My cell phone rings.
“Is this ‘Robik’?” someone asks.
“That’s my nickname,” I answer, confused. “Who’s this?” It’s a police officer.
“We think we have your father here. He says he’s trying to get into your house.”
“I’m in my house. Where are you?” They’re outside, down the block. My mother and I run out to the street and approach the unforgettable scene: my father, old, grey and stiff, arms bleeding in handcuffs, is sobbing and yelling, surrounded by officers.
“You hurt me!” my father yells. “Why do you hurt me?” My mother and I, mortified and scared (please don’t shoot him, I pray to myself), run up to them.
“Does he have dementia?” an officer asks.
“Yes, I apologize for this.” I’m relieved to have an explanation. They take him out of the handcuffs and allow us to walk him home. My father tells me that he’s sorry, that he decided to take a walk but coming back he couldn’t discern which house was ours. So he started entering neighbors’ houses. We cry as we hold each other.
We had already warned him not to leave our house. We had already taken his car away. We were making plans to take away his cell phone. We were battling with the million little details of dementia. So we thought.
* * *
My father’s transition from being an independent person to one who could no longer care for himself was messy and prolonged. It took years for us to truly recognize his decline. We knew he was on antidepressants and anti-anxiety medications and that they didn’t seem to be successful. We supported his decision to sell his small business and go on disability because of debilitating stress and anxiety. He was nearing retirement age anyway. We agonized over his deteriorating driving skills and his increasing disorientation. We worried that he wasn’t taking his medications properly, or might even be over-medicating himself. But since he lived on his own — an hour away from family — we couldn’t be entirely sure what he was doing. To make matters worse, he was being sued by his downstairs neighbor for making excessive noise while walking in his home. We hired lawyers and acoustics experts and negotiated a settlement, but this is where my father seemed to spiral.
No one tells you when it’s time to take over for a parent’s care. You just realize that someone’s at the end of their rope, and they’re about to fall.
My realization came when my father’s housemate called us to let us know he had driven my father to his first electroshock treatment.
“Why is he getting electroshock treatments?”
“He says he’s depressed. He says he wants to die.”
When I called the clinic that was performing the “emergency” electroconvulsive therapy (ECT) on the advice of my father’s newest psychiatrist, it was clear to me that they did not know what medications he was taking, were expecting him to get himself to and from the clinic without driving (he planned to drive himself until we intervened and paid people to drive), believed he would actually follow their instructions (you’re not supposed to drive for at least a week after your last treatment), and believed he was on the brink of committing suicide. But my father was almost 70 and had never attempted suicide. I was alarmed.
Another important note: an MRI later revealed that my father suffered a mini-stroke (transient ischemic attack) some time before his psychiatrist signed him up for ECT.
“Do you know that my father is showing signs of memory loss and confusion?” I asked the clinician. “Are you sure electroconvulsive therapy won’t exacerbate this?”
“Although there can be mild memory loss from the ECT, your father is suffering from treatment-resistant depression, and the ECT can help him.”
He was wrong. It didn’t help.
* * *
You may have already heard that the statistics behind short-term and long-term effectiveness of psychotropic drugs are dubious — that for many people they simply don’t work or are harmful. You may have heard that the shifting emphasis on prescription drugs for mental health has not necessarily improved mental health. You may have heard about the hidden evidence that some antidepressants can increase a person’s risk of suicide. So consider this anecdote as a warning, with one important message: psychotropic drugs do not “balance” a person’s brain chemistry. They alter it, sometimes to an astonishingly harmful degree.
