Here is how it all started: the year was 1985, and Vincent Felitti, chief of preventive medicine at Kaiser Permanente in San Diego, was struggling to understand what was going on “with one memorable patient, a woman I’ll call Patty,” he said.
Patty was 28, and when Felitti first saw her, she weighed 409 pounds. A year earlier, Felitti had started a radical weight loss program at Kaiser Permanente. He was supervising about 300 obese patients a year as they stopped eating any food—all they consumed was five glasses of water a day plus a nutritional supplement called Optifast, which was manufactured by Sandoz. After 51 weeks on the diet, Patty’s weight went down to 132 pounds. She stayed there for about three weeks, but over the next three weeks, she suddenly regained 39 pounds.
“I was puzzled,” Felitti recalled in an interview, “and so was Patty.”
Then Patty told Felitti that she was a sleep walker who binged on food during her nocturnal wanderings. “She would get up and see all these open cans and boxes of food. She would also cook during the night,” he said. “So I asked her, ‘What do you think might be going on?’ She blurted out, ‘The men at work now say that I look attractive.’”
Felitti was still confused, and he asked Patty what those comments might have to do with her eating at night, which led to a startling confession. “She told me that she began overeating at 11, about a half a year after her grandfather began sexually abusing her.”
Thus was a hypothesis born: “Patty’s inability to keep the weight off made me realize that obesity, which was then viewed as a purely physiological process, might have psychological roots,” Felitti said. “For Patty, overeating appeared to be a coping mechanism—her way of covering up the intense pain and anxiety caused by abuse; it was her solution to a problem. It wasn’t a healthy solution, but it worked in its own way.”
The ACE Study
There have been few studies in medicine that have produced such compelling findings as the Adverse Childhood Experiences (ACE) study, which so convincingly describes how abuse, trauma, and other childhood difficulties exact a long-term psychological—and physical—toll. Yet, Felitti encountered significant resistance to his work early on, and despite the conceptual impact of the ACE study, the incorporation of the findings into public health policy is still in its beginning stages.
For Felitti, the light bulb that went off after Patti told him of the incestuous molestation was the start of a long scientific, and ultimately political, process.

Soon after Patti confided in him, Felitti and his colleagues at Kaiser Permanente in San Diego began to ask other obese patients about whether they also had a history of sexual abuse. “We were shocked. Of the first 286 patients we asked, 55% reported a history of abuse,” he said.
They knew that they were on to a scientific breakthrough about how childhood experiences played out in adult lives, yet Felitti found it difficult to get other doctors and health professionals to take his work seriously. In 1990, Felitti traveled to Atlanta to attend a national conference on obesity where he was eager to share his findings about Patty and his other patients in San Diego who were struggling with the long-term effects of sexual abuse.
“A physician gets up and attacks me,” Felitti recalled. “This guy tells me, ‘You need to understand that these statements about early abuse are fabrications. Your work is filled with lies. These patients are seeking social aggrandizement.’”
To this day, the ACE study has been criticized because of its reliance on retrospective reports. “But patients rarely make up stories about trauma,” he said. “This argument is just a common way of avoiding threatening information.”
That evening at a dinner for speakers, Felitti was seated next to David Williamson, a researcher at Atlanta’s Centers for Disease Control (CDC). Intrigued by Felitti’s ideas, Williamson told him that this work could be of enormous importance for the country, but that he would need to conduct a large epidemiological study in the general population. Thus was set in motion the twenty-year collaboration between Kaiser Permanente and the CDC on the ACE study.
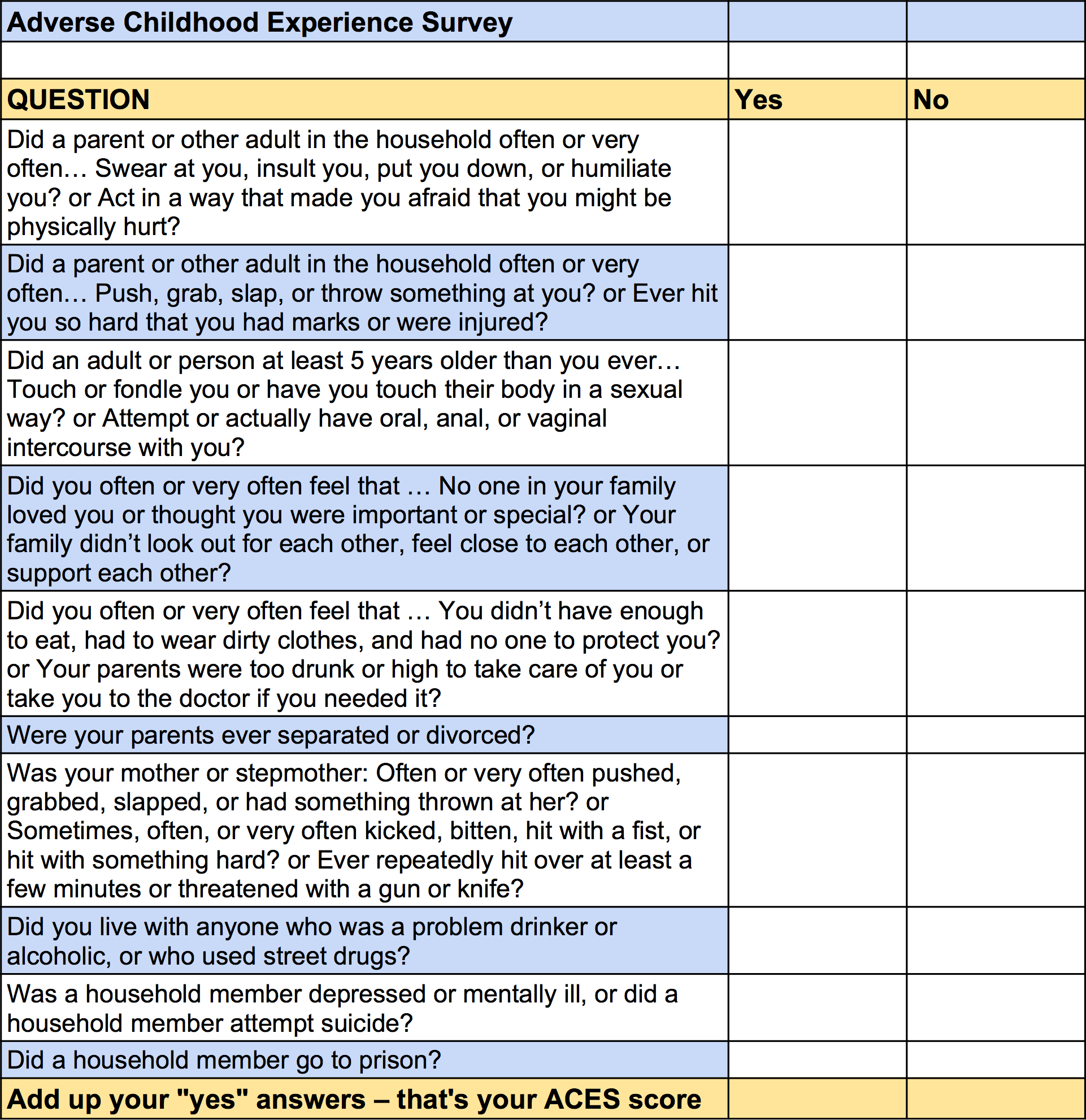
From 1992 to 1994, Felitti regularly interviewed patients to see what other early traumas they might have experienced besides sexual abuse. That’s when he came up with a list of the ten most common adverse child events, which in addition to sexual abuse include such experiences as physical abuse, parental alcoholism, and parental mental illness. He turned this list into a questionnaire, which he could use to conduct a formal study.
