the person being diagnosed with a “psychiatric disorder.” This is supremely unscientific if you ask me; I’d rather make the attack on “chemical imbalance” hypotheses using studies that I feel convinced by myself. As it stands they can still use these findings to “demonstrate” that “psychiatric disorders” are rooted in brain chemistry, though maybe not so much as Alzheimers, etc.
I’m sure no biochemist, and I didn’t read the whole study, but even if those impressive pictures show something going on here or there in the non-neurological group’s brains it could mean anything, good or bad or neither. In one person it might be an adaptation to an old concussion, in another a residual (or current) effect of drugs, and so on. Because in reality there is no category “people with psychiatric disorders,” only people diagnosed with “psychiatric disorders.”
Anyway, I’m still looking for the “perfect study” with which to relegate Torrey’s propaganda to the same historical dustbin that holds Mengele’s.
Report comment
I don’t see any significant gains coming from a study of this kind. The researchers are calling both neurological and psychiatric disorder “diseases”, but they say they are different “diseases” of differing severity and affecting different areas of the brain. What they are not doing is taking a serious look at the drug induced disability involved. Where is the line, different areas of the brain are affected? Or are we really dealing with drug effects? As long as research is intent on finding biology as the source, and chemistry as the answer, I think you’re going to get this kind of thing. Obviously, we’re dealing with two different things. When a disease is determined to be neurological it ceases to be psychiatric. Okay, brain scans say, yes, indeed we’ve got two separate phenomenon. Problem is one is in all likelihood disease, and the other is, in all likelihood, prescription drug effects. Researchers are under no compulsion here to jeopardize the chemical gold mine and quick but debilitating fix they’ve developed. Bias (prejudice by any other name) taints the entire field.
Report comment
It is also important to remember that these brain scan studies always use averages of a large number of scans. Any individual person’s scan may vary widely from the average, and the scans you see represent at best general correlations of what is MORE LIKELY to occur in one condition than another. Of course, this is to be expected, given the heterogeneity of people who happen to get any one particular label, and it’s always important to keep in mind that any similarities are more likely to be related to treatment effects than to any similarities the participants may have had preceding “treatment”.
Report comment
This is interesting. It suggest that trauma, stress, and deficits in interpersonal relationships leading to terror, rage and confusion (i.e. the mythical “schizophrenia”) affects the brain in observably different ways than dementia or Parkinson’s. That does make sense, when you think about it.
Report comment
Wow, I really like your concise, clear, & accurate description of so-called “mental illness.” Very nicely done. Do you mind if I borrow it or a version of it?
Report comment
Sure, thank you. Feel free to post a link to where you write!
Report comment
And despite that, there is no single “diagnosis” that can be even close to predicted by brain scans of any type. The pictures they show you of the “ADHD brain” are AVERAGES over many people. Not all “ADHD” people have that particular brain scan, nor do all with that kind of scan show any signs of “ADHD.” Daniel Amen, the brain scan’s biggest proponent, even admits that the so-called “ADHD” brain is also seen in people with brain injuries as well as diagnoses of schizophrenia and one other “disorder” I’ve forgotten.
Also remember that these are brain ACTIVITY scans, not structural scans. So they reflect how you USE your brain at a given moment. They are fluid and active and respond to external stimuli (the “ADHD brain” is apparently only observable when you make the subject do something they find tedious or stressful, so maybe it’s the “bored brain” or the “stressed brain?”) There was a study I recall where they had people think of something sad, and their brains went in the direction of the “depressed brain” averages. When they then thought of something happy, their brains changed back.
Brain scans should be renamed “Brain scams.” They don’t diagnose anything.
— Steve
Report comment
the “ADHD brain” is apparently only observable when you make the subject do something they find tedious or stressful, so maybe it’s the “bored brain” or the “stressed brain?”
Excellent observation!
Bored students in boring school systems are given speed to compensate for the system’s failure, because speed makes everything more interesting.
Report comment
Right! It’s artificial stimulation to make up for the lack of expected natural stimulation. Why not instead make the environment more stimulating? But that would require the ADULTS to make the adaptations, and it’s much easier to put the blame on the powerless and continue with our own misconceptions unchallenged.
Report comment
They always talk about “learning disablilties,” never teaching disabilities. Though I wonder what they would prescribe if the latter were added to the DSM.
Report comment
This also reminds me of when (here I go seriously dating myself) Timothy Leary used to talk about “set and setting” in relation to the LSD experience, i.e. where you were physically and mentally after ingesting it. If so-called ADHD brain scans depend on one’s mood, expectations and physical surroundings while they are being done, visualize the conditions under which those procedures are generally conducted and draw your own conclusions as to the significance of the results…
Report comment
The stupidity and insanity of biological psychiatry never ceases to amaze me. They have claimed for decades that ‘mental illness’ is a real biological illness, brain disease, or chemical imbalance, even though no such evidence exists to support such claims. After decades of research they still have not found anything wrong with the brain regarding ‘mental illness’. So what do they do in the face of this total lack of evidence? They seek to reclassify and redefine psychiatric disorders as brain diseases. Absolute insanity.
