Recent data, published in The Canadian Journal of Psychiatry, finds that a large proportion of adults with intellectual and developmental disabilities (IDD) are prescribed antipsychotic drugs. Researchers found this to be the case for both those who have been diagnosed with psychiatric disorders and those without any documented diagnosis.
“These findings suggest that future attention to the appropriateness of antipsychotic prescribing for adults with IDD in Ontario is warranted,” the authors write.
A greater awareness and acknowledgment of the inappropriate use of antipsychotics to manage behavioral and psychological symptoms in children, youth, and older adults has led to a number of policies attempting to educate providers and protect vulnerable populations, particularly older adults with dementia symptoms.
While these efforts may have made an impact in protecting adults with dementia, adults with intellectual and developmental disabilities (IDD) represent another population vulnerable to being inappropriately exposed to this class of drug. Despite the risk, however, less attention has been devoted to this population.
Dr. Yona Lunsky and a team of researchers in Canada sought to gather population data on the extent of antipsychotic use by adults with IDD as a way to document the problem and to rectify the issue in the Canadian psychiatric community.
Evidence indicates that in the UK, the Netherlands, Australia, Norway, and the U.S., adults with IDD are frequently prescribed antipsychotics in response to either or both “psychiatric disorder” presentations and “challenging behaviors,” write the authors. Yet, they raise the fundamental concern that research on the efficacy of long term antipsychotic use is absent (see MIA report), support for short-term efficacy is inconclusive, and adverse side effects are grave (see MIA report).
Furthermore, the ability to consent, to report the presence of adverse effects, and to generally communicate about treatment with providers is complicated by cognition and memory symptoms related to disabilities.
For this population-based cohort study, researchers monitored the antipsychotic exposure of 51,881 participants from Ontario between April of 2010 and March of 2016 using a government health care program. Participants were adults (aged 18-64 years) with an IDD diagnosis and featured a subgroup of 4,073 individuals who were living in group homes. With access to various databases, the researchers were able to gather information on all current and previous participant psychiatric diagnoses, procedures, and medications.
Among all of the participants, 39.2% were dispensed at least one antipsychotic, a figure that increases to 56.4% of participants when looking only at those who lived in group homes. Most prescriptions were for persons diagnosed with “atypical psychoses.” Demographic data indicated that most antipsychotic users were, on average, 42-years-old, male (58.8%), and living in an urban area (85%).
Almost one-third (28.91%) of individuals using antipsychotic drugs had no documented psychiatric diagnosis. Antipsychotic users without psychiatric diagnoses were slightly older, wealthier, and less likely to live in an urban area than antipsychotic users with a psychiatric diagnosis. They were also more likely to have been prescribed lithium or an antiepileptic drug, but less likely than those with a psychiatric diagnosis to have been prescribed antidepressants or benzodiazepines in the year preceding the antipsychotic prescription.
“Individuals prescribed antipsychotics had a host of medical concerns and were frequent health service users.”
It is important to note that “psychiatric diagnosis” included “major depressive disorder” in this study. A similar study that did not include depression as a psychiatric disorder found that only 29% of those treated with antipsychotics had a serious mental illness documented in their primary care file, diverging from the 40% estimate found in this study.
Estimates that over half of adults with IDD in group homes are prescribed antipsychotics and that, overall, 2 in 5 adults with IDD are prescribed antipsychotic drugs lead the authors to voice concern surrounding the appropriate prescription of these drugs and the steep financial costs incurred.
“Further research is required to fully understand the multiple factors contributing to antipsychotic prescribing in our country, which could inform proposed interventions.”
The researchers suggest that part of the problem may arise from prescribers lacking sufficient knowledge of IDD. The same may be true for staff in residential homes, they propose, alongside additional system-wide challenges.
“Future research and policy in Canada should focus on the extent to which antipsychotics are being appropriately prescribed in this highly vulnerable population, including using chart audits and other feedback mechanisms.”
****
Lunsky, Y., Khuu, W., Tadrous, M., Vigod, S., Cobigo, V., & Gomes, T. (2017). Antipsychotic Use With and Without Comorbid Psychiatric Diagnosis Among Adults with Intellectual and Developmental Disabilities. The Canadian Journal of Psychiatry, 0706743717727240. (Link)















What would be an “appropriate” use for these toxic poisons that shrink the brain and cause brain damage?? There isn’t one.
Report comment
Truth I agree but as one who has seen and experienced multiple perspectives- even I would have to admit there can be rare circumstances that usage is the only option left. That is why there needs to be trauma sensitive treatment, money for standard and alternative treatments, well paid and cutting edge informed staff from janitors up the line.
There is such a thing as disability fatigue. My family has been very very aware and our ability to handle difference and otherness fairly high though definitely not perfect. Our family has had a multiple perspective on disability through personal experience. One family elder came back from a family event and said there were just too many disabled folks to have a relaxing time. And this was said with love. If we are going to a near if not complete medication philosophy then we must acknowledge and accept families and staff will need supports just as much as those in need or crisis. Lopsided approaches and views are ignorant and doomed to failure.
