Dr. Madhukar Trivedi and colleagues investigated the effectiveness of sertraline to treat depressive symptoms in patients with Chronic Kidney Disease. The results of the new study, published in JAMA, indicate that sertraline does not significantly reduce depressive symptoms in this population. The authors, therefore, do not recommend sertraline for patients with Chronic Kidney Disease experiencing depression.
“These results provide evidence regarding the lack of efficacy of sertraline among patients with non-dialysis-dependent CKD [Chronic Kidney Disease] that would change clinical practice,” write the researchers.
The senior author of the study, Dr. Madhukar Trivedi, is a professor and Chief of the Division of Mood Disorders in the Department of Psychiatry at the University of Texas Southwestern Medical Center. He is a renowned researcher on the efficacy of depression treatments, especially antidepressant medication, and reports being an “advisor or consultant” to a number of pharmaceutical companies that manufacture antidepressant drugs.
Dr. Trivedi was a co-principal investigator of the NIMH-funded Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, the largest antidepressant efficacy study ever conducted. The researchers of the STAR*D study used their findings to suggest a 67% remission rate for depressed patients who use antidepressants. However, the STAR*D study’s methodology and the conclusions drawn from the results have been heavily criticized, including calls that the findings be retracted. The present study reports very different outcomes, questioning the effectiveness of sertraline for depressed patients with Chronic Kidney Disease.
The authors report that 15% of the US population has Chronic Kidney Disease. A quarter of individuals with kidney disease also experience depression, which is four times the rate of depression in the general population. Individuals with comorbid kidney disease and depression have worsened patient-centered outcomes and higher rates of hospitalization, dialysis, and death.
The researchers note, “Evidence for placebo-controlled efficacy of commonly used antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), is limited among patients with CKD [Chronic Kidney Disease], who generally have been excluded from large randomized trials of antidepressant medication treatment due to safety concerns.”
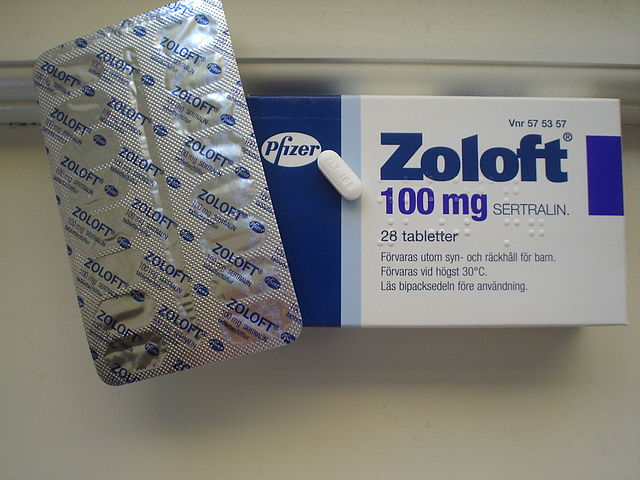
Therefore, the authors designed The Chronic Kidney Disease Antidepressant Sertraline Trial (CAST) to evaluate the effectiveness of sertraline, a widely prescribed SSRI, at reducing depressive symptoms in patients with Chronic Kidney Disease.
The study was a double-blind, placebo-controlled, randomized clinical trial. The authors recruited 201 patients who were non-dialysis dependent in stages 3, 4, or 5 of kidney disease (i.e., moderate to end-stage kidney disease). Participants were randomized to either receive sertraline or placebo for 12 weeks. The researchers measured depressive symptoms using the Clinician Rated Quick Inventory of Depression Symptomatology (QIDS). A total of 193 patients were included in the final analyses.
Findings show no significant difference in depression symptom reduction between the sertraline group and placebo group (QIDS score between-group difference was 0.1 points on a 27 point scale). Remission rates were also not significantly different, nor was there significantly different improvement in overall quality of life or health.
The one exception is that participants taking sertraline reported significantly improved sleep compared to the control group. The researchers describe any effect sertraline may have had as “clinically irrelevant” and conclude, “it is unlikely that sertraline is effective for depression treatment in this patient population.”
The researchers find that participants taking sertraline reported higher rates of nausea, vomiting, and diarrhea. They summarize:
“Although sertraline did not result in increased serious adverse events or bleeding, it did increase the rate of adverse gastrointestinal symptoms. These types of adverse events are particularly undesirable among patients with advanced CKD [Chronic Kidney Disease] because they are already prone to uremic symptoms such as nausea and vomiting.”
The authors speculate why sertraline was ineffective in this population. They highlight that 84% of participants were unemployed, and cite findings from the STAR*D study: “socioeconomic factors such as unemployment were shown to be associated with a low likelihood of antidepressant treatment response.” The researchers also question whether depression experienced by chronically ill individuals is “a different clinical entity” than ‘psychiatric’ Major Depressive Disorder. They state:
“These findings are in line with increasing evidence from well-powered trials among patients with other chronic medical conditions, such as asthma, ischemic heart disease, and congestive heart failure, that found SSRIs were no more efficacious than placebo for treating depression.”
In light of the findings, Trivedi and colleagues recommend, “Future studies need to explore whether non-SSRI medications or nonpharmacological therapies can result in improvement in depressive symptoms among patients with non-dialysis-dependent CKD [Chronic Kidney Disease], who are at a disproportionately higher risk for depression and its complications than the general population.” These findings add to a growing body of literature questioning the efficacy of SSRIs to treat depression.