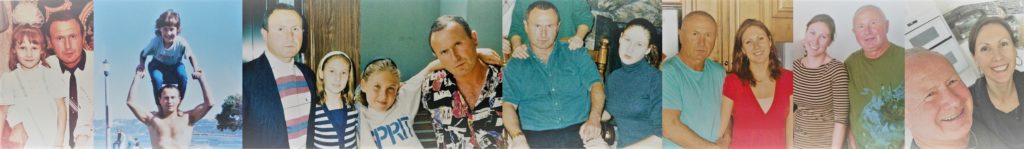
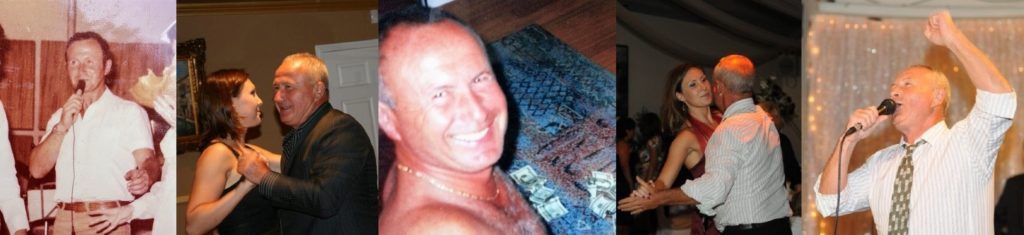
I never believed my father was clinically depressed. To the contrary, my father was gregarious, energetic and hard-working. He was a born performer, playing guitar, singing, performing as Santa Claus, emceeing wedding receptions, or reciting one of thousands of memorized poems and jokes. He had a witty, if caustic, sense of humor and he was always “on” in the company of others. The term “bipolar” or “manic depressive” would more aptly describe him, though his highs well outweighed his lows. I featured some of my father’s antics and talents in a compilation of old home movies — an entertaining glimpse into his typical disposition.
As I grew up, I recognized my father’s personality in people like Robin Williams (I’ll return to this point later). Like him, and like so many creatives with “dangerous gifts,” my father had demons. His marriage to my mother was deeply dysfunctional. He was a serial adulterer. His drinking of alcohol was likely influenced by his Russian genetic and cultural heritage. (Alcohol, I should note, is one of the most potent depressants a human can ingest.) And, as someone who had a family to support after immigrating to America at almost 40 years old, he shouldered immense levels of stress. He worked constantly. And the career he fantasized about, one full of music, singing and poetry, never materialized.
My father’s first foray into psychiatric medications coincided, not surprisingly, with the collapse of his marriage. A therapist prescribed Zoloft for depression. This was twenty years ago, before the term “chemical imbalance” was in vogue.
Following the Zoloft, two strains of a pattern emerged. Either my father would feel better and stop the medication, or he would feel worse and a doctor would increase his dose or introduce new medications. Throughout this pattern, my father continued to drink and never went to any sort of therapy. This lasted for close to two decades. He altered his mental state with pills and alcohol, which resulted not only in no improvement to his mental or emotional well-being, but ended with him abandoning his business and feeling worse than he ever had.
For me, there are a few clues that my father was misdiagnosed and mistreated. Medical professionals were probably rarely, if ever, exposed to the reality of my father’s bipolar personality, because when he was manically “happy” he was not making doctor’s appointments. It’s doubtful he confided in them about his level of drinking, partying and dysfunctional relationships with young women. Additionally, there was a language barrier. It was easier for my father to make simple statements, like “I’m depressed” and “I don’t want to live,” rather than try to find the appropriate English words to delve into his mental state and his manic lifestyle. He also probably became unable to differentiate between what might have been a side effect of one of the multiple prescriptions he was on, and what was his own self-diagnosed mental health issue. Most people, including doctors, don’t really know what the behavior they are seeing indicates. Unhappiness, sadness, boredom, stress, these can all come across to a doctor or patient as “depression.”
When he signed himself up for the ECT because he “wanted to die” and could hardly move his limbs, I’m betting his doctors and nurses didn’t stop to consider that a recent stroke and his self-medicating with alcohol and multiple psychiatric drugs might be contributing to his psychosis, or at least to cognitive impairment that could have led to the emotional devastation and anxiety he felt at the time.
 One other thing I’m sure of: my father was a hedonistic pleasure-seeker. With his doctors, he found a high that could dull his senses and lift his mood. Although medical professionals may believe they are treating someone’s illness, my father, by ignoring things like therapy or sobriety, was enjoying the drug effect and sedation, the chemical fix for the unhappiness that came with the collision of his dreams and his reality. Meanwhile, the drugs wreaked continuous havoc to his brain.
One other thing I’m sure of: my father was a hedonistic pleasure-seeker. With his doctors, he found a high that could dull his senses and lift his mood. Although medical professionals may believe they are treating someone’s illness, my father, by ignoring things like therapy or sobriety, was enjoying the drug effect and sedation, the chemical fix for the unhappiness that came with the collision of his dreams and his reality. Meanwhile, the drugs wreaked continuous havoc to his brain.
