The second in a series of blogs presenting a philosophical analysis of the modern mental health system and what it is concerned with.
 There are two broad approaches to the ‘mental’ that Wittgenstein’s ideas challenge. One is that all our feelings, thoughts and behaviours are caused by, or ‘epiphenomena’ of, a specific brain state or process. This is sometimes referred to as ‘physicalism’ (‘epiphenomenalism’ being one variant of physicalism). On this view — the one that much neuroscience is based on — the brain states that lie behind the sensations and behaviours are what is primary and important. Just as to accurately understand the behaviour of water we need to know its molecular structure, to understand human behaviour we need to identify the brain states that produce it.
There are two broad approaches to the ‘mental’ that Wittgenstein’s ideas challenge. One is that all our feelings, thoughts and behaviours are caused by, or ‘epiphenomena’ of, a specific brain state or process. This is sometimes referred to as ‘physicalism’ (‘epiphenomenalism’ being one variant of physicalism). On this view — the one that much neuroscience is based on — the brain states that lie behind the sensations and behaviours are what is primary and important. Just as to accurately understand the behaviour of water we need to know its molecular structure, to understand human behaviour we need to identify the brain states that produce it.
The second approach to understanding human experience is the ‘psychological’. By this I mean the idea that mental events and behaviour can be studied and theorised in their own right, without reference either to the brain or to the individual that has them. According to this view mental states have independent characteristics that can be categorised, compared and experimentally manipulated just like material things in the world, such as minerals or plants.
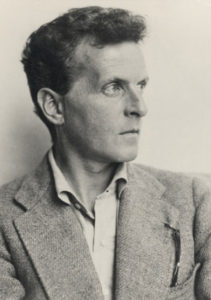
Although Wittgenstein did not deny that we have personal experiences, for example pain or sadness or guilt, some of which we refer to as mental or psychological states, what he pointed out is that we understand these experiences through the way we express them. We express ourselves through words, gestures and actions, and all of these derive their meaning through the way they are used in a public and social context.
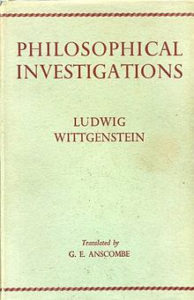 In Philosophical Investigations Wittgenstein gives the example of pain. Although pain is a personal or subjective experience, we express pain through well-recognised responses, which are both automatic or involuntary (recoiling from the painful stimulus, crying out) and voluntary (begging someone to stop doing whatever it is that hurts). These behaviours and utterances are recognised as manifestations of pain by other people when they occur in particular circumstances (such as someone falling over or stubbing their toe). If someone is screaming but no painful stimulus is apparent, we might doubt whether their behaviour is a manifestation of pain, even if they claim it is.
In Philosophical Investigations Wittgenstein gives the example of pain. Although pain is a personal or subjective experience, we express pain through well-recognised responses, which are both automatic or involuntary (recoiling from the painful stimulus, crying out) and voluntary (begging someone to stop doing whatever it is that hurts). These behaviours and utterances are recognised as manifestations of pain by other people when they occur in particular circumstances (such as someone falling over or stubbing their toe). If someone is screaming but no painful stimulus is apparent, we might doubt whether their behaviour is a manifestation of pain, even if they claim it is.
Think of a young child who learns that expressing pain will bring love and attention from a grown-up! The point is that it is the public manifestations of pain and their particular context that constitute our immediate, ordinary understanding of pain, not the ‘internal’ or personal experience of it and not whatever it is that goes on in the painful area or in the brain or nervous system. The meaning of pain is how we use the word in everyday language1.
We can, however, investigate the neural basis of pain, and the local bodily processes that produce it. This is a perfectly legitimate activity but it does not reveal the meaning of pain. It reveals the bodily basis of pain, but not how we understand the phenomena of pain in everyday life.
The Wittgenstinian philosopher Peter Hacker has described how emotions and moods are also understood through particular public expressions, which form the criteria for ascribing an emotional state to someone2. Some emotions are demonstrated by an immediate reaction, like a smile or expression of surprise, and some, like sadness, grief or anxiety, by longer lasting patterns of behaviour. Implicit in most emotion language is the idea that the feeling is a reaction to someone or something. Love, hate and anger often have as their object another living being. Surprise and delight are usually immediate reactions to proximate events. Sadness, fear, guilt, shame and happiness are less immediate reactions, but also normally understood as responses to something that has happened, is happening or might happen to someone. Part of the context of emotion language is the object or events at which the emotion is directed.
We recognise sadness when someone tells us they are sad, when someone looks sad, and behaves in a sad way, and usually this involves explaining what made them sad. These things are necessary for us to understand and accept that someone is sad. If someone says they are sad, but has a big smile on their face, and proceeds to laugh and act in a lively and cheerful manner, we would not understand their claim to be sad. Similarly, if someone says they are sad, but can’t explain why, we would not necessarily disbelieve them, but we would find their assertion more difficult to accept than if they told us they were sad because their cat had been run over.