Although Felitti had access to a large sample of patients to survey—the thousands of adults who receive health risk appraisals at Kaiser Permanente—he had difficulty getting past the institutional review board (IRB) to do the testing. “In 1994, we battled the IRB for nine months. We were turned down at first. They told me, ‘You can’t allow these patients to decompensate by asking them all these questions about trauma.’ ”
His study finally got underway in 1995, and eventually would include asking 26,000 consecutive Kaiser Permanente patients, 17,000 of whom agreed to participate.
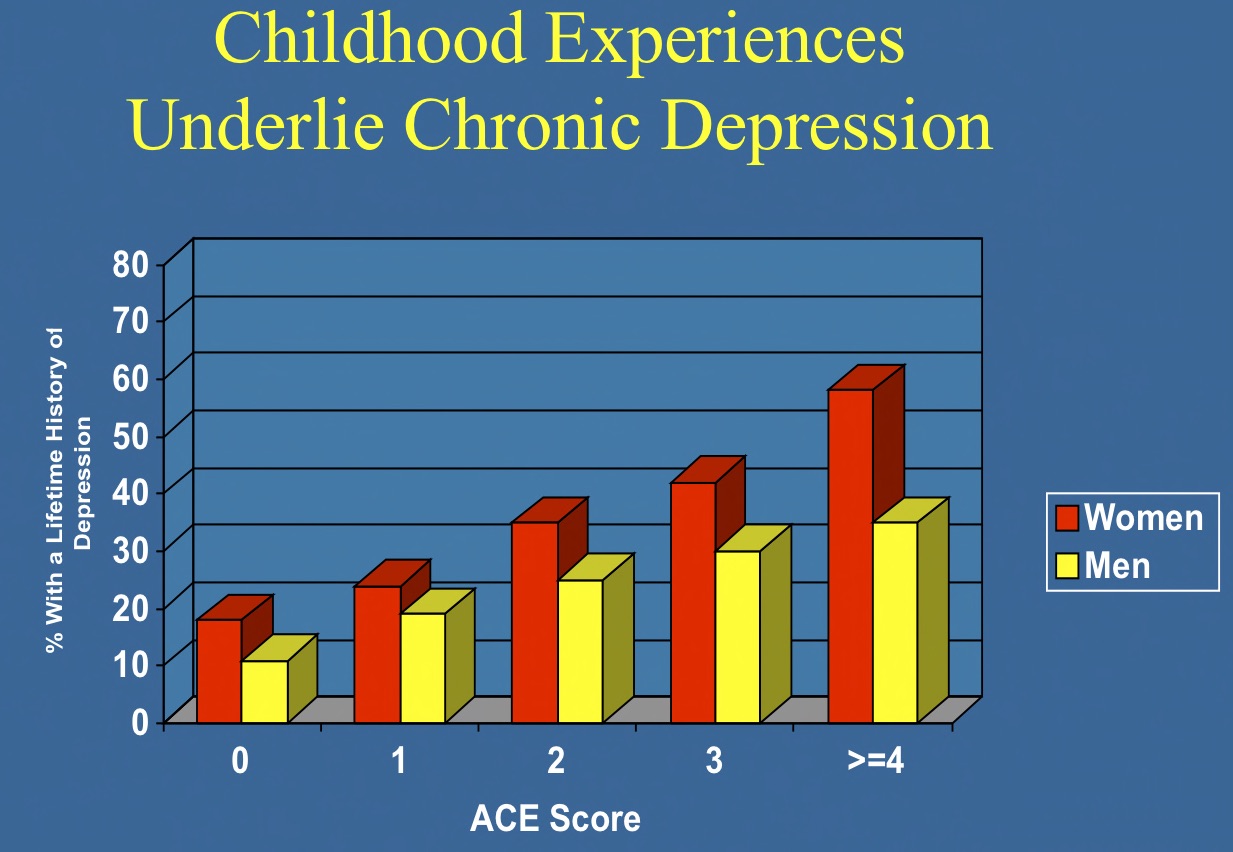
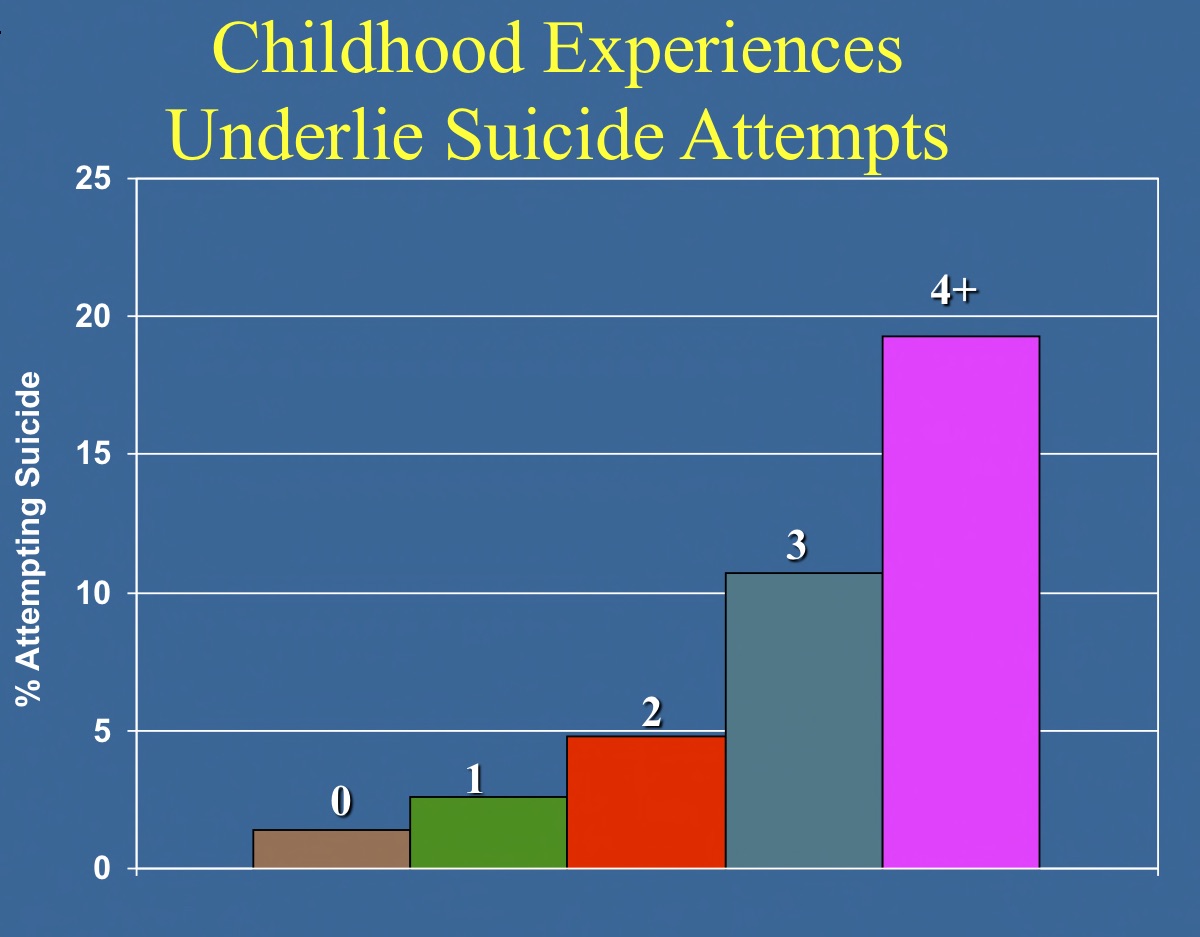
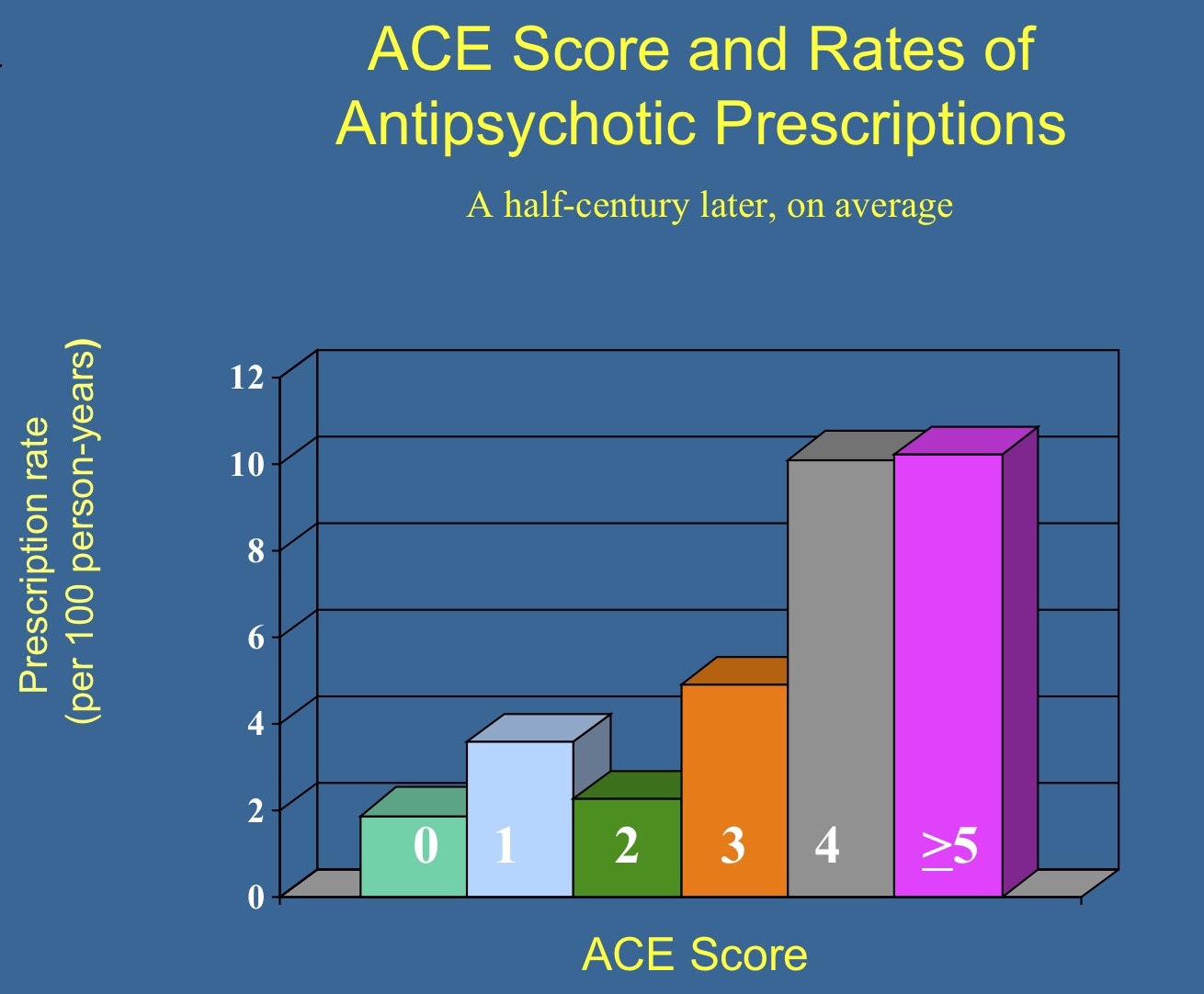
In his landmark 1998 article published in The American Journal of Preventive Medicine, which remains the most cited article in that journal’s history, Felitti and his collaborators at the CDC, such as Williamson and Rob Anda, linked ACEs to a host of mental and physical health problems. Among other