Over the course of twenty years, my father was treated by or consulted with at least 16 different medical professionals who prescribed him a total of at least 21 psychotropic medications. He was frequently taking more than one medication at one time. Eventually, the antidepressants and anti-anxiety medications were not strong enough for him. His prescriptions were increasingly for antipsychotics, drugs that are used to treat schizophrenia and other psychoses, as well as anticonvulsants that are typically prescribed for mania.
Additionally, my father was taking medications for other maladies, like blood pressure, cholesterol and blood clots. It wasn’t until this year that someone pointed out to me that a statin can have neurological side effects, including depression, confusion and memory loss. My father had been on statins for years.
And, this is the hardest part for me to accept: It’s well-understood that SSRIs, along with several other drugs, increase the risk of a stroke. This is particularly true if a person has been on blood thinners, which my father had been. I’m still a bit enraged when I think about the fact that doctors didn’t warn my father that he could increase his chances of a stroke by being on blood thinners and antidepressants, especially considering that his blood pressure and cholesterol levels already made him a stroke risk.
* * *
Upon completing a whopping 11 ECT treatments, my father only became more disoriented, more forgetful and less coherent. We could no longer let him drive, so we sold his car and asked his doctor to notify the DMV that his driving was impaired. Having evidence of my father‘s recent mini-stroke and memory loss, the doctor surmised that it looked like he was beginning to suffer the early stages of dementia.
From then on, my father was ping-ponging between my sister, my mother and me as his caregivers. We prepared every meal, eliminated his access to alcohol, supervised nearly everything he did and dutifully took him to his medical appointments. This included an almost monthly visit with a psychiatrist. By 2018, my father was taking lithium for depression/bipolar disorder, lamotrigine for bipolar disorder, clonazepam for anxiety and sleep, donepezil for dementia, plus his statin and other medications.
Meanwhile, I became more and more alarmed by my father’s mental and physical decline. After reading a well-known tome about caring for someone with dementia — “The 36 Hour Day” — and joining a 20,000-member Facebook group for caregivers of people with dementia and Alzheimer’s, I was introduced to many symptoms that I recognized in my dad. He was emotionally volatile, frequently sobbing for no reason. His physical movements were impaired: he had trouble moving his limbs or bending his body in any way, which meant he never wanted to change his clothes, nor shower. His mental decline was staggering. He no longer understood basic facts, or people’s names, ages and relation to him. He had no ability to read, play guitar, or even watch television. All technology became a frustration to him. He had hand tremors. His writing ability regressed to the point that he couldn’t spell basic words and would write painstakingly and slowly, like a child. He asked the same questions over and over, compulsively agonizing about small facts. He had trouble seeing. He did damaging things on accident, like pour liquid soap into a cup and drink it, or leave a faucet on.
Worst of all, he developed extreme combativeness and aggression, even physically lashing out, and yelling angrily at the top of his lungs, often in public. We began to fear him and the increasing frequency of “catastrophic reactions” that are well-known in the world of dementia.
One thing “The 36 Hour Day” and all medical professionals seemed to agree on was the obligation to treat a patient’s depression, even if (and maybe especially if) the patient has dementia. But this did not make sense to me. His treatment for depression had all but failed for 20 years; I couldn’t understand why medical professionals pursued this unicorn of a cure. While they were busy experimenting with his brain, my father was becoming a monster, and it agonized us that he was behaving so wildly and dangerously with everyone who cared for him (and in front of my small children — who hated being around him). The only reprieve we got was when he slept, which was often. After all, the majority of the drugs he was on had major sedating effects. But when he was awake, it was like dealing with an aggressive, 200-pound zombie. We were nearing the end of our ability to manage him. We considered two end-of-the-road options: a memory care facility and/or much heavier medications. We toured some facilities and asked the psychiatrist for Seroquel. Seroquel is a “black box” drug, which means it comes with the FDA’s most serious warning for serious or life-threatening risks. It also increases the mortality rate for dementia patients. Even though it’s specifically not approved for dementia, it’s well known as an off-label treatment. To my shock, after all the hand-wringing we did about the Seroquel, I found out that my father had already had a prescription for it several years earlier, before the dementia diagnosis.
Between all the appointments, medications and terror in our home, a thought continued to nag at me: how could this man suffer such a massive decline? He was barely 70 years old. The people at the memory care facilities were wheelchair-bound and decades older than him. There was no way he could sit alongside them. He never wanted to sit. He stood and paced frantically, he could walk for hours. If he went to a facility, they would only sedate him more, because he would be a combative nuisance.