As Rom Harré (another philosopher much influenced by Wittgenstein) has pointed out, emotions are different from physiological responses like pain or hunger, which are primarily experienced in the body. Emotions may be associated with particular bodily sensations, but they are not reducible to these sensations3. Therefore, unlike pain, it is not clear that emotions have specific physical correlates. In fact evidence suggests they do not. Several different types of emotion; fear, anxiety, anger and euphoria, for example, are associated with the physiological state of arousal that is linked with the release of chemicals like adrenalin and noradrenalin (sometimes referred to as the ‘fight or flight’ response). This physiological state and its biochemical characteristics are not specific to a particular emotion, therefore, but cut across several types of emotional response.
Even if we did find a specific brain state that correlated perfectly with the experience of fear, and another one that was present every time anyone felt joy or pity, the brain states are not what we understand as emotion in everyday life. It is not brains that feel fear, pity and joy, it is people. Emotions are attributes of people living and acting within a social or public world.
So what does all this mean for the study of the ‘mental’ realm, including the situations we refer to as ‘mental disorders.’ It means that we understand them through the public expressions by which they are manifested. This is what our language of mental states and emotions refers to. It refers to the publicly available voluntary and involuntary actions of whole living persons who are actively engaged in the social and material world.
Take depression for example, or prolonged sadness or melancholy or despondency (the term depression has become so strongly associated now with the psychiatric approach, it is sometimes better to use other words to clarify what we mean when we think about this sort of emotional state). There are various patterns of behaviour we might associate with this emotion as broadly conceived. Someone might take to bed and cease to go about their everyday life. Someone might be crying a lot and displaying obvious signs of distress. Someone might become preoccupied with a negative and pessimistic view of the world. Usually, use of such terms implies a change: that someone was previously acting normally, and then starts acting in a depressed manner.
The important point is that the sorts of behaviours we associate with depression are not signs or symptoms of an underlying brain disease or mental construct that is what depression really is. When we refer to someone as ‘depressed’, even when we do this as psychiatrists in the framework of diagnostic systems like the Diagnostic and Statistical Manual (the DSM), we are not identifying the real nature of their nervous system or mental make-up. We are referring to the sorts of behaviours4 they are displaying, and how we normally interpret these. Depression is just the behaviours that we understand as expressing depression.
The ethnomethodologist Jeff Coulter has written about the characteristics of the expression of psychosis or madness. Coulter explains that madness is attributed when someone acts in a way that is not easily understandable, and breaks unwritten rules of social conduct such as behaving unpredictably, or failing to undertake expected tasks. Following Wittgenstein, Coulter stresses that madness, like other mental states, is recognised and attributed by the community in response to public patterns of behaviour, and is not something hidden that can only be detected by experts 5.
So the important point that Wittgenstein makes is that mental states, including mental disorders like depression or psychosis, are not just, or primarily, private events — whether these are considered as brain events or events in an abstract mind. We recognise and identify these situations through the sorts of behaviours and reactions that people display publicly, and the context in which these occur. Neither brains nor minds are depressed, anxious or psychotic — real people are, in real social situations!
Studying mental disorders as if they are conditions of individual minds or brains therefore misses the point of them. We need to understand them at the social level, as problems that show up in social groups or contexts. Yet our current mental health services are set up to adjust individual brains or minds, as if this could fix the problem. But the problem lies in the interaction of a person’s behaviour with their social environment, which includes the social expectations of how people should behave.
This suggests that sometimes it may be the environment that needs fixing, rather than the individual. Take the example of so-called ‘Attention Deficit Hyperactivity Disorder’. Many people have pointed out that instead of adjusting individual children’s behaviour through brain-modifying chemicals, we should devise an education system that accommodates a wider range of developmental trajectories; one that is better able to cope with children who need more physical activity and stimulation than the average child of their age 6.
Other ‘mental disorders’ also act as barometers that reveal the strains and tensions of our social institutions. If we recognised this, we might be able to imagine other ways to organise society that might render ‘mental disorders’ less prevalent or less problematic.















With depression is the cause more of breakdown of bodily system (such as endocrine) that the central nervous system needs to communicate with brain as opposed to serotonin being prevented from going to brain? (AR database)
With above said are the depression medications actually working with neurotransmitters the way needed? I think no actually.
Medicines work better for schizophrenia in more cases then they do for depression.
This is because the medicine is targeting correct function sometimes in schizophrenia but not really that much with depression.
With having schizophrenia it targets neurotransmitters in effective way thus alleviates pain but not cure.
Report comment
thus alleviates pain but not cure
This is exactly what one would expect from taking a tranquilizer. Anyone who takes an “antipsychotic” is going to get tranquilized, because “antipsychotics” are tranquilizers. It has nothing to do with “the medicine […] targeting correct function sometimes in schizophrenia.”
Report comment
ALSO the human heart is equal in the blame for mental states.
The different systems in body play on one another and this is true for the brain as well. I think the author is going to great depths when referring to mental states to explain the opposite of what I just mentioned.
Report comment
Some guys stop at the bar every evening to go on a bender. Why? The alcohol numbs their pain. Apparently they have an alcohol deficiency in their brains. Lol.