key findings, they reported that adults with four or more ACEs, as opposed to those with none, were four times more likely to have had a depressive episode in the past year and twelve times more likely to have attempted suicide.
Indeed, the results told of how the risk of depression and other psychiatric struggles in adulthood rose in lockstep with the frequency of adverse child experiences.
Such data, tragically, foretold Patty’s fate, Felitti said. Patty eventually regained all of her weight, and then disappeared from the clinic for about twelve years. When she returned, she got bariatric surgery and lost 94 pounds, and soon became incapacitated by chronic depression. “My will is crumbling,” she told Felitti.
Patty eventually had five stays in psych hospitals, during which she underwent three courses of ECT. In the end, nothing seemed to help her, and she died a few years ago.
More Data and More Frustration
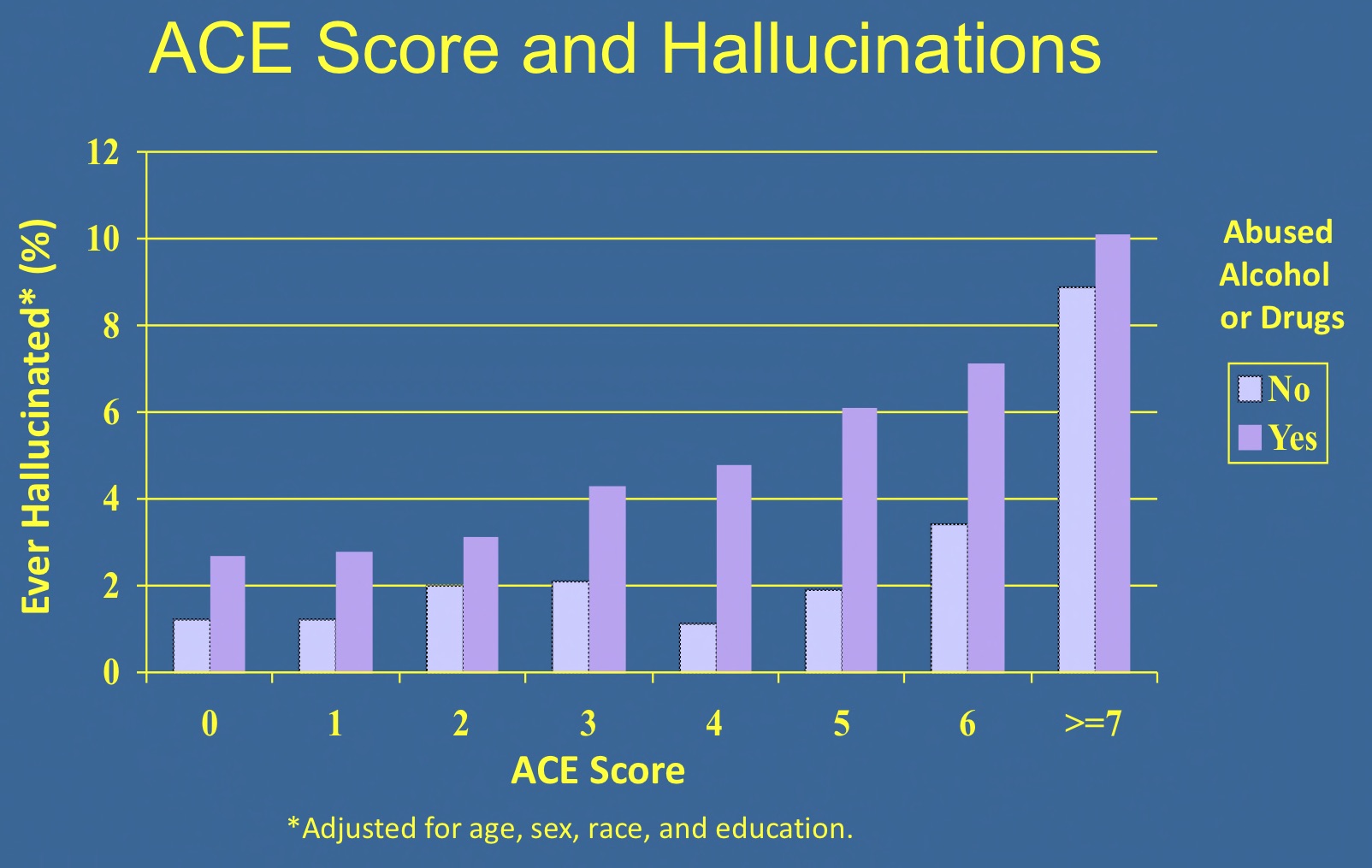
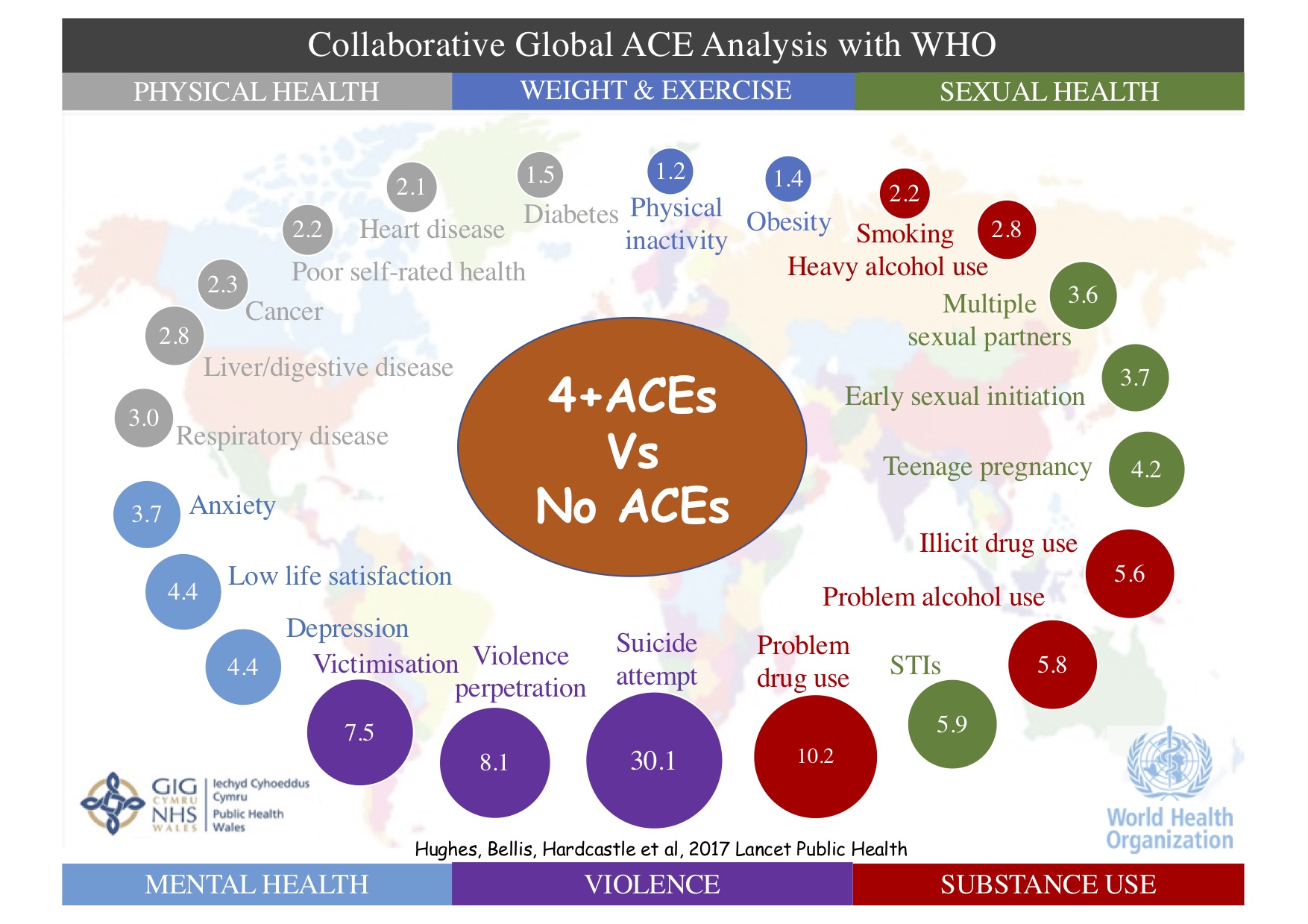
Over the past two decades, roughly 100 other scientific papers in leading medical journals have followed Felitti’s original paper. ACEs have now been shown to increase the risk of a wide range of health conditions besides depression and obesity—including alcoholism, cancer, diabetes, heart disease, respiratory disease, substance abuse and violence, according to a 2017 meta-analysis published in Lancet Public Health by a team of international researchers led by Britain’s Karen Hughes, which analyzed data on roughly a quarter of a million subjects across 37 studies.
However, even though the ACE results have become widely known, and lauded for their importance, the findings have not been incorporated into public health policy, or in medical care, in a robust way. As Hughes and her collaborators concluded, “despite accumulating knowledge about the lifelong effects of ACEs, their prevention and the development of resilience and support for those affected have been slow to move up political agendas.”