When we took my father to a neurologist to see if there was anything new to report on his latest MRI, we learned that nothing had changed. There was nothing more going on in his brain than his original scan showed two years earlier.
“Can you at least test him? Find out how bad his dementia is? We don’t understand why he’s behaving this way,” I said. But the neurologist said my father seemed to be past the point of being capable of sitting through testing. He couldn’t sit at the appointment, he was complaining and yelling from the moment we entered the room, to the moment we exited.
“You know, the dose of Seroquel you have him on is not that high. You might consider increasing it,” the neurologist offered. I felt so defeated. Not a single drug was improving his condition.
“Okay, but can we at least take him off some of these other pills? They’re clearly not helping.”
“That’s a conversation you need to have with his psychiatrist.”
We’d already had that conversation. Her response was to replace lamotrigine with Trileptal. She didn’t even know, and then was fairly unconcerned, about his dementia diagnosis. She asked him how he felt, he talked through his mental fog about how depressed he was and how it was the worst day of his life, and she typed on her tablet and tweaked his prescriptions. It was a textbook case of what I later learned is referred to as the “15 minute med check.” After a few of these appointments, it was clear to me that my father’s brain was a problem no one could solve and no pill had ever seemed to solve. Not only that, the fact that he was making life in our home impossible seemed not to register with anyone.
I came to the conclusion that because doctors are always going to aim for “treatment,” it’s very difficult for them to accept the concept that drugs are doing more harm than good and that abandoning them might be warranted. They are not thinking about discontinuation, tapering and the complicated nature of a body’s and brain’s withdrawal symptoms. When the medical professionals had seemingly no interest in my father’s completely “insane” behavior, I looked more closely at his medications. The side effects were staggering: blurred vision, tooth pain, memory loss, muscle stiffness, depression(!), suicidal thoughts, drowsiness, insomnia, aggression. I read about the tragic misuse of sedating medications on people with dementia and small efforts to end the practice. I read about the use of these incredibly strong psychotropic drugs on children in the foster care system, on prisoners, on migrants. I read in the caregiver Facebook group how many caregivers were sedating their loved ones with hardcore drugs, and treating them for depression and anxiety, and yet still experiencing agitation and violence, just like we were. A study even shows that long-term use of benzodiazepines leads to a significantly higher risk of developing Alzheimer’s. “Unwarranted long term use of these drugs should be considered as a public health concern,” the study concludes.
I also read about “polypharmacy,” which is typically defined by a patient taking more than five medications at one time. Polypharmacy is associated with an increase in adverse drug events, reduced functional capacity and several geriatric syndromes.
What are we participating in, I wondered? Why aren’t the doctors who are seeing my father get worse and worse scrutinizing the medications more closely?
I’m going to cut to the chase here:
My father now uses Skype on his own to talk to friends. He has a tablet to watch YouTube. He reads. He plays guitar. He’s memorizing new poems. He recently transcribed, quickly and with perfect spelling, the song he sings in the YouTube video. He plays with my children almost daily and laughs uproariously. We got him a dog and he walks her and loves her. He rarely sobs. He almost never yells. He changes his clothes and can shower by himself. He can walk to the neighborhood pool by himself, swim, and walk himself back without getting lost. His memory has markedly improved. And his severe muscle stiffness is gone. Hand tremors, gone. He can hop, skip, even sprint. He does push-ups and sit-ups in his room every day without prompting.
How did this happen?
Well, three months ago—without any medical professional’s knowledge or assistance — we eliminated his last psychotropic prescription (please note: abrupt discontinuation is not recommended). We have him on a healthy diet and a routine of physical activity. And no alcohol. And a little THC.
It was as if my father, the one I knew, came back from the dead. As the months go by and I watch him emerge from his chemical stupor, I am in disbelief that such a profound change can happen in a person simply by removing the side effects of medications (by removing the medications themselves). It occurs to me that for so long what we thought was his declining mental state could actually have been a state of disinhibition, the way one might feel when they’re high or drunk. His wild and impulsive behaviors, his disorientation, the loud and combative aggression — in hindsight they seem like that of a person who spent his waking hours inebriated. And now, in a matter of months, he’s sober.