I say it again. Psychiatrists don’t treat the insane. They are the insane.
Report comment
Very cogent comment! I totally agree. Would that the general public had any idea of the degree of stupidity and insanity, not to mention cruelty and harm, of biological psychiatry. They don’t treat the insane, they are the insane, that’s perfect.
Report comment
Psychiatrists don’t “treat” the insane – they ARE the INSANE.
Report comment
Well said and amen.
Midevil science persists and it’s time it stopped. They robbed me of a decent, loving and career oriented life. They perpetuate these lies to support themselves.
BTW, I just more or less had a pretty bad experience at ATMC in Sedona, AZ. I left after a week. A good number of their staff are ex-cons (I didn’t discover this until I went there), including I think the owner (who I’ll not name at this time). I suggest men and women who have a little bit left of their brain function to stay away (unless you like ex-cons in a cult environment) and find ways to reduce and/or eliminate their toxic poisons through their own research and resources. 40K for 8 weeks of ….
Report comment
In a perfect world, every “mentally ill” patient would be brain scanned on a yearly basis , like our teeth are X-rayed to detect cavities, to see if and where brain damage, or brain changes are taking place.
But as you all know , there is nothing physically wrong with the brain in the mentally ill, the mentally ill are not following orders of those in authority ( involuntary psychiatry).
In the case of voluntary psychiatry , people believe something is physically wrong with their brain and need a medicine for their illness ( from a psychiatrist-doctor).
As science is confronting the legitimacy of psychiatric drugging (nothing wrong with the brain), I have hope for the future. Like phrenology went out of fashion, psychiatry might as well.
Report comment
Psychiatry is 21st Century Phrenology, with “meds” – DANGEROUS “meds”.
Report comment
Oldhead,
I agree that it is absurd to discuss the neuroscience of an abstract concept like the mind and that this article is more pseudoscientific support for the medical model.
However, real science explains human psychology and mental distress; examine this study closely and the pseudoscience becomes evident. This study examines areas of the brain that have atypical decreases in gray matter between neurological patients vs. psychiatric patients. Neurological patients are defined as having “organic” problems- identifiable problems with brain neurobiology; the decreases in gray matter (brain volume) are logical products of recognizable biological problems. In contrast, psychiatric patients are defined as having “functional” problems- without identifiable problems with brain neurobiology; these decreases in gray matter are logical products of emotional distress or neuroleptic drug abuse. The decrease in areas of brain functioning (and a correlated decrease in gray matter- brain volume) is a logical product of long-term depression, anxiety and/or neuroleptic drug abuse. Since neuroleptics reduce brain functioning, it is logical that they cause a correlated reduction of gray matter.
“Mental illness” is a myth. There is nothing functionally wrong with the brains of psychiatric patients; only pseudoscience supports the medical model. Distressful experiences naturally cause painful emotional distress; emotional suffering is not a brain or (mental) disorder.
Best wishes, Steve
Report comment
Nothing to take issue with here except possibly this:
The decrease in areas of brain functioning (and a correlated decrease in gray matter- brain volume) is a logical product of long-term depression, anxiety and/or neuroleptic drug abuse.
Not sure if you can legitimately put emotional/psychological states in the same basket with neuroleptic drug effects. Also, practically speaking, people in these studies with various forms of emotional distress are also taking drugs so it would be hard to differentiate.
If I were study prone I might suggest choosing several hundred random people off the street at noon, giving them brain scans and seeing what can be extrapolated from that. But that’s a lot of radiation just to prove a point.
Report comment
The radiation is said to be insignificant “In higher elevation areas such as Colorado, the background exposure can be up to 10 millisieverts per year, yet no increased incidence of cancer in higher background radiation locations has been observed. A CT scan can deliver anywhere from 2 to 10 millisieverts of radiation, depending on what type of scan a patient receives. For exams requiring multiple scans, this can add up to 20-30 milliSieverts, but this is still considered a low dose of radiation. For some, scans, such as a head CT, the exposure is very low, about 1 – 2 milliSieverts.”
and “Some patients will opt to have the MRI because it does not use ionizing radiation.”
http://www.news-medical.net/news/20130531/Mayo-Clinic-experts-provide-some-insight-about-radiation-dose-from-CT-imaging.aspx
Report comment
I assume that we are discussing atrophy from lack of use rather than some mystical (invisible) disease eating our brains. Hence I agree that long-term neuroleptic abuse would be the predominate cause of atrophy in some areas of the brain because it causes a reduction of brain activity.
Best wishes, Steve
Report comment
I don’t even know what those gray areas signify, is there scientific agreement on that?
Report comment
The psychiatrists are making stupid people more stupid in order to “help” them. I predict the next swing of the pendulum will be to make stupid people smarter instead.
Report comment
Nervous tissue is divided into “gray matter” and “white matter.” “White matter” is nervous tissue that guides the flow of neural communication through the peripheral nervous system and much of the brain; it creates common pathways fixed by hereditary. “Gray matter” is predominately found in the brain; our interaction with the environment creates our unique patterns of neural communication that creates unique thinking by “gray matter.”