****
Hedayati, S. S., Gregg, L. P., Carmody, T., Jain, N., Toups, M., Rush, A. J., … Trivedi, M. H. (2017). Effect of sertraline on depressive symptoms in patients with chronic kidney disease without dialysis dependence: The CAST randomized clinical trial. The Journal of the American Medical Association. Advance online publication. (Link)















The idea that SSRI’s would have any effect on depression instigated by toxic metabolites seems to be an element of some bizarre biochemical fantasy.
Report comment
My understanding was that antidepressants haven’t been shown to beat placebo response for mild to moderate depression.
Report comment
You forgot to mention the SSRI’s create the symptoms of “bipolar.” And that the medical community has misdiagnosed the adverse effects of the antidepressants as “bipolar” in millions and millions of Americans already, including over a million American children, resulting in the completely iatrogenic “childhood bipolar epidemic.” And you forgot to mention that the SSRI’s and SNRI’s can also make a person “psychotic,” via anticholinergic toxidrome poisoning.
https://en.wikipedia.org/wiki/Toxidrome
The SSRI’s and SNRI’s are ineffective and harmful for all people. The SNRI’s are NOT “safe smoking cessation meds,” as the medical community fraudulently claims. But they do cause people to increase how much they smoke. “Psychiatric patients smoke because the hydrocarbons in cigarettes induce the enzymes that metabolise antidepressants and antipsychotics, and as a result they feel less toxic and more comfortable.”
https://www.madinamerica.com/2017/10/mortality-mental-health-services/
Report comment
An SSRI created my “Bipolar” disorder. The doctors fed my mom some bovine excrement about how Anafranil had only “unmasked” my insanity lying there all along. They claimed I would need “mood stabilizers” and neuroleptics as well as SSRI’s. Cha-ching! $$$$
What nobody thought to ask was: Since all these d__n drugs do is “mask” or hide symptoms anyhow wouldn’t quitting SSRI’s be a lot easier than taking other crap? That could “re-mask” the original problem. No more mania. Wow.
Report comment
Doctors should be running these 13 blood tests before giving out antidepressants: http://www.optimallivingdynamics.com/blog/13-important-blood-tests-to-get-done-if-you-have-depression
Psychiatry is complete quackery.
Report comment
You’re preaching to the choir here, Jordan. 🙂
Report comment
you know what would really help a lot of “depressed” people with health problems? curing their health problems.
similarly…what would help a lot of “depressed” people with financial problems? money. low status? higher status. On and on it goes…
from what I understand, Francesca Simpson is correct. the data, such as it is, indicates a greater response in more severe depressive states. I think some critics have even called that into question, also.
Report comment
Good one. So anti-depressants, Zoloft/sertraline anyway, doesn’t work for depressants with chronic kidney disease, and, like, it’s supposed to work for people without kidney disease. You think?
Report comment
Maybe those suffering from chronic disease can’t derive much of a placebo effect?
Report comment
Maybe, but you’d better have your blood test, as suggested by an above blogger, and maybe also an HOD test, to make sure your depression isn’t also associated with a lot of perceptual distortions, so you don’t get sent through the roof by antidepressant therapy.
Report comment
“SSRI Ineffective at Treating Depression in Individuals with Chronic Kidney Disease” – say what?
Here’s a title for a more accurate and appropriate article: “SSRIs Effective in Causing Depression and Chronic Kidney Disease”
Report comment
My liver, kidneys, brain and every other bodily organ feel better now that that crap is out of my system! I escaped diabetes and have lost 35 pounds too.
I had a friend who was denied a kidney because she had a “bipolar” diagnosis. Sweet lady. Sickeningly ironic when you realize her “meds” destroyed her kidneys in the first place. 🙁
Report comment
Twenty per cent of those taking SSRIs will develop clinically significant AKATHISIA.
(38 or 39 of this group of 193).
This is the most dangerous of the multiplicity of serious ADRs caused by sertraline et al.
It is via akathisia that SSRIs induce self harm, violence and suicidality in all age groups treated.
Why is this not discussed in detail?
Even though these patients had the suffering of debilitating chronic kidney disease, they do not appear to have had any assessment of sexuality, sexual function or sexual expectations “baseline” before being exposed to the great risk of SSRI induced genital numbing, multifactorial sexual dysfunction and sexual failure (PSSD) – aggravating their suffering. (See RxISK PRIZE and latest MIA podcast).
Doctors are responsible for the adverse effects caused by the drugs which they prescribe, and have a professional duty of care to be aware of these toxicities.
Frequently, they are not aware, and/or they do not address, discuss with patients and/or recognise and correctly diagnose when they so commonly occur.
Even worse, toxicities including akathisia are misdiagnosed as “Serious Mental Illnesses” such as psychotic depression.
Hence the epidemic of SSRI induced, iatrogenic “pseudo-bipolar disorder” previously referred to.
TRM 123. Retired Consultant Physician.
Report comment
People with CKD are already being told they’re gonna die no matter what they do. Nephrology is a cult of hopelessness. How about actually treating the CKD with a more hopeful attitude? I have gone to kidney forums and found the same theme over and over. The people who stop going to the doctors and start using common sense live longer and feel much, much better.
Simple dietary changes will work wonders. I do not eat any salt, which means staying away from almost all processed foods and foregoing the restaurants and pizza, but I feel much better. I figured that one out entirely on my own without a doctor.
Report comment