Report comment
This seems off the topic of the blog. The question at hand is whether psychological phenomena are the consequence of brain activity, or independent phenomena that can be studied or acted upon independent of the brain. You seem to be saying you accept the former. However, I wonder if you are recognizing the fact that both positions are philosophical, not scientific, positions. As I think has been stated multiple times directly to you, there is no actual evidence that any of these “mental disorders” have a consistent biological cause or treatment. So depression may SOMETIMES be the result of a bodily system breakdown or even of “low serotonin” in specific cases, but there is no GENERAL condition that “causes depression,” because “depression” is not a thing that can be caused, it’s a natural body reaction that is caused by many different potential things. The idea that “depression” is a specific state that is always caused by the same thing and requires the same “treatment” is exactly the concept that has led psychiatry down the false path it currently follows.
Report comment
My points talked about how causes are many and varied. That is obvious to a child. It’s like conventional wisdom.
Sometimes you can love it away. Sometimes you can therapy it away. And sometimes if you need to you can try medication.
Report comment
No argument from me on those points. Though it is indeed obvious to a child, I have unfortunately found many “mental health professionals” to whom this appears to be a foreign concept.
Report comment
It remains foreign to them because accepting it would threaten their careers in the Mental Illness Factory.
Report comment
That’s thev way it’s done for those of you in reality and not operating on fringes of mad in America.
To win a debate with folks here you hardly ever justify your points with what you actually do. They use that as excuse to laugh in your face. Also it diminishes how hard you worked to be where you are at now.
Report comment
It is unfortunate that you seem incapable of a civil conversation, Pat. Why do you insist on insulting posters just because they express a point of view you don’t agree with? Is it just possible that other people had different experiences with the MH system than you have?
Report comment
Pat, your own arguments are generally far from coherent. They can’t convince anyone if they’re indecipherable.
I take it you’re “meds compliant.” The things you post validate those of us who went off our drugs. I won’t argue that they make you feel good; only you can judge that.
As far as winning a debate, you might score points as a poster child for NAMI. However, speaking, reasoning and other skills are irrelevant in that situation.
Just stand at the podium and shout, “Lithium saved my life!” Or “I found Salvation in a bottle of Prozac!” Or “Thank you, Abilify, for saving my soul!” Then try to smile if the drugs haven’t stolen that from you.
No one in NAMI will challenge these statements. They welcome dissenting points of view less than MIA does. If anyone asked how you could scientifically prove Zoloft saved your soul (real science you know) the sheeple would run around bleating and the NAMI mommies would arrange to have the heretic tarred and feathered. 🙂
Report comment
Because it gives me something to do.
Also because I’ve been talking the the people you call your friends and it seems that me there’s means to an end. They don’t care anymore. What you say.
Report comment
Pat, so you admit you just like screwing with people? Essentially, admitting you’re trolling? On that basis, I’d suggest that no one should respond to you ever, as you are clearly not serious about establishing the truth of the situation. I will begin applying the policy of “ignore the troll” starting immediately.
Report comment
“But the problem lies in the interaction of a person’s behaviour with their social environment, which includes the social expectations of how people should behave.”
But psychiatrists do that, that is why they feel justified in drugging people..to shut them down. They do not care a jot if they gave them akathisia – toxic psychosis – that maywell have casued the violence, behavioural discontrol in the first place. But if wrong, sorry if I misunderstood you there…. please don’t have someone come round and pump risperidone in me 😉
“This suggests that sometimes it may be the environment that needs fixing”
Yes ofcourse, neoliberal globalism, and the psychotic financial system of banksters: fractional reserve banking, quantitative easing, derivatives like credit default swaps and collateralized debt obligations. In other words a monumental screw-over of the public. Jim Rickard’s of the CIA is trying to do something about it, but he is on the right of…. well, the right, although he may not agree. He sees the collapse of the $ and then a gold backed $ at $5000 an ounce probably much more, which will be a disaster on the scale of the great depression: hyperinflation , but he wants that to get rid of Wall street..take out the banksters, screwing everyone over with made up funny money.
https://twitter.com/JamesGRickards/status/909263132543131648
Report comment
I definately agree, the way society is structured needs to change. And since about 90% of those labeled with today’s serious “mental illnesses” are actually legitimately distressed child abuse victims; I’m quite certain a return to arresting the pedophiles, as opposed to continuing to turn millions of child abuse victims into the “mentally ill” with the psychiatric drugs, would be an excellent start.
But rumor on the internet is that our world is controlled by “luciferian pedophiles.” And ending the mislabeling of child abuse victims as the “mentally ill” would decrease psychiatry’s business by 90%, so most of the psychiatrists don’t want to stop profiteering off of covering up child abuse en mass, despite this actually being technically illegal in the US.
Report comment
A person can, without any sort of brain change or abnormality, think him or herself into a corner, yes.
It is social interactions, public events, that get people into therapy, and so in that sense, Ludwig Wittgenstein is correct. People don’t enter into therapy because their behaviors are seen as consistent with the “norm”. No state of mind is a problem in itself, it only becomes a problem when it interferes with the ordinary course of life events.
Did the corner that this person or that thought him or herself into register in a discernible way in the social realm, this person or that becomes a prime candidate for therapy.
Paul-Michel Foucault made the case in his first book, Mental Illness and Psychology (1954, rev. 1962), that without madness, without inexplicable behaviors, psychology would have little raison d’etre. Given irrational behaviors and acts, you’ve got psychology there, the study of people’s motivations, delving into this great enigma, the reason for the unreasonable in human behavior, and, frankly, there doesn’t have to be a reason. Your blog entry is a case in point. What are we primarily looking at here if not the behaviors of people that somebody finds wanting or disturbing? Doing so certainly doesn’t offer any sort of explanations for the behaviors of most men and women.