There is no scientific agreement on the significance of decreases of gray matter in “functional areas” of the brains of psychiatric patients. Neuroscientists cannot understand an obvious explanation because they investigate the absurd; they investigate how a mystical (invisible) disease is causing an abstract concept of a “mind” to malfunction. Instead, real science would assume that chemically paralyzing the brain with heavy sedatives will naturally cause patterns of atrophy- a decrease in gray matter. Neurology investigates brains with functional problems; psychiatry is causing functional problems by medicating natural emotional pain from distressful experiences as if it was a disease.
Best wishes, Steve
Report comment
OK so step by step here…
There is no scientific agreement on the significance of decreases of gray matter in “functional areas” of the brains of psychiatric patients.
Is there any agreement on the significance of gray matter decreases in general?
Report comment
Oldhead,
That is a good question; I was hoping that someone with a medical school background would have responded by now. I assume that imaging dark spots described as “organic” loss of gray matter include problems from strokes or trauma. With strokes, I assume that blood clots block blood to areas of the brain and cause a reduction of gray matter from lack of nourishment beyond the blockage. With trauma, I assume trauma tears established pathways of neural connections (neural communication) and thereby causes inactivity beyond the point of trauma and a reduction of gray matter from atrophy. But I do not know it there is agreement on this or if I am missing something significant; can anyone else comment?
Best wishes, Steve
Report comment
“atrophy from lack of use” brain tissue loss is from the poison, not from lack of use. Like saying a frogs legs have atrophied from lack of use , when they have been chemically paralyzed or cut off.
Report comment
If you chemically paralyze a frog’s legs, they will atrophy over time. There is nothing diseased about chemically paralyzed legs but the volume of muscle tissue will decrease from lack of use just as nervous tissue will decrease from lack of use.
Best wishes, Steve
Report comment
Right on.
Report comment
The article doesn’t specify that they have indeed found any brain abnormalities among people with supposed MI beyond what has been caused by treatment. We know that neurological disorders are detectable via testing, often including unusual seizure activity or deterioration (in the case of dementia, or injury if sustaining a TBI (including ECT). The article only states that studies have shown “differences” between those with neuro abnormalities and those without. It doesn’t state differences between the supposed MI and the general population, beyond what is caused by the various treatments, and possibly poverty, lack of sunlight, malnutrition, and neglect, also caused by treatment.
Report comment
I just read a story of a nun who had no signs of any mental decay whatsoever, but her brain was full of plaques and tangles of Alzheimer’s (see: http://www.thestar.com/news/world/2015/11/24/how-nun-dodged-alzheimers-part-of-dementias-mystery.html )
Makes me wonder if a brain is even necessary?!
Report comment
This is not new, but also not published. Apparently, people who are at peace with their lives are much less likely to develop the full range of Alzheimers symptoms even if their brains are falling apart. They may not remember things, but they don’t get disoriented and confused and hostile and delusional. So even Alzheimers, which clearly has a physiological component, is not entirely a “brain disease.” Experience and attitude are factors even when your brain is dying off.
Report comment
“Experience and attitude are factors even when your brain is dying off.”
Indeed, I believe they are critical factors in adapting to any kind of change, which of course, is inevitable. I’d also add that how we apply our wisdom factors in here, too, which I guess is related to experience. That’s exactly what heart consciousness is, which is what dictate our desires and our capacity to love. It is also how we heal from trauma–through the heart.
Report comment
They may even have good memory – before improved standards of antenatal care were available, Lorber (1981) had studied hundreds of patients who displayed normal and above normal IQ’s in spite of having severely reduced brain tissue. [Reference: Lorber J. Is your brain really necessary? Nurs Mirror. 1981 Apr 30;152(18):29-30.]
Also there had been an article in Lancet titled “Half brain but not half function”: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(02)09793-3/references
Report comment
Ah, so a meta-analysis of 168 phrenology, I mean MRI studies shows “structural” differences between different types of disorders. Well, if you include lacunar infarcts, hydrocephalus and such as neurological disorders, I bet there was a difference. When it comes to brain tumors, imaging is a valuable and lifesaving tool.
However, when it comes to function, imaging is largely an expensive exercise in pseudoscience. “Structural” differences in populations are forever being proposed and deposed. Comparisons are based on small convenience samples. If there were normative sizes and shapes for different brain structures, we could measure deviations from the norm in clinical populations. But there are no such norms. So we are free to compare clinical populations to whatever sample we wish, get funding, and publish pretty false-color pictures “proving” our pet theories.
Report comment
That sounds like a pretty cool gig.
We could even make tons of CA$H by selling them lots of potent placebos!
Placebos are the only true panacea for phrenological phenomena, such as
pseudo-scientific psychiatry.
Report comment
They will never be able to see souls with electromagnetic scans.
Report comment
Amen to that, and the soul/spirit of psychiatry as a profession died long ago. RIP.
Report comment