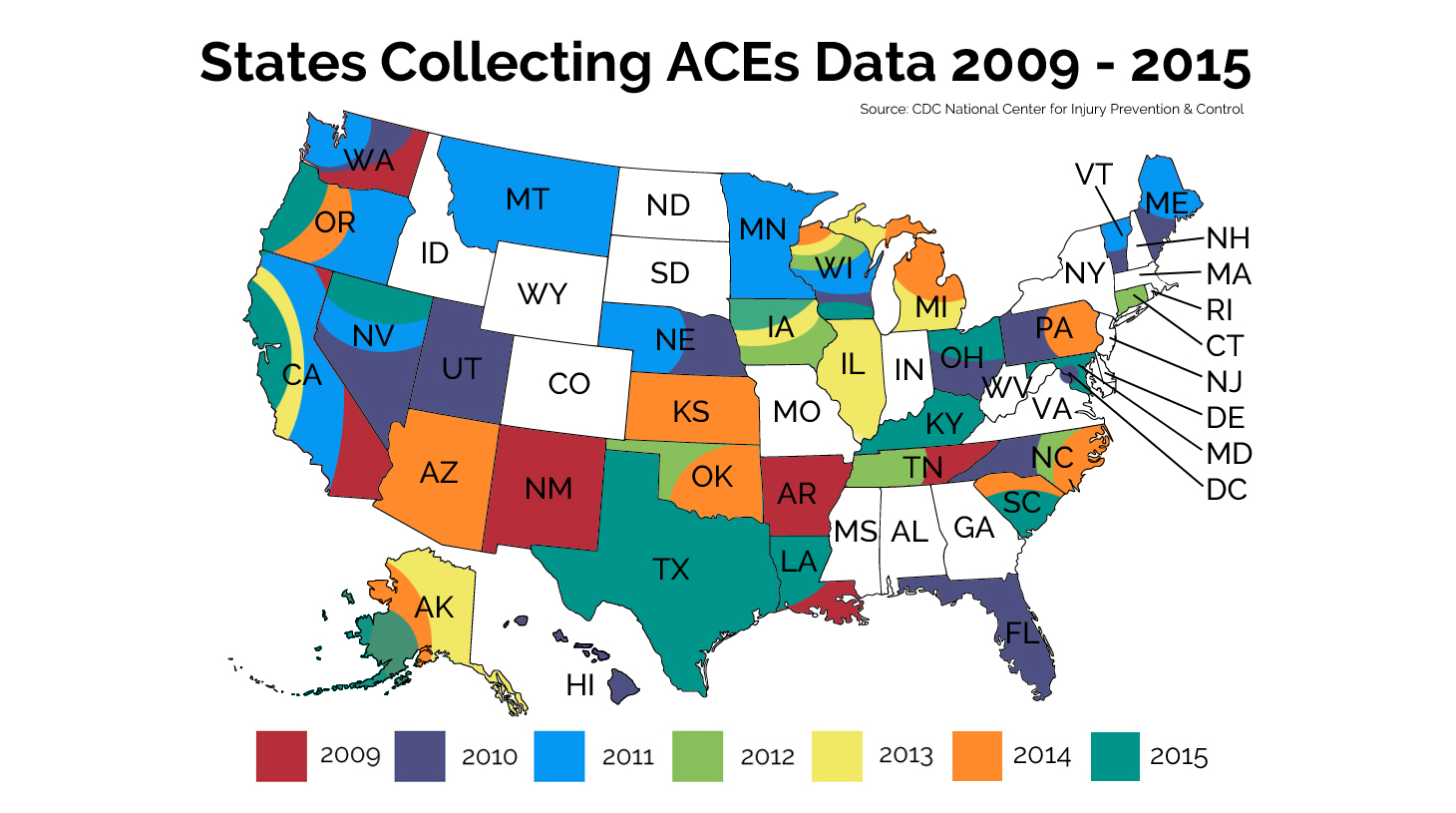
The ACE study led by Felitti was closed in 2015, and Felitti and his original collaborators at the CDC, including Williamson and Rob Anda, have all retired. However, a new generation of CDC researchers are still analyzing its 440,000 pages of barcoded data, and the CDC has integrated ACEs into its Behavioral Risk Factor Surveillance System (BRFSS), an annual, state-based survey that collects data from non-institutionalized U.S. adults regarding health conditions and risk factors. Since 2009, 42 states plus the District of Columbia have featured ACE questions for at least one year on their survey.
Felitti is still speaking around the world to try to get the word out, and even as more and more data are gathered, he shares the frustration voiced by Hughes and her collaborators. “Unfortunately, it’s been a big problem to get people to use the data, particularly physicians, where there remains a lot of resistance,” he said.
Felitti’s View of the Implications of the ACE Study
For Felitti, the ACE study reveals that early traumas pose a lifelong threat to both mental and physical health. “Traumatic stress affects a person’s neurobiology. And it does not typically go away on its own. Adults with ACEs are constantly being triggered. Their immune systems are weakened.”
This understanding, he said, demonstrates the need for a multi-pronged response from medical professionals and public health officials. There is a pressing need for increased investments in policies that will prevent child abuse and improve parenting skills, and this preventive effort needs to be combined with efforts to identify and treat patients at high risk for developing numerous debilitating health problems, physical and psychological, related to adverse childhood experiences.
Yet, turning that understanding into policy has proved quite difficult. Even though most health professionals in America are now familiar with the ACE study, few doctors in the United States screen for ACEs.
A first line of care that primary care physicians can provide, he said, is just to listen and implicitly accept patients’ stories. “It is the analogue of confession. A lot of patients feel a sense of relief when they can tell their doctor the worst story of their lives. Take the old lady who told me, ‘I thought I would die before I got to tell anyone about this.’ But many physicians don’t like asking about this stuff. They are embarrassed and they also worry that something may go wrong.”
Primary care doctors, of course, are not given much time to listen to their patients, and Felitti tells of numerous efforts to get physicians to ask about ACE that have failed. For example, about twenty years ago, Felitti contacted Erik Shinsecki, then the Chief of Staff of the US Army (and later the head of the Veterans Administration under President Obama). With Shinsecki’s help, Felitti set up a pilot program whereby incoming recruits at Ft. Hood would be screened for ACEs. “After two and a half months, it had to be stopped,” Felitti explained. “Drill instructors couldn’t handle the emotional reactions of all those recruits who would be found crying. And senior staff seemed to be worried about what would happen if the public knew that the U.S. Army is made up of vulnerable people.”
Even when people are screened and score high on the ACE questionnaire, there remains the problem of getting effective treatment, beyond the relief that may come from just telling their story to a physician. Felliti, for his part, has always been concerned about mental health services that typically treat patients like Patty with drugs and other biological treatments that fail to address the long-term effects of trauma. “Back when I was at Kaiser Permanente, I was afraid to send patients to psychiatrists,” he said.
He does believe that talk therapy can often be helpful, but with caveats. “Psychotherapy is an inefficient process, and it’s not affordable for many patients, as clinicians now charge up to $300 an hour and patients could easily go to hundreds of sessions.” Felitti recommends short-term treatments that focus explicitly on the precipitating traumas such as hypnotherapy, neurofeedback and eye movement desensitization and reprocessing (EMDR).
As he continues to speak about the ACE findings and its implications, Felitti finds that it is school systems and police departments, rather than health providers, that are most receptive to his ideas. “School officials and police officers appreciate what I have to say—about how a history of early trauma is often behind mental health problems and violent behavior.”
The political response to his work remains a mixed bag. “States are realizing that if they want to curb problems like opioid addiction and suicide, they are going to have to address ACEs, and that this might also help them save Medicaid dollars.” The intellectual interest may be there, he said, but state and local governments have rarely provided the funding needed to roll out concrete policy prescriptions.
The Next Generation of ACE Research
Alex Butchart, a psychologist who hails from South Africa and is now based in Geneva, is on a mission to bring ACE research to the rest of the world.
Since 2001, Butchart has been the coordinator of the Prevention of Violence Team (PVL) at the World Health Organization (WHO). After the WHO released its World Report on Violence and Health in 2002, Butchart became acutely aware of how a history of child maltreatment was an important risk factor for violence. He became interested in the ACE study because he wanted to develop research tools that could beef up the PVL’s evidence-based approach.

Butchart decided to develop a new instrument, which he calls the ACE-IQ (Adverse Childhood Experiences International Questionnaire). His goal was to initiate ACE research not just in other wealthy countries like the United States, but also in low- and middle-income countries. “The ACE-IQ is about one third as long as the questionnaire that is used in the United States,” he said. “And it adds a question about exposure to violence in the community, which is common in countries in those parts of the world where there is lots of conflict.”
The ACE-IQ was field tested between 2009 and 2011. “I am puzzled that the ACE-IQ has not received as much traction as we had hoped, though we have received about 20 to 30 requests for permission to use it,” he said.
However, the tide is slowly turning. Within the past year, studies using the ACE-IQ have linked ACEs to a host of mental and physical health problems in numerous countries, including Malawi, Saudi Arabia, China, Holland, Tunisia, Kenya, Lebanon and South Africa, with these reports published in leading journals.
Like Felitti, Butchart believes that ACE research should lead to a host of public health measures—both to prevent child maltreatment in the first place and to provide trauma-informed care for survivors. Such efforts would be cost-effective, he noted. Research by James Heckman, the Nobel Prize-winning economist at the University of Chicago, found that investments in early childhood development typically show a return of 7 to 10%. “But there is not much appetite for prevention—not just in the United States, but in the rest of the world, too,” he said.