Report comment
It is none of anyone business what others behaviours are.
Again involuntary and voluntary seeking help is overlooked.
Peoples sins are their own. If people choose to be depressed ( old sin of sloth) that is there choice. https://en.wikipedia.org/wiki/Seven_deadly_sins
Today gluttony is fast becoming a true medical condition. http://www.cbc.ca/news/health/health-hospital-obesity-bariatric-michaelgarronhospital-uofalberta-1.4305767
addiction to food http://www.cbc.ca/listen/shows/white-coat-black-art/episode/13982189
People go to a medical doctor for problems with their sins, the Fing doctor can’t tell them the truth.
Report comment
“Involuntary” “seeking help”? Some people don’t ‘seek help’, and the state with its psychiatry would ‘intervene’ nonetheless.
Sin is a religious term, and, therefore, N/A. You’re dialoguing with an atheist here.
Some people fancy they are “sick”, who are not “sick”, and they, those people, ‘afflicted’ with imaginary ailments, have psychiatry and the entire “mental health” treatment bureaucracy to “service” them.
Report comment
Did I need a comma? after “involuntary” ?
Put “voluntary seeking” in quotes?
Doctors give “help” according to the law and science so I use the term.
Overeating, a choice, was defined as a sin.
If atheist, who are you offending when you overeat?
Report comment
Paternalism is at work here. “Seeking help” is presumption. The government (in league with exasperated families) in many case would impose it’s version of “help” on those who never sought it.
Convince a person that they are “psychologically distressed”, and that’s pretty close to convincing the same that they have a “disease”. The idea is to “calm” such a person through brainwashing and serving the interests of other people.
Well, when a person eats themselves to death, I guess that makes overindulgence, in that instance, a bad choice, except, perhaps, as a form of suicide, and in so far as suicide goes, I imagine there are many other better ways to go.
Report comment
“Paternalism is at work here.” No, I say it is the matriarchy. All punishment can not appear to be punishment. Hospital not a jail, Medicines not drugs are given. No specific fault or problem is confronted to avoid the possibility of violence.
Report comment
“The matriarchy”? I think you need a new theory.
Report comment
it is neither male or female
Report comment
….”atheist”? Cool. I STILL don’t believe in the God that you don’t believe in, either!….
Report comment
Thank you for all of your community service in support of the disenfranchised; however, not so much in this post. I contend that psychiatry is a (harmful) philosophy that masquerades as a medical science and that it is illogical to defend psychiatry (or any medical science) based on philosophy. Wittgenstein implicitly rejects psychiatry and other “real” medical sciences when challenging “physicalism” because physicalism is the foundation of medical science. You explain how the DSM categorizes social welfare problems, but thereafter you continue to assume that they are somehow medical problems anyway (the subject of psychiatry). It is difficult for cultural leaders to imagine the natural emotional suffering (pain) of the disenfranchised; they have different experiences. However, tagging social welfare problems as medical problems is staggeringly oppressive for the disenfranchised; it promotes suicide. “Of all tyrannies, a tyranny sincerely exercised for the good of its victims may be the most oppressive (C.S. Lewis).”
Report comment
Bingo.
Report comment
Yep..BINGO!
Report comment
Hi Steve,
thanks for your comments, but I don’t know why you think I am defending modern psychiatry through philosophy. I am critiquing it in a way that leads to the conclusion that it is misplaced to view mental disorders as medical conditions.
I know that most Mad in America contributors don’t need to have an elaborate philosophical analysis of this position, but my blogs are aimed at those that are still convinced that madness is a medical disease, hence why I am setting out an elaborate and (sorry) rather slow argument. I completely agree with you that labelling someone’s distress as disease or illness is disenfranchising and disempowering.
Report comment
Thank you for your response and again for your community service. Perhaps it is me that is misunderstanding “labels;” somehow I understood you to consider yourself a “Critical Psychiatrist.” I understand Critical Psychiatry to criticize the practice of psychiatry but support its legitimacy in addressing “madness.” I am an “Antipsychiatrist” because I am more critical of the harm caused by the illegitimacy of psychiatry in addressing natural problems with living than the resulting harmful practices.
Report comment
I am not claiming to speak for all ‘critical psychiatrists’ but what I feel is that some problems of living need a social response of some sort – whether that is to help the individual or to protect the community. I don’t think the response should be fundamentally medical, but I do think that medical interventions can sometimes play a part. I think that sedatives of various sorts, including antipsychotics, can be helpful if someone is acutely manic or psychotic, for instance. I am concerend about their long-term effects, but for some people I think the benefits probably outweigh the harms of long-term tretament- just probably not nearly as many as currently take them long-term.
So I agree that any institution that is based on the idea that mental disorder is a disease is problemmatic and that we need to fundamentally re-imagine our current responses (although I do not have a blueprint for the future, and would be most interested in other people’s ideas). But I think medical or pharmaceutical expertise of some sort will still have a small but useful role to play in a new system.
Report comment
Joanna, I wish we could bring back the “moral therapy” or “soothing treatment” like the 19th century Quakers offered. I heard they achieved a 90% total cure rate with folks totally out of touch with reality. No drugs, locks, electroshock, or other abuse.