Just imagine if we had let my father stay on the medications, as doctors prescribed. We would have assumed, for example, that his inability to write was a symptom of his dementia. If we had told his psychiatrist “he’s no longer able to write,” she would have chalked it up to the recent dementia diagnosis we told her about, and would have continued right on keeping him in the chemical cage that took away his fine motor skills. He would have spent years in the stupor, unable to write his poems and songs. How many other people, I wonder, are stuck in a chemical cage, not realizing that their mental and physical well-being has deteriorated because of side effects? A mere six months ago, we were considering memory care facilities for my father, and would have put him on more sedatives to manage him, which now seems truly absurd.
Now the flip side: He did have a mini-stroke and we do think there is some mental fallout from that. He is, and will always be, a drug-seeker, looking for the magic fix. He tells us often how terrible he feels, how depressed he is. The more coherent he becomes, the more aware he is of his loneliness, his sadness, and his boredom. A pill — I’m convinced — won’t fix that. It never did. As his voluntary caregivers, we do what we can to keep him active and stimulated, as well as safe and healthy. We’re not going to let him drive, and we still supervise him almost everywhere. But — and I’m not exaggerating — all of the monster-like qualities that we thought were severe symptoms of his dementia have practically disappeared. The spectrum of his emotional volatility narrowed substantially. We’ve found ourselves questioning whether he has dementia at all.
* * *
So, a word about Robin Williams:
When Robin Williams committed suicide in August of 2014, within days the world began talking yet again about the need to treat depression. Everyone seemed to gloss over the fact that Williams was misdiagnosed with Parkinson’s disease. His wife wrote about “chemical warfare” in his brain, the symptoms of which went far beyond depression and into confusion, memory loss, paranoia, intense anxiety and insomnia. She was keen to pinpoint the final diagnosis — Lewy Body Dementia — as the culprit responsible for his suicide. Few talked about Williams’ multiple medications as a potential issue. Like the fact that he had taken two medications for Parkinson’s, which not only can lead to psychosis, but are specifically flagged as inappropriate for people with psychiatric disorders because they can lead to psychosis.
On top of the Parkinson’s drugs, Williams was also taking an antidepressant called mirtazapine, a “black box” drug with noted suicide risk. Additionally, Williams had taken out a prescription for Seroquel mere days before his suicide. Williams did indeed have “chemical warfare” in his brain. But we can never truly know how much of the culprit was his dementia, and how much was the number of psychosis-inducing, sedating, debilitating chemicals that the doctor who was “treating” him prescribed.
Susan Schneider, Williams’ wife, made clear that Robin Williams was being treated for depression. He was, after all, a star with the best medical resources and treatments available to him. It’s not like they weren’t going to treatment. Schneider described at least a year of doctor’s appointments, of trial and error with medications, of worsening symptoms, of a “terrorist” inside her husband’s brain. It was as if she was speaking about my father. But my father got better. He may still call himself depressed, but he’s sober, stable and coherent, the value of which he will probably never admit nor appreciate, because he doesn’t remember what the monster in him was like.
Having had this experience, the way I look at psychiatry and psychotropic medications has completely changed. Of course, I understand that they work for some people (though time and life changes also work). I know stories of people who have had specific mental conditions and behaviors that certain medications helped alleviate, usually in combination with self-care, psychotherapy and eventual discontinuation. Antidepressants might be an important tool in certain situations, though the benefits have repeatedly been shown to be small, especially when compared to a placebo.
However, I can say with certainty that doctors and psychiatrists often don’t really know if they’ve got the diagnosis, the treatment, or the symptoms right when it comes to mental health. They often aren’t taking time to understand the brain they are altering. They are often unaware of what other medications the patient might be taking. They don’t know if they’re treating the patient, or the patient’s side effects. And they can’t be sure that the cure isn’t worse than the disease.
If you are being treated with psychiatric medications, please consider my warning:
They are experimenting.
Every time.
On you.
At the end of the day, the psychiatric drugs you or your loved one are on are sedatives and chemicals. Some go so far as to call them neurotoxins. The longer you use them, the weaker your brain gets at being able to regulate itself on its own. The higher your risk of deleterious effects. And the harder it is to get off them. But sometimes that’s exactly what needs to happen.

















Your story is extremely education and at the same time extremely sad.
Thanks so much.
Jim
Report comment
This is very much reminiscent of my wife’s father’s experience. He really did have some dementia going on, but they put him on Risperdal and had him close to paralyzed. He was showing obvious signs of distress, trying to talk, rolling his eyes, moving his head side to side, but couldn’t make any coordinated movements of his body.