With Butchart’s leadership, the WHO has rolled out INSPIRE: Seven strategies for ending violence against children. The seven strategies encompass Implementation and Enforcement of laws; Norms and Values; Safe environments; Parent and caregiver support; Income and economic strengthening; Response and support services; and Education and Life skills. “In low- and middle-income countries, there are limited resources, so prevention has to be the major emphasis,” he said.
In developed countries, he added, public health officials have the opportunity to be more ambitious. “Trauma-informed services can be a critical ingredient in several policy areas—such as social welfare, health, education and criminal justice.”
ACE research, Butchart noted, has demonstrated a clear link between early adversity and a wide variety of health and behavioral problems—such as various types of addiction, bullying, and delinquency. “Juvenile offenders are often punished, and we need more social services instead. We also need to change the way police are trained.”
Norway Turns to ACE-Based Health Care
Back in the mid-1980s, when Felitti was struggling with the mystery of what ailed Patty in San Diego, some 6000 miles away in Norway, Anna Luise Kirkengen was also stumbling upon the connection between a history of trauma and various medical ills.
Trained in medicine in her native Germany, Kirkengen moved to Norway where she set up shop as a general practitioner in the city of Oslo—at that time, the only female GP in her part of town. Soon 90% of her patients were women. “I began hearing repeated stories from women about being violated as children. And there was nothing about it in textbooks. It seemed like the past was still present in many of the medical complaints that my patients spoke about,” she said.
Kirkengen, who today teaches in the department of public health and nursing at the Norwegian University of Science and Technology in Trondheim, decided to go back to university to obtain her doctorate. Although she was not then aware of the ACE study, she was formulating similar conclusions. She turned her dissertation into the 2001 book, Inscribed Bodies: Health Impact of Child Sexual Abuse. Felitti reviewed the book a year later, and they have been close collaborators ever since. “His work is a mirror of my own philosophical reflections,” Kirkengen said.

For the past couple of decades, Kirkengen has fought to convince colleagues in the medical community about the scientific basis of her findings. “This knowledge is now seeping into public health and general medicine in Norway. There are now courses on the effects of childhood trauma for doctors enrolled in residency programs in family medicine. And by 2020, this training will be required for all doctors who want to work in family medicine for municipalities throughout Norway.”
Some family doctors in Norway, she said, have begun routinely referring their patients to mental health clinicians—psychologists, physiotherapists and body workers—who can help them address the long-terms effects of trauma. “Conditions like depression are inscribed into the body, and medication is ineffective. These patients need help reorganizing their way of being, and this is not done in psychiatry.”
Norway has a generous publicly-funded health insurance system, which typically covers most of the cost of these services. “This behavior is not yet mainstream among my primary care colleagues, but there is a growing awareness, and family doctors can play a key role in setting up these relationships with psychologists and physiotherapists,” she said.
Endre Sandvik is a family physician who has worked as the Director General of the Department of Health and Social Affairs for the city of Oslo since 2013. Last year, he became the project director of a program designed to turn Oslo into a trauma-informed city, which was initiated by the city’s vice-mayor for education and family services, Inga Marte Thorkildsen. “ACE research is the basis for this effort,” Sandvik said.
According to Sandvik, ACE research has three key components. It highlights how trauma can cause a host of behavioral and health problems; it explains how these negative effects are encoded into body through neurobiology; and it suggests that traumatized people can heal when they enter into safe relationships with those who can validate the pain of their overwhelming experiences.
The Oslo initiative will start by focusing on training teachers. Over the last three years, about $2 million has been approved for kindergartens, and by 2020, 22 of the city’s 171 schools will be covered. “We want to educate teachers—to change the way that they approach young people who have behavioral problems; right now, they are typically punished. An understanding of trauma can be extremely helpful, as these kids are often reacting normally to their own abnormal experiences.”
Sandvik is confident that these investments will ultimately lead to better mental health and higher graduation rates along with reductions in both crime and teenage pregnancy.
In May, Sandvik attended a WHO meeting in Copenhagen that aimed to launch a global network of trauma-informed cities. “In Europe, there is more emphasis on public health than in America, and this may be easier to implement. Our health policy is not as driven by drug companies,” he said. “However, we have a lot to learn from the excellent scientific studies conducted in the United States.”
California Rediscovers the ACE Study
Felitti is disappointed that Kaiser Permanente never made use of his ACE research during his decades of work there. “Before I left, a German data mining company looked at data on 135,000 patients. It found that asking about ACEs reduced outpatient visits by 35% and ER visits by 11%. I passed this information on to various regional medical directors at Kaiser, and there was no response.”
However, California has recently been rediscovering the ACE Study, thanks to the innovative work of the San Francisco-based pediatrician Nadine Burke Harris. Kaiser Permanente is also now circling back to the research that was launched under its auspices.
Harris is the founder of the Center for Youth Wellness in San Francisco, a health care organization that helps inner city kids. About a decade ago, Harris had an “aha moment” when she realized that the ACE study explained a lot of the health problems that she was seeing in her young patients. Harris wrote about her clinical work in the 2018 book, The Deepest Well: Healing the Long-Term Effects of Childhood Adversity.
Early this year, incoming Governor Gavin Newsom asked Harris to become the first Surgeon General of California. Soon after taking office, Harris released a statement declaring that one of her top priorities was to raise awareness about how adverse childhood experiences increase the risk of major health problems, noting that “the science is clear: early intervention improves outcomes.” Newsom’s 2019-2020 budget proposals include over $200 million in funds for developmental screenings and support for home-visiting initiatives to improve infant health.
Three years ago, pediatrician Mercie Digangi heard Harris give a talk about screening three-year-olds for ACEs. “It blew my mind,” she recalled, as she had been working for seven years in the Downey Medical Center near Los Angeles and yet had heard little about ACE while she was there. “I realized that the original ACE work came out of Kaiser Permanente in San Diego, and that we had not done anything with it for a while.”
It took Digangi two years to take action. Digangi began by arranging for ACE testing on three and five-year-olds at Downey. Within six months, the testing was also up and running in three other Kaiser Permanente medical centers in southern California. By the end of 2019, she hopes to have ACE testing in place at all fifteen Kaiser Permanente centers in southern California and to be testing three, five, ten and thirteen-year-olds.
Digangi is now working on helping the affected children find trauma-informed care in the community. “This will be a challenge. There is a lack of knowledge. While most psychologists and social workers understands how trauma affects children, I worry a lot about psychiatrists who might try to give these patients medication,” she said.
****
MIA Reports are supported, in part, by a grant from the Open Society Foundations





Thank you for this, Joshua, it’s so very important. I’ve been encouraged by Nadine Narris now having such an effective bully pulpit for getting this more on the policy table. And the work in Norway sounds wonderful.
One thing that I think is also important is the likelihood that ACE scores actually understate the connection between trauma and later effects, since there are many things from very early in life that people don’t remember or know about, and others that they probably just don’t mention because they’re in that semi-conscious zone we just don’t think or talk about. I think van der Kolk’s work on developmental trauma disorder is crucial here but it seems like that often does not make it into the ACEs discussion.
Report comment
I am happy to hear there is a return on investment.
Report comment
According to Georges Devereux, the trauma is not directly related to the severity of the adversity. It is related to the relationship between the severity of adversity and the size of the adapted cultural defenses. This is why children are more susceptible to trauma than adults because their cultural defenses are not sufficiently trained or strong. But anyone can succumb to trauma if their defenses are not culturally adapted to adversity. Quantity vs quality…
This relationship between adversity and cultural defenses is of paramount importance for understanding trauma. Psychosis is, basically, the creation of an idiosyncratic culture (beliefs, rituals, visions …) to face adversity. Psychotherapy is a way of dealing with the adversity one has experienced during childhood with the cultural defenses acquired in adulthood.