Report comment
I consider emotional pain to be a natural response to painfully distressful experiences; I support drug therapy for emotional pain managed by general practitioners consistent with medical science guidelines for addressing physical pain.
Report comment
Let’s get rid of psychiatric prisons, and make the psychiatric prisons of the moral managers redundant as well. If liberation = health, well, I’m not sure how many birds you take out with that one stone.
Report comment
Hmmm. In his book Miracles, Lewis talks about materialism as a philosophy. Sounds like “physicalism” may be a synonym for that mindset. Most churches have bought into psychiatry because they’re materialists for all practical purposes. They just don’t know it yet.
Report comment
Yes, I understand physicalism and materialism to be synonymous.
Report comment
I don’t think we know very much about the CAUSES of anxiety and depression and suicide…
whatever words you use to describe these sufferings….
Report comment
When approaching this issue, it is extremely important to separate TWO distinct levels of analyses. One is the conventional level of analyses – we analyze how trees grow, how the weather happens, how digestion takes place in our body, the chemical/molecular structure of compounds, and even how the brain works along with neural correlates of thoughts, etc.
The second level of analyses relate to understanding the moment-by-moment manifestation of the mind-stream (i.e., “stream of consciousness”). We need to remember that we only have ONE thought moment at a time (see for example: Slagter, Heleen A., et al. “Mental training affects distribution of limited brain resources.” PLoS biology 5.6 (2007): e138). This mind-stream happens in everyone all the time, whether one is cooking, driving a car, gardening or carrying out a research investigation (such as studying the brain). Even when reading this article, our mind-stream is constantly changing.
Joanna mentioned the importance of the social context. This too can be understood by considering the mind-stream. For example, seeing a person you really like would result in a pleasant feeling. However, if that person became your enemy one-day, then seeing this same person would result in an unpleasant feeling. This change is due to social experience – not DUE to changes in neurons (although neurons would have changed as a RESULT of social experiences – note that the brain is changing all the time as a result of human experience). To take another example, if someone has learnt as a child that interrupting a conversation is rude, then when one observes someone interrupting, this behavior would be labeled as ‘bad behavior’ (due to the social expectations) and if the person has not learnt this, then the person would not care about someone interrupting another person.
It should be noted that Buddhist teachings have comprehensively (and systematically) analyzed the mind-stream and the these teachings talk of “conditioned causality” – i.e., how mind-states are interrelated in different ways and how various causes and conditions lead to other causes and conditions, etc. To understand this mind-stream better – it is also useful to conceptually understand what is meant by the “present moment,” “the past” and “the future.” One can get an idea about all this from the following academic article: “Theoretical Foundations to Guide Mindfulness Meditation: A Path to Wisdom.” Current Psychology (2017).
As I see it, unless we separate the two levels of analyses described above – people will be continuously arguing in circles. The problem with attempting to understand the brain/neurons with the aim of understanding the mind/consciousness) is that one forgets that the inquirer is interlocked with the item under inquiry. The two levels of analyses can also be thought of as the ‘third person perspective’ and the ‘first-person perspective.’ The following article is also useful to understand the two levels of analyses: Karunamuni, N.D. (2015). The Five-Aggregate Model of the Mind. SAGE Open, 5 (2).
Report comment
I posted the above comment a few minutes ago, but it looks like it had got marked as ‘spam’ because it had too many links (therefore, I had to post it again without links – the comment above). However, I thought of attempting to add the following free link (it is a LEGAL link) to the article “Theoretical Foundations to Guide Mindfulness Meditation: A Path to Wisdom,” (2017) from the MindRxiv research repository: https://mindrxiv.org/mfs63/
Report comment
Nancy99,
The solution has been there for 2,000 years!
Report comment
That’s true Fiachra – 2600 years to be precise!
Report comment
Sorry you’re right.
I have experienced a great improvement in the quality of my life through Buddhist Practice and Philosophy. And this was without changing anything “on the outside”.
Report comment
If you look at people with longterm validated recovery a a lot of them will identify Buddhism as the key.
You are doing a good service by promoting the value of Buddhism.
Report comment
Thanks Fiachra. I too have benefited a great deal from Buddhist teachings. Yes, there are many things that happen to us that are beyond our power to change – however we can change the way we view/approach these issues and that makes a BIG difference.
Report comment
Hi Nancy,
thanks for these comments. My next blog is about just this subject- how we need different approaches to knowledge for different contexts and subjects. I will refer to Heidegger and I know that some people have compared his later philosophy to Buddhist teachings.
Report comment
Thank you Joanna – I look forward to reading your next blog.
Report comment
Agreed. Part of the problem is that the difference is the level of analysis. Another problem is the assumption that terminology used in differing frameworks are equivalent. Many times, they aren’t. This leads to people talking past one another because they assume they’re talking about the same or very similiar thing.
Report comment
https://www.youtube.com/watch?v=j6AhepWgYg4
Report comment
The philosophy football match between the Germans and the Greeks is also great fun
https://www.youtube.com/watch?v=B6nI1v7mwwA
Report comment
Comment removed for moderation
Report comment
I agree with you Dragon,
There’s no schizophrenia. People have breakdowns because they get overloaded. They’ll be “behaving” “irrationally” to a certain extent because thats part of a breakdown.