Once my wife got her mom to take him off, within three days, he was sitting up, making eye contact, talking, joking, laughing, feeding himself. Yet in his nearly frozen state, not one of the staff people or the doctor showed any concern that this previously vigorous and energetic person suddenly was unable to move or talk. The doctor, in fact, was very angry that Ginny’s mom had exercised her right to informed consent and stopped the drug!
One can only conclude that a) they don’t care, or b) the inert state achieved is considered the desirable outcome. It is amazing that 20 years of complete and utter treatment failure, in your dad’s case, led to absolutely no reassessment of the situation or any attempt to try something besides more drugs. It is sickening, yet all too common. I’m glad you were able to find your way out of the maze.
Report comment
Steve, they cannot BUT know better, unless something is deeply fundamentally wrong with the people working in the field.
It is difficult for me to believe that people, educated, are that clueless, or that bound to not be in the wrong.
But then, all of psychiatry is set up to ultimately end up being abusive, starting off with diagnosis and as such, I cannot see how ANY of their decision making or treatments will be rational and based on being informed or actually caring.
It must only rely on the manner in which cults work. No other explanation.
Why would anyone feel the need to hide the harms?
Report comment
Your father was a very good dancer, and EGOIC masters in medical disguise do not like when THEIR slaves are happy.
James Hillman, Re – Visioning psychology.
Report comment
Hopefully, Roberta, you’ll take the next step in your awakening, and realize that the DSM is really nothing more than a catalog of billing codes. ALL of the supposed “mental illnesses” in it are bogus, and they were ALL invented. NONE of them were discovered. The DSM is a laundry list of excuses and justifications to $ELL DRUG$. So-called “mental illnesses” are exactly as “real” as presents from Santa Claus, but not more real. Psychiatry is a pseudoscience, a drug racket, and a means of social control. It’s 21st Century Phrenology, with potent neuro-toxins. Psychiatry has done, and continues to do, far more harm than good.
In closing, I assume you meant to write, “And a little THC.”, and that’s not a typo for “TLC”. Yes, medical cannabis, and especially CBD oils, has a very real potential to HELP HEAL your Father, in a way that all the pHarma DRUGS cannot. Pharma sells drugs to make money, not to make sick people healthy….
And the quack doctors are some of the sickest people in society. They either don’t know, which means they’re incompetent, or else they do know, and do it anyway, which means they’re malicious and malevolent. The allopathic medical profession is incompetent, crooked and corrupt.
Report comment
Finally, someone as pissed off as I am. I truly believe most illnesses are caused by poison (drugs).
Report comment
Yip. Me too!
Report comment
Couldn’t agree more!
Report comment
High cholesterol? Heavy drinking? Sounds like a job for niacin if he’s going to get any outside substances administered. Of course the doctors would threaten you for even considering such a “dangerous” substance and they’d want to know who I was, so they could prosecute me as well.
Report comment
Bcharris, my gut is very unhealthy and it’s messing up my absorption of micro-nutrients. And ability to think straight. Off my SSRI drugs after 20+ years but they wiped out my intestines’ natural ecosystem. What should I do?
Report comment
Rachel777, do you take probiotics? If not maybe try some, but not all are created equal, make sure to find a good quality one. And there are foods that are a source of probiotics such as kefir, sauerkraut, kombucha tea, etc.
Report comment
I’m going on a regimen Rosalee. 2 Tbs of apple cider vinegar (with the “mother”) and slices of fresh lemon mixed with hot water after getting up each morning. Half an hour later 2 Tbs of EV coconut oil chased down by almond milk. Half an hour later breakfast with kombucha and a probiotic tablet. Before bedtime a charcoal tablet.
No refined sugars, dairy, or gluten for the month. No caffeine except the kombucha tea. Dairy tends to “set off” my system if I’m not okay just like gluten–though when my health is good and I’m not stressed out I can digest moderate amounts of these foods. I plan on eating fermented veggies every day instead of yogurt or kefir.
Report comment
Rachel, good plan. I found great success with homemade kombucha, kefir, and fermented foods. I stopped doing that when my husband and I went traveling full time and I’m convinced that’s what led to the current flare I’m having.
Incidentally, people are told to have yogurt for the probiotics but commercial yogurt has very little nutritional value and the sugar content feeds bad bacteria in your gut. The S. cerevisiae that’s in kombucha is well studied as protective in preventing candida and c.diff infections in those taking antibiotics.