The research on ACE is actually not at all new, but it provides statistics and methodology adapted to the contemporary era.
Report comment
An ethical pastor confessed to me in 2011 that psychologists/psychiatrists covering up child abuse, for the religious leaders and their wealthy, is “the dirty little secret of the two original educated professions.” I did my due diligence, through many years of research, and did find that the psychologists have, in fact, been covering up child abuse for over a century.
https://www.indybay.org/newsitems/2019/01/23/18820633.php?fbclid=IwAR2-cgZPcEvbz7yFqMuUwneIuaqGleGiOzackY4N2sPeVXolwmEga5iKxdo
And with today’s psychiatric DSM “bible” theology dictating all “care” by all “mental health” workers, “the prevalence of childhood trauma exposure within borderline personality disorder patients has been evidenced to be as high as 92% (Yen et al., 2002). Within individuals diagnosed with psychotic or affective disorders, it reaches 82% (Larsson et al., 2012).”
https://www.madinamerica.com/2016/04/heal-for-life/
And absolutely you are correct, the psychiatric drugs do NOT help child abuse survivors, or their legitimately concerned parents. To the contrary the psychiatric drugs create the symptoms of the DSM disorders. The ADHD drugs and antidepressants create the “bipolar” symptoms. And the antipsychotics/neuroleptics create both the negative and positive symptoms of “schizophrenia,” via NIDS and anticholinergic toxidrome.
https://www.alternet.org/2010/04/are_prozac_and_other_psychiatric_drugs_causing_the_astonishing_rise_of_mental_illness_in_america/
https://en.wikipedia.org/wiki/Neuroleptic-induced_deficit_syndrome
https://en.wikipedia.org/wiki/Toxidrome
All this misdiagnosis of child abuse survivors is by DSM design. Because NO “mental health” worker today may EVER bill ANY insurance company for EVER helping ANY child abuse survivor EVER, unless they first misdiagnose them with one of the billable, but “invalid” and “unreliable,” DSM disorders.
https://www.psychologytoday.com/us/blog/your-child-does-not-have-bipolar-disorder/201402/dsm-5-and-child-neglect-and-abuse-1
https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2013/transforming-diagnosis.shtml
All this means that the primary actual societal function of both the psychological and psychiatric factions of the “mental health” system, both historically and today, has been, and still is, covering up child abuse. I personally do not believe it is wise to trust “mental health” industries, who have spent over a century profiteering off of covering up child abuse, to all of a sudden do a 100% flip and start helping child abuse survivors.
I believe our society should get rid of the child abuse covering up “mental health” industries, and these systemic child rape cover uppers should all probably be put in jail, since covering up child abuse is illegal. I believe our society needs to start arresting the child molesters. Today, when a mother tries to file a police report, because medical evidence of the abuse of her child was handed over. The police refuse to file a report, and tell her to go talk to a psychiatrist. I believe the religions, who employ our DSM “bible” believers, should also get out of the child abuse covering up business.
https://books.google.com/books?id=xI01AlxH1uAC&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=false
https://virtueonline.org/lutherans-elca-texas-catastrophe-coming-lesson-episcopalians
CPS also ignores real cases of child abuse, that happen outside the home, because they can’t steal the children from the home. I was able to scare a school, that had a pedophile on their school board, into closing its doors forever, once the medical evidence of the abuse was handed over, but I couldn’t get the pedophile arrested. I believe it’s time to put an end to “the dirty little secret of the two original educated professions’,” now multibillion dollar, primarily child abuse covering up, iatrogenic illness creating, scientific fraud based “mental health” system.
Especially since all this systemic child abuse covering up by our so called “mental health professionals” has also functioned to aid, abet, and empower the pedophiles and child sex traffickers. So our society now has pedophilia and child sex trafficking run amok problems, even according to world leaders, and the few ethical within the “mental health” industries.
https://globalfreedommovement.org/putin-blasts-euro-western-culture-of-pedophilia-and-satanism/
https://www.nytimes.com/2018/04/11/us/backpage-sex-trafficking.html
https://www.amazon.com/Pedophilia-Empire-11-Book-Series/dp/B077N6WNQS
I would like to point out that when a mother is able to get her abused child away from the child molesters fairly quickly. And she is able to keep the insane psychiatrists, who believe the way to help a child abuse survivor is to drug him, away. And she is able to keep the insane school social workers, who want to drug her child because he largely healed from the child abuse, and went from remedial reading in first grade, to getting 100% on his state standardized tests in eighth grade, away from her child.
Child abuse survivors can heal, and graduate from university with highest honors, Phi Beta Kappa, in addition to winning a psychology award. So our “mental health” workers, who don’t believe child abuse survivors can ever heal or need to be drugged, are incorrect. You should have heard all the psychology professors gush over how psychologically brilliant and well adjusted my child was at his graduation.
Loving mothers know how to help child abuse survivors heal. “Mental health” workers only know how to stigmatize, defame, silence, cover up, and drug child abuse survivors and their concerned family members.
Report comment
“Digangi is now working on helping the affected children find trauma-informed care in the community. ‘This will be a challenge. There is a lack of knowledge. While most psychologists and social workers understand how trauma affects children, I worry a lot about psychiatrists who might try to give these patients medication,’ she said.”
All “mental health” workers worship from the same, by design, can’t bill for helping child abuse survivors, DSM billing code “bible.” So NO “mental health” workers, not the psychologists, not the social workers, not the psychiatrists, not the counselors – NONE of those who utilize the DSM billing codes for reimbursement, can bill to help child abuse survivors. It’s a systemic problem with the DSM.
I do work with under privileged children, at least one of whom I’m certain was abused, but all are considered “at risk.” And I can say, non-medical, non-stigmatizing art therapy can help abused children heal. And not just learn to trust in people again, but also develop the creative side of their brain, which is the side of the brain which allows people to see the big picture.
It’s been really rather cool to watch a bunch of children, who started out wanting to copy my samples, turn into a bunch of truly unique and amazingly creative, creators. Perhaps the child abuse survivors should be handed over to the artists instead?
Report comment
Since the artists, unlike all the DSM believing “mental health” workers, don’t necessarily want to profiteer off of covering up what happened to child abuse survivors.
Artists want to help child abuse survivors work through what happened to them, help them heal, and grow spiritually and emotionally, by allowing them to get the evil that happened to them out, in a non-violent manner.
And “the truth will set you free.” All our DSM believing “mental health professionals” are about covering up the truth that child abuse happens. Despite the reality that child abuse is a serious – to the point of now being called a pandemic – societal problem.
Report comment
Okay, glad to see the research and discussion but again we have layers of concern. If one lives in substandard housing and one lives in fear of shootings by all aspects of society how can a child really learn? This is over and above the components of life in the ACE study.
Also ACE is really an inter generational nexus. It ain’t just the patient in the office, the child acting out in school, the father in jail, the substance addicted helping professional in all areas, the clergy, the legal professionals who have chosen greed over ethics, it is all of us.
Until we see humanity as in great distress as the environment and earth crisis without resolution will continue.
We all have different weaknesses and strengths and so many folks need to wake up- the canaries are in trouble.
Report comment
I understand that the physicians doing this research have the best of intentions, and that they believe the data they are generating will be used for good purposes, or that is at least their hope. But that Pollyanna viewpoint is at odds with the actual reality of health “care,” at least here in the US. In Scandinavian countries, there is a much bigger sense of communal responsibility, not the toxic individualism of the US. The cultural response to this tidbit, for instance, is vastly different:
“After the WHO released its World Report on Violence and Health in 2002, Butchart became acutely aware of how a history of child maltreatment was an important risk factor for violence.”