Trauma informedmeans thewhole 9 yards,the whole cobbdle from
prevention to everything else.
It also means we must all accept we fit into the other category now and then or lifelong. Sometimes both- sometimes on a variety of different levels. Use of chemicals should only be used as a desperation measure. If services were really well funded, proactive, and all encompassing I would hope greatly that the option would be used if at all very very infrequently.
Report comment
I asked a Professional Expert here once–that since she recommended neuroleptics for cases of violent or extremely agitated behavior in psychotic individuals with little hope for recovery–why not use tranquilizers instead. Since tranquilizing was all she really was attempting. She never deigned to answer.
My guess is, they need to use neuroleptics instead of tranquilizers, to keep up the facade that they are indeed DOING SOMETHING and fighting psychosis with antipsychotics instead of just numbing the victim and making them into a semi-vegetable or zombie.
Report comment
Truth writes the truth: “What would be an ‘appropriate’ use for these toxic poisons that shrink the brain and cause brain damage?? There isn’t one.” Bingo.
There is no “appropriate” use of toxic poisons that shrink the brain and cause brain damage. Where are the courageous people at Mad in America who aren’t afraid to communicate the truth to the general public? I challenge all those at Mad in America or who read these articles, those who know the real history of psychiatry, to stand up and be counted. Enough equivocating. Enough acquiescing to the powers that be. Slay the Dragon of Psychiatry.
Report comment
“Truth writes the truth: ‘What would be an ‘appropriate’ use for these toxic poisons that shrink the brain and cause brain damage?? There isn’t one.’” I agree, too.
Report comment
Maybe by “inappropriate” Zenobia was referring to off label use? That would have been a better term since appropriate/inappropriate are highly subjective. I agree there is no appropriate use for neuroleptics.
In my 25 years as a “consumer” I have only known one dangerous person considered SMI. He wasn’t psychotic, but violently angry at being imprisoned in the psych ward. If he had hurt me, it would have been “friendly fire.” He really only wanted to hurt the staff.
Report comment
Too long in coming but I will take it. Thanks. There has been a long history that is mostly covered up behind this research. Back in the days of institutions, there were attempts to separate folks based on cognitive function but this was after WW1 and the indriduction of IQ testing in soldiers. Many inmates were commuted due to all sorts of issues and many times those with nonsimilar issues were committed. I still remember a an “inmate”of a state institution for the Developmentally Disabled trying desperately to use the very weak process available to him to get out based on the fact he was not developmentally diabled.
In some states services are tied together in other states not. Therefore many times the monies go in unequal portions to Developementally Disabled systems rather than “mental health”
This creates a wedge among family members – jawbreaking at times to me. On the radio I heard a sister of a developmentally challenged woman state – “but she’s not crazy”
In another instance if a life long MH labeled man say-“but he’s not retarded”
Many folks after deinstulization started taking place went directly to nursing homes – even children.
I can easily see how medication was used to make it easier on staff with bare bones staffing and almost no training.
Many group homes are run by immigrants and they bring their own trauma issues with them which adds another layer to the mess.
Monies are barrel scraping for many programs- like many areas of social services in our country today and that makes the use of medication the go to response BD with the historical amnesia and lack off i depth education and training many programs are being run by administration and staff who are completely ignorant about best practices.
The other issue not addressed here but should be is the high rate of abuse. Developmentally disabled folks are prime targets and putting them on these types of medications only aids offenders. In a state wide training on offenders they interviewed a hospital staff member who worked with
compromised patients and abused them knowing they had no ability to tell on him.
Another issue is how to handle problematic behaviors. Medication should be at the very end of the line. The idea of “least restrictive environment”isessential. Every
every program that works with folks in need needs to have a team approach and medical ethicist on board.
Expensive yesbutwho everpriseddoing the right thing would be easy or inexpensive?
Report comment
Sorry for the typos
. Thanks
Report comment
Regarding “individuals using antipsychotic drugs had no documented psychiatric diagnosis.”
If I had a broken leg twenty years ago and I go to see the doctor, will he/she put a new cast on my healed leg? No, because too much time has passed. Similarly the application of psychiatric drugs on to people who had a history of taking psychiatric drugs is insane.