Also, don’t forget to eat foods with prebiotics (a type of fiber) to feed your good gut bacteria.
I also highly suggest a turmeric (golden paste) or curcumin supplement. Curcumin is as or more effective as SSRIS (without the side effects) in multiple drug trials comparing them. Not that you’ll hear that on the news.
(It sounds like I’m speaking to the choir here, so this is mostly for others reading and learning about gut health.)
Report comment
I’m not deep in the know about pre and probiotics like the other commentators, but I am familiar with the use of supplements in place of medications. To set up an appropriate program, I’d have to see you in person for an interview and perhaps a Hoffer Osmond Diagnostic test (the infamous HOD I sometimes mention in correspondence on the site) to find out what nutrients I might have to use. I’m just a former crazy, myself, who accidentally treated himself, so I’d suggest finding out if there’s an orthomolecular practitioner in your neighborhood, many of whom can be found on websites (search “orthomolecular”).
Report comment
If you took the so-called SSRI “antidepressants” it’s no wonder that your digestive system is messed up. Probably one of the reasons is that the place in our bodies where we have the most serotonin is in the stomach. Massive doses of the damned things can screw everything up in that area.
Report comment
Ironically my stomach was already messed up due to intense stress and constant low calorie diets as an adolescent to earn love and acceptance by looking like Kate Moss or Calista Flockhart. Lol.
“You can never be too thin or too rich girls!” What all our mothers kept telling us.
Despite going 2 or 3 days at a time on little but iceberg lettuce, I never became thin, lovely and lovable. Just messed up my digestive system.
Report comment
Thank you for such a wonderful piece of writing that is both saddening yet offers hope. My own story is similar but I do recognise that your father’s experiences and how they affected you and your family have been particularly difficult. I am also in the process of reducing various medications for many of the same reasons you have highlighted with regards to your father.
My first experience of mental ill health was as a young man in my late 20’s which resulted in a 7 month stay in the local asylum some 40 years ago. Winding the clock forward my most recent crisis was 11 years ago and since then I have been under a total of 17 psychiatrists for varying lengths of time, experienced 7 hospital admissions, consumed copious amounts of medication and received ECT and had to give up employment. Ironically I had been working for the previous 13 years in both Mental Health Advocacy and as a Mental Health Support Project Co-ordinator. After 4 years of admissions and different medications, just like your father I was no better and my physical health was failing. I was so desperate it got to a point around 2012 where I actually begged for ECT in desperation for some relief from the psychological torment and physical pain and disteress I was in. The ECT, like the medications didn’t help in anyway. My mental and physical health was chronic and continued to decline even further.
Beginning of 2016 I suffered a stroke which I now suspect may well have been brought on by the Pregabalin, one of the medications I was taking at the time to supposedly help with the various aches and pains I was experiencing along with my severe anxiety, distress and depression which saw me wanting to end my life every single day. Sleep was a huge problem – around 4 hours of light broken sleep was the best I could hope for and on one occasion, just prior to the stroke I went a full 2 weeks without any sleep at all. I will jump forward to around 18 months ago when I made the decision to somehow find the courage to taper off the medications. I have been under the same psychiatrist for over 2 years now and although she is not in agreement with the decision I made 6 months ago to slowly taper she has supported me in this decision.
My physical condition is still quite poor but my mental health is a little better and it is early days. After beginning tapering around July 2018 I have been off the Seroquel/Quetiapine for 3 months now and am now slowly reducing my anti-depressant Sertraline. I am still taking medications for a mild heart attack which followed the stroke at the end of 2016. Progress is slow though I remain determined to see this through. I am one of the increasing numbers of people who are deeply angry at what appears to be irresponsible and dangerous practice by psychiatry who are the official sales force for the giant manufacturers and suppliers of these medications – namely the Pharmaceutical Industry. The fact that I am motivated and confident enough to compile this (very lengthy) comment is something of an achievement for me. I would never have managed this a year ago. All is far from ideal but I recognise that recognition and acceptance of progress, however slow and small, can be considered ideal in these circumstances. Thank you Roberta for lighting my fuse.
Report comment
Arlin, yes the numbers of people deeply angry with psychiatry are ever increasing and I hope it keeps increasing. I am glad you are doing better and determined to see your recovery through. Thanks for sharing your story, all the best, keep your fuse lite.