Unlike Scandinavia, the US is more likely to use this info against the adult survivors of child abuse. Reveal that you were routinely subjected to “maltreatment” (isn’t that a nice, safe word?) as a child, and you will be forever branded as someone the community must be protected from. Our social policies are not driven by compassion, or a sense of responsibility for one another; no, they are driven by fear and control, and that situation is only getting intensified. The fact the CDC named their survey the Behavioral Risk Factor Surveillance System (BRFSS) is chilling. So that’s on the societal level.
On the personal level, when somebody asks you these ACE questions, do your own risk assessment. Ask yourself: why do they want to know this about me? Is it in my best interest to disclose? or to lie? or to refuse to answer? ?How will divulging this information effect the health care I will receive?
When Patty (the patient in the article) made the connection between the molestation and her weight gain, what did disclosing that info get her? Psychiatry, of course! I daresay she’d have been MUCH better off if she’d kept that revelation to herself in that moment. She could have used it to understand herself better, to find healthy ways of feeling safe in her own body. A course in self-defense, perhaps.
Report comment
This is really an excellent comment for two reasons: it articulately addresses Psychiatry’s advocacy of Pollyanna and how the community re-abuses those who have experienced childhood trauma. Psychiatry advocates Pollyanna in a fairy tale world of goodness. Psychiatry falsely implies that Adverse Childhood Experiences are an anomaly in a world of fairness and altruism wherein cruelty and social and economic injustice are successfully redressed through established social structures. Psychiatry denies the reality of trauma; it is an experience of a distressful environment rather than a distressful experience in an otherwise friendly environment. Also, I read an article at this website that described how adults who were “diagnosed” with Adverse Childhood Experiences were considered risky candidates for adoption; the cruelty and injustice are staggering.
Report comment
Our social policies are not driven by compassion, or a sense of responsibility for one another; no, they are driven by fear and control, and that situation is only getting intensified.
Absolutely — because psychiatry is a branch of law enforcement, not medicine or “social services.”
When the Murphy Bill was on the table — dressed in all sorts of concern for the well-being of the “mentally ill” — Murphy kept a photo of the Sandy Hook victims on his desk to remind him of what this is really all about, i.e. protecting society from US. (Rather than U.S.)
P.S. Being a stickler for semantics I would add that these are not “our” social policies unless you identify with the ruling class; these are their social policies.
I knew you’d appreciate that. 🙂
Report comment
The CT Attorney General, in refusing to release to the public the final full report on “Sandy Hook”, stated that to do so would “cause people to stop taking their meds”…. And the alleged shooter, “Adam Lanza”, *WAS* a victim of both psychiatry, AND psych drugs. As ALL the mass-casualty school shooters were/are….
Go ahead, I DARE you to find even one who wasn’t….
It’s NOT the guns that kill, rather it’s psychiatry and psych drugs which pulls the triggers….
Report comment
Psychiatry is the only branch of accepted medicine to regularly demonize its “patients.”
You won’t find cardiologists going on 60 Minutes to terrify the public with tales of all those monsters with heart disease who should be locked up and subjected to cruel, pointless experiments to protect the public.
I know pro psychiatry friends who got angry at Murphy for maligning them. Basically called them murderers.
Report comment
olhead said: “P.S. Being a stickler for semantics I would add that these are not “our” social policies unless you identify with the ruling class; these are their social policies.”
I DO appreciate that! Thank you for woke-ing my vocab! Lemme just fix that wording: should’ve been “America’s policies…” rather than “our policies…” because frankly, I cannot in good conscience claim as my own this country that America has become. And the thing about eschewing the elitism, too. 🙂
you do get me, buddy.
Report comment
thanks for this joshua….
there may be another problem when obesity
is present…how about leptin resistance causing
some of the problem….with weight gain…
Report comment
ah yes, psychiatry, the state’s way of hiding the causes of mental distress.
Kaiser Permanente, a private insurance company with zero interest in preventative medicine. They are trying to take over the UK NHS which is crumbling as a result.
Report comment
You mean people have reasons for their problems? That can not be! http://www.collectmedicalantiques.com/sites/default/files/gallery-images/robertburger-villingenplastometerneedhighresberlinphrenologist.1410027341.jpg
Report comment
Absolutely, there are NO real life reasons for peoples’ distress. Child abuse NEVER happens, according to our “mental health” workers, who have set up their DSM “bible” such that they may NEVER bill to help ANY child abuse survivor EVER.
And our DSM deluded believe that, “all distress is caused by ‘chemical imbalances’ in people’s brains, that the doctors can cure with the psych drugs.” Despite this “invalid” theology being debunked by science decades ago.
What a totally insane world in which we live. God save the decent, and judge the insane people fairly, for “they know not what they do.” And the DSM “bible” believers are a bunch of insanely deluded, wrongly given “omnipotent moral busy body” status, fraud based, money only worshipping lunatics.
Report comment
Schizophrenia Bulletin 38(4):661-71 · March 2012 Childhood Adversities Increase the Risk of Psychosis: A Meta-analysis of Patient-Control, Prospective- and Cross-sectional Cohort Studies https://www.researchgate.net/publication/223990226_Childhood_Adversities_Increase_the_Risk_of_Psychosis_A_Meta-analysis_of_Patient-Control_Prospective-_and_Cross-sectional_Cohort_Studies
Schizophrenia Research Available online 22 May 2019 Linking Childhood Adversities with schizophrenia: A mediating role of the balanced time perspective
Report comment
Now the cause of “mental distress” has always been Snidely Whiplash, but is your “mental health treatment professional” really Dudley Doright? I’ve got a lot of serious doubts on the subject as far as that goes.
Report comment
Nope. The Mental Illness Guy is actually Snidely Whiplash disguised as Dudley Do-Right.
Report comment
Groomed for success versus mussed for failure? This train ain’t goin’ nowhere! Adverse Childhood Experiences ACEs leading to Adverse Adulthood Experiences AAEs? I tend to see both developments as a dimension of farce, that is, change the play, and you will get a different result. Stage a tragedy, in the life-game, and the results are going to be tragic. What is that statement attributed, falsely, I believe, to Albert Einstein? Oh, yeah. The definition of insanity is doing the same thing over and over again and expecting different results. If adverse experiences are leading to more adverse experiences, maybe something is missing. Maybe something like pleasant experiences.
https://www.history.com/news/here-are-6-things-albert-einstein-never-said
Report comment
“and this preventive effort needs to be combined with efforts to identify and treat patients at high risk for developing numerous debilitating health problems, physical and psychological, related to adverse childhood experiences.”
And what of the dilemma of psychiatric/”mental health” treatment being an ACE itself? Forced drugging, adverse drug reactions, being segregated and stigmatized and treated differently than other children, being bullied as a result and it being blamed on you, being sent to special schools, being drugged more and more as you naturally resist, developing permanent involuntary movement disorders, being taken away from your parents for refusing to keep drugging you, on and on it goes, eventually becoming a disabled adult on SSI, trapped under that same psychiatric system, hiding the best you can, trying to slip through the cracks while still receiving your monthly pittance.
But I imagine that will never be considered an ACE. It would just be way too awkward, now wouldn’t it?
Report comment
I’d love to see the ACE questionnaire include trauma that happened in adulthood. I just got off the phone with someone who had been seeking help for his depression and he clearly identified a trauma in adulthood that was the beginning of his struggles with depression
Report comment
Yeah, but we don’t want this to turn into a justification for Therapy, Recovery, or Healing.
It has to be penalties for perpetrators, and reparations for survivors.
Report comment
I’d love to see the ACE questionnaire include trauma that happened in adulthood. I just got off the phone with someone who had been seeking help for his depression and he clearly identified a trauma in adulthood that was the beginning of his struggles with depression
Report comment