The breakdown might mend itself but the person might also need to work on any underlying weakspots.
The chemical approach turns a person into a long term patient. In my opinion most longterm patients are created by the treatment.
Note that “mental illness” arrived with the industrial revolution in Victorian times, when appearance meant Everything.
Report comment
I agree Dragon. The field of psychiatry ASSUMES that the brain changes for no reason at all and therefore assumes that the brain has to be treated with medicines (note that they also provide all types of detailed neuro-jargon explanations as to how these medicines work – as if the activity of the brain has been fully understood!). They completely forget (and ignore) the fact that it is HUMAN EXPERIENCE that brings about changes in brain chemicals and structural changes in the brain. Even animal studies have shown this. Mice subjected to various psychological stresses (e.g. being restrained) show adverse changes in the brain [see for example the following article: Popoli M, et al. (2012). The stressed synapse: the impact of stress and glucocorticoids on glutamate transmission. Nature Reviews Neuroscience. 2011;13(1):22-37] – these changes are reversible through psychological means (e.g. when stressed, restrained animals are released as described in the same article).
Report comment
Hi Nancy99,
I don’t see life experience changing the brain much. And I know plenty of people that have changed their lives completely in late middle age.
But if you look at people like Will Hall (Pioneer) and Dr Rufus May (British Psychologist) that have both been labelled “schizophrenic” and have recovered – they Both practise the Buddhist Approach.
Report comment
Hi Fiachra,
Perhaps you misunderstood what I meant by ‘life experience.’ Our brains are constantly changing all the time, as a result of experience and this happens regardless of age. Life experience could involve reacting to a life stressor by ruminating, regretting, proliferating thoughts, etc., or letting go (though the practice of mindfulness for example). Many studies have shown that the practice of mindfulness (that prevents mental proliferations and rumination and reduce psychological stress) also changes the structure and function of the brain and neurons in positive ways. On the other hand, ruminating, regretting, proliferating thoughts, etc. are linked to so called “mental disorders.” So, even if one starts meditating (e.g. Buddhist practice) at a later age, that can have positive benefits for mental health.
If you think I have misunderstood your question, please let me know! 🙂
Report comment
Nancy99,
I see it more in terms of psychology than actual brain change; but It’s not really an issue – as we’re talking about the same solution.
Report comment
Fiachra: I agree that it is not necessary to bring the organ brain into these types of discussions – but because we hear so much about the brain and neurons these days (and it is emphasized in psychiatry!), sometimes it is useful to talk about them in terms of where they fit into the equation. I think there is even a book titled “The Buddha’s brain” where the changes in the brain that happen with meditation practice are discussed.
Report comment
so we are talking about mental states…and the words we are using…
words can be very damaging…but there is one word I want to keep talking about…
that word is biology…and what does biology have to do with mental states…
we need critical thinking here…not just emotion…
Report comment
what does biology have to do with mental states..
what does neuroscience have to do with mental states…
do you think we should continue studying about the serotonin system in the brain..
does any of this say anything about mental suffering…
Report comment
littleturtle: Biology is ONE of the factors that can contribute to our experienced “mind-stream” that manifest moment to moment. But it is NOT the only factor. Other factors that contribute include our various life experiences, our conditioned attitudes and views, attachments, etc. The problem with psychiatry is that it makes the assumption that mental issues are purely biological and therefore many of them need to be treated with medicines. If you read the article (“Theoretical Foundations to…) I posted in an earlier comment here – it gives more information on various different FACTORS that can influence the moment-to-moment manifestation of the mind-stream.
Also note that our brains/neurons are CONSTANTLY CHANGING all the time as a RESULT of our experience (this is generally referred to as ‘neuroplasticity ’). To take some examples: studies have shown that as taxi drivers do their jobs (psychological causes), their brain/neurons change. jugglers gain more grey matter in certain areas of the brain as a RESULT of engaging in this activity. Various psychological habits, choices, etc., also change the brain. For example, research has shown that impulsivity trait results in reductions in gray matter in the brain. On the other hand, mindfulness practices (that result in reductions in impulsivity) change the structure and function of the brain in positive ways (e.g. increases in gray matter and cortical thickness). I also gave an example of a mice study in a different comment here. So, although biology affects our mind stream, it is our mental states that continuously change the brain and neurons (note: although biology can be affected as a result of an injury to the brain or due to a tumour, etc. – these are rare and a completely different story).
Also remember that how the brain works (as an organ) has NOT been understood AT ALL. So, all the authentic-sounding explanations that is provided in psychiatry regarding how neurotransmitters work, about serotonin levels, GABA, glutamate, PEA, etc., can be very misleading. Pharmaceutical companies come up with various medicines for mental problems using a purely ‘hit or miss’ approach, and these may work for some only because of their ‘placebo effect.’ Additionally, we need to remember that despite decades of research, scientists have not been able to find any structural or other brain differences between patients who show up with “mental illness” and healthy individuals. This is the reason why doctors use subjective criteria (check-lists) to diagnose patients – they do not have any objective tests like blood tests.
Report comment
When you suffer sustained stress you loose magnesium. Magnesium plays a vital role in the brain by regulating the N-Methyl D-Aspartate receptor. The NMDA receptor is a glutamate receptor. Glutamate is the major excitatory neurotransmitter in the central nervous system. The NMDA receptor is blocked or gated in a voltage dependent way by…wait for it…magnesium ions.