Report comment
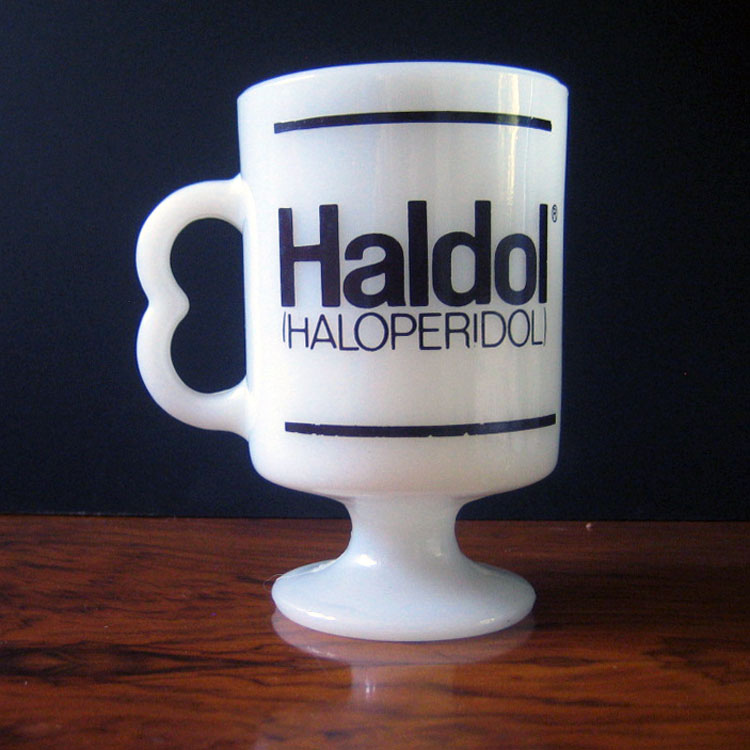
Regarding the photo of the Haldol mug. I STOLE one from a psych ward and kept it many years. It didn’t look like that mug, though. It looked more like a standard diner mug. It had a crack in it, I recall, never quite looked clean. Held about ten ounces of coffee maybe.
I stole the mug during my first, or perhaps my third hospitalization/imprisonment in Putnam Memorial Hospital in 1983. Undoubtedly the nurses knew I stole it. I was on the fifth floor, end of the hall where the psych ward was. It’s now called Southwestern Vermont Medical Center. Guess they wanted something more generic. They did away with the psych ward, too. that I know of. I no longer own the mug. I tossed it. I had some pens, too, guess like everyone did.
I suppose this was off topic but I saw that Haldol mug and it brought back memories.
Someone I know drugged their kid……..who had a developmental delay or something…..terrible. For a behavior “control” thing.
Report comment
The Haldol mug was cracked? Ironic–and appropriate.
Angers me. Developmentally delayed people already have brain problems. So we want to damage their brains even more? Sickening!
Report comment
The Royal College of Psychiatrists – everybody :
“It is important for professionals to be aware that intellectual disability associated with abnormally aggressive or seriously irresponsible behaviour could potentially be a mental disorder, even if a person does not have a mental illness”
http://www.rcpsych.ac.uk/pdf/FR%20ID%2004%20for%20website.pdf
Report comment
Understand the anger. I have relatives on meds. I give them my views.It’s a hard call even when I was aware at some point I fell into line with horrific results for me.
Just so you know. Sometimes the options are very, very poor. A old old friend was a social worker way back before the 1950’s. She had a lovely family with a very very brain damaged CP small child that could only literally cry. There was no capacity for human emotion – my guess is that the brain must have been malformed or something awful happened. As a social worker she and she was very aware of the maltreatment in institutions tried to help the family get the child in the institution for relief . the child screamed and slept, screamed and slept in a non cyclic way. the family had go to court their petition was denied because the state would only take children five and beyond. there were no meds then just placement in an attic. Not good.
Until all of you can use the brains that I know you have to open your minds that sometimes despite. the bad bad issues sometimes people have the right to use medications as the only option left. If yo
Be kind, have mercy. If you haven’t worked with DD folks with severe impairments don’t comment. it shows. You are getting angry at the choir. Here . And yes. I am anonymous and yes I have been on the other side. But don’t do what Big Pharma does and paint everything on just two sides. The snarky stuff does not become you. Keep your minds open when triggered and in anger. And I have empathy rage – sometimes I want folks to feel what I have felt in solitary confinement.- Walk away and write on a different day. WE need all of your voices just not the voice coming from the trauma and suffering we all had. I think of Mandela. Years of prison. We all can do this. And I will tell you I fail all the time and my curses are truly vile.. If I was a Big Pharma person I would be shuddering!! Yikes!
Report comment
Catnight
I understand where you’re coming from.
And although I am so antipsychiatry, something has to be done for that screaming child. The huge problem is that psychiatry with being allowed to give their treatments, is and has caused much more harm than good.
Their help takes away power of families, who no longer have any say over the child.
A GP could prescribe meds, we don’t need psychiatry that makes everyone carry a label which permeates all aspects of their lives.
That child is an extreme example and I would think is a neurology case, who I would think can prescribe.
Report comment
I guess as long as we are not willing or able to help look after the needy, then control happens. It is where the tax dollars go.
Psychiatry and institutions are not invested in us as humans. They don’t feel any particular attachment or love for needy people.
Here is your tag, your meds and your pittance. Get lost. Ohh and don’t forget, you no longer hold a valid citizen passport.
Report comment
There should be a new standard on human treatment.
If you can’t come up with less horrible drugs, no one should be medicated.
Look back. Do you think it was nasty to take chunks out of the brain?
The drugs are worse, but people like it better if it does not involve knives.
And quit telling everyone about the masses of dangerous psychosis.
We will look back again.
Report comment