Further Glutamate (major excitatory neurotransmitter) and GABA (major inhibitory neurotransmitter) convert from one to the other using the active form of B6 and an enzyme called GAD…glutamic acid decarboxylase. Now if there is a problem with the genetic expression of GAD there are internal biology problems…. Now why and how do we know this is this related to mental health ? Because alcohol and benzo’s/hypnotics directly unbalance this system (externally) causing: anxiety, aggression/violence, depression, toxic psychosis, grand mal seizure, death.
Most of it is referenced here:
Magnesium supplementation and test anxiety
Oral Magnesium Supplementation and Test
Anxiety in University Undergraduates
http://www.jasnh.com/pdf/Vol11-No2-article2.pdf
Antidepressant- and anxiolytic-like activity of magnesium in mice
http://www.sciencedirect.com/science/article/pii/S0091305704000231
Consequences of Magnesium Deficiency on the Enhancement of Stress Reactions; Preventive and Therapeutic Implications (A Review)
http://www.mgwater.com/conseq.shtml#CONCLUDING
Magnesium deficiency induces anxiety and HPA axis dysregulation: modulation by therapeutic drug treatment.
https://www.ncbi.nlm.nih.gov/pubmed/21835188
Magnesium deficiency and stress: Issues of their relationship, diagnostic tests, and approaches to therapy.
https://www.ncbi.nlm.nih.gov/pubmed/26591563
Dietary magnesium deficiency affects gut microbiota and anxiety-like behaviour in C57BL/6N mice.
https://www.ncbi.nlm.nih.gov/pubmed/25773775
Low dietary intake of magnesium is associated with increased externalising behaviours in adolescents.
https://www.ncbi.nlm.nih.gov/pubmed/25373528
Essential elements in depression and anxiety. Part I.
https://www.ncbi.nlm.nih.gov/pubmed/24948052
The mechanism of magnesium block of NMDA receptors
http://www.sciencedirect.com/science/article/pii/S1044576584710128
Zinc, magnesium and NMDA receptor alterations in the hippocampus of suicide victims
http://www.academia.edu/14325192/Zinc_magnesium_and_NMDA_receptor_alterations_in_the_hippocampus_of_suicide_victims
Zinc, magnesium and NMDA receptor alterations in the hippocampus of suicide victims.
https://www.ncbi.nlm.nih.gov/pubmed/24055117
Report comment
Ironically the drugs they give prevent your body from absorbing these nutrients. I believe Abilify was causing my anemia. After going off it, my iron levels normalized and I’m no longer depressed all the time.
Report comment
Just like a man who works out with weights may have large, defined muscles. Would you say, “His large biceps cause him to lift weights three hours a week”? If you subscribe to the “science” of psychiatry you might. Next, you convince him or his doting family members that his big biceps are a disease, but luckily you have some safe and effective treatments to shrink them to normal levels. 🙂
Report comment
I don’t know what to say….I thought it was very important to study neuroscience…
maybe we will understand better why people get depressed and suffer..
I have had awful problems with depression….I want to know more about serotonin…
I hope dr Moncrieff says something here…
Report comment
The reality is that serotonin has very little to do with depression. There are people with very low serotonin levels who are not “depressed”, and “depressed” people who have very high serotonin levels. That you think serotonin has anything to do with “depression” says more about the marketing efforts of PhRMA, than it does with reality. Much, perhaps most, of the bodies’ serotonin is produced in the gut, according to recent research.
And, “depression” almost always arises in persons who have been verbally, emotionally, psychologically, or even physically or sexually abused. Even adults who say they had “loving parents” are often unaware of just how badly they were hurt as children, because it seemed “normal” at the time. People don’t always “choose” to “suffer”, but at some point, they do choose to *continue* to suffer. As was noted briefly in some comments above, I can strongly recommend reading some books by the Dalai Lama. He explains Buddhism in a way that makes a lot of sense. It won’t make you a Buddhist, of course, but Buddhism has a LOT to say about suffering, the causes of suffering, and the alleviation of suffering.
And, it always helps to have as many good friends as one can get. I have MANY FRIENDS here at MiA, even if I’ve never met any of them in person. It’s a start!…. I hope this helps. ~B./
Report comment
IMO, many folks are convinced they have a disease like tuberculosis when they feel depressed. Why should they feel ashamed for feeling bad? Maybe their lives stink and their unhappiness is a sign of good emotional health!
Report comment
ok I have heard about a model for determining causes of mental suffering…
I really like it…the psych/social/bio/econ/pol model..
what do you all think about that…
Report comment
I believe that the biopsychosocial model is standard psychology (economic and political issues are included); my problem is with what passes for biology and neuroscience. Psychiatry’s neuroscience contradicts the most fundamental principle of every science that informs it (biology, physiology, natural science and general science); it also contradicts the most basic principle of the philosophy of science.
Report comment
Really beats the bio/bio/bio model we have, Littleturtle.
Report comment
I think you are right on yetanotheraccount…
Report comment
Only problem is you left out the spiritual. My “breaks” started at age nine because a Sunday school teacher told me I was going to Hell. I became firmly convinced I was damned and drove myself nuts. Finally, many years later, I studied the Bible for myself and realized Mrs. X had taught bad theology. Can you imagine telling preschoolers not to cry so God would let them into Heaven? Yeah. A four year old who weeps has committed the Unpardonable Sin!
Report comment
doesn’t sound good for mental health…
I had a similar problem…
Report comment
There is nothing biological about the current bio model; it is pure pseudoscience. The most fundamental principle of biology is biological reductionism (an organism is understandable through its physical mechanisms); biology cannot investigate a philosophy of “mind” by definition.
Report comment
Reductionism itself is dead completly, proof see here:
On December 9, 2015 Toby S. Cubitt, David Perez-Garcia, and Michael M. Wolf reported in the journal „Nature“[ http://www.nature.com/nature/journal/v528/n7581/full/nature16059.html ], that a mathematical problem, which is basic to many fundamental questions of particle and quantum physics, is definitely unsolvable: even with the theoretically complete knowledge of all microstates it is impossible to determine the macrostate of a material! See: Quantum physics problem proved unsolvable, here: https://www.tum.de/en/studies/studinews/issue-012014/show/article/32791/ .
Complete original text in English: http://arxiv.org/pdf/1502.04573v2.pdf
Supplementary Discussion: http://eprints.ucm.es/38062/1/spectral-gap_supplementary.pdf
Here a quote by Michael Wolf, professor of mathematical physics at the Technical University of Munich: „But up until now, such [in principle undecidable problems] were found only in very abstract corners of theoretical informatics and mathematical logic. No-one had expected something like this right in the heart of theoretical physics. However, our results change this picture, …because the insuperable difficulty lies precisely in the derivation of the macroscopic properties of a microscopic description.“
With that, the hopes in physics are ruined, just as Kurt Goedel dissapointed the hopes of the Hilbert program in mathematics.
See also: http://kurtgoedel.de/kurt-goedel-a-world-without-a-past/
Report comment
This is similar logic to the social model of disability, which argues that disability is caused by the way society is organised rather than by a person’s impairment or difference. It looks at ways of removing barriers that restrict life choices for disabled people. Whilst this approach has led to (mostly toothless) legislation against disability discrimination, critics have pointed out that it can also produce an unhelpful binary opposition between disabled and non-disabled people, marking the former as ‘the oppressed’ and the latter as ‘oppressor’. Also, a social constructivist model of disability disembodies lived experience of physical difference; whilst our understanding of the meaning of pain might be a social construct, our individual experience of pain and its associated effects must also be taken into account. Whilst the meaning of depression is a social construct a depressed person might nevertheless wish to take a drug which ameliorates its effects (no matter how superficially) in order to be socially constructive at all. To say that depression is ‘all in the mind’ is as limiting as claiming that it’s ‘all in society’. In truth it’s somewhere in between, where we all are, in the murky area between perception of ourselves as individual biological entities and social beings.
Report comment
How often does disability mean not working because one is paid by the state for not working? The line between can’t and won’t, when it comes to employment, can grow awfully thin indeed, given such smokescreens.
Report comment
Right, because who can possibly resist the temptation of living it up on $10k a year or less. /s
Report comment
I’m not saying a government check makes anybody rich. I’m saying there is a wee bit of difference between a lifetime of government checks, and subsisting off the labor of one’s own hands. Artificial disability is artificial disability. It’s very similar, in a way, to artistic ability. What do they say? Oh, yeah. Wiley like a fox.
There is a very good reason why they say ‘follow the money’ as well. Any one government check is going to a heck of a lot of people.
Report comment
Nobody subsists off the labor of their own hands unless they live alone in the wilderness and grow/catch their own food.
Report comment
According to Merriam-Webster, earn means “to receive as return for effort and especially for work done or services rendered.” Money that is not received as a return for effort, work done, or service rendered is unearned.
Report comment
I think you need to take some more classes at the local free skool, Frank.
Report comment
Don’t think I can make it without lunch, Uprising. To quote Bertolt Brecht, in translation of course, “Grub first, then ethics.”
Report comment
I agree, to a point. There are actually people running to shrinks begging for pills and MI labels so they can collect “nut checks” and loaf.
Then there are gullible folks who want to work and are told that the only way they can do so is through religious adherence to the shrink’s treatment plan.
Report comment
Many people have pointed out that instead of adjusting individual children’s behaviour through brain-modifying chemicals, we should devise an education system that accommodates a wider range of developmental trajectories; one that is better able to cope with children who need more physical activity and stimulation than the average child of their age 6.
The scary part is that the average person responds to such an observation as though it’s a deep, radical new concept, rather than with a jaded “Duh”…
Not criticizing the article, just sayin’.
Report comment
I was really hoping that dr Moncrieff would wrap this thing up with some concluding remarks…
maybe we have been horribly off topic..but there are some important points that need some response…
Report comment
If someone hasn’t already said this, Wittengstein’s argument against private language, I feel would be relevant here.
https://en.wikipedia.org/wiki/Private_language_argument
https://plato.stanford.edu/entries/private-language/
Hubert Dreyfus just recently passed away, but this paper, Merleau-Ponty as opposed to Freud I have always found insightful.
http://socrates.berkeley.edu/~hdreyfus/pdf/Alternative%20(Word98).pdf
Report comment