Report comment
Arlin, you’ve been through so much. Thank you for writing. You have all my best wishes for a stable recovery and a healthier future. Take care of yourself.
Report comment
Roberta, I have an incredibly similar story, is there any possibility I could speak with you? I have a radio show I would love to bring you on and something else I would like to discuss with you. My email is [email protected]… hope to hear from you!
Report comment
Roberta, what a horrible ordeal your father endured, as well as you and your family. As more people share their stories I hope others will avoid irresponsible, corrupt and harmful psychiatric treatment. Thank goodness your father is doing better and had you as a strong and very concerned advocate. It really makes me wonder what really happened with Robin Williams.
Report comment
Me too! I’ve suspected it from the moment I heard about Robin William’s death.
Report comment
Great story. Thanks for sharing. So much is written about the withdrawal effects but these drugs are also very bad to take and cause neurotoxicity, dementia, stroke, akathisia and so much more. I’m glad he’s improving.
Report comment
Roberta I was expecting another tragic story here. MIA contains many.
I’m so glad my expectations were wrong and your family had a happy ending. Like other happy endings on this site, you owe it to disobeying psychiatric orders. Congratulations! 🙂
Happy for you, your dad, and other family members.
Did you know research is showing that there are effective treatments for early stage dementia? Proper nutrition, rest, physical exercise, and lots of mental exercises. There are no drugs to fix these problems, but solutions exist. We need to stop looking for magic in a drugstore bottle.
Report comment
Roberta
Thank goodness you realized what was happening and you researched things. Glad that you were able to do this for your father.
The experience that Roberta recounts here is just one of thousands taking place all across the country. I’m not minimizing her and her father’s experiences but just want to emphasize that they are not alone by any means. What more do we need to push for the removal of psychiatry as a specialty of medicine? And of course, there are many other doctors who aren’t psychiatrists who are failing in their calling as healers because they’ve allied themselves with the drug companies and are satisfied with their positions as pushers and shills for the drug companies.
This problem is not confined to psychiatry. It’s time to begin talking back to doctors rather than just meekly bowing down to their instructions, and what often seem like absolute commands. Recently I was scheduled for a procedure and I told the doctor that we weren’t going to do anything until she answered each and every one of my questions about what was going to happen. She looked at me as if she couldn’t believe that I didn’t meekly accept things as they’d been laid out for me. And she tried to hold information back from me but I could tell from her actions and the way she didn’t look at me so I confronted her again and forced her to tell me everything. They are not going to tell you any more than they think that they can get away with so you have to keep pushing them until you feel satisfied that they’ve been as honest with you as you can make them be. I’m disgusted with doctors in general and don’t put up with much from them. Consequently I’m described as “prickly”, uncooperative, noncompliant, etc. Too damned bad. I now realize why my family didn’t go to doctors while I was growing up. My grandmother and mother were indigenous Wise Women who treated our ills at home with native remedies. They did their best to keep us out of the clutches of “medicine” carried out by the White medical system.
Report comment
Well said Stephen!
Report comment
Thank you for sharing your story.
Report comment
They almost killed me the same way.
Report comment
#MeAsWell
Report comment
After 4 years in the Psychiatric System I was written off as completely useless, and then I just about managed to stop the strong drugs – and completely recovered.
Report comment
Roberta,
You’re a good daughter, and your father is lucky (in a sense) that you are around.
Report comment
Roberta, Thanks so much for sharing this story. I am increasingly appalled that elders are drugged so much and so heavily. The plight of elders is of particular interest to me as I am not that much younger than your father. This story so very clearly illustrates the harm that those drugs can do, even drugs for physical conditions such as statins, which are given to elders like candy.
Much of this is due to the Medicare system. Medicare is not a benefit to elders. It is a benefit to the doctors who treat the elders. Medicare doesn’t pay elders a penny, but is paying billions to doctors and pharma companies. They use elders’ bodies and lives as objects, so they can get paid and enjoy a bit of power in the process. Old people are gonna die no matter what, so who will notice if a few guinea pigs get killed?
Thing is, we’re human beings, humans with decades of history, culture, memory, and tradition behind us. We are each unique and complex. We are not useless waste just because we are older. The medical profession needs to stop treating us like we’re emotionless, ugly things who lack intellect and perception.
As for the depression your father feels, my guess is that this will improve, perhaps very slowly, though. Alcohol and drugs (of any sort) will dampen a person’s ability to feel passionate. You end up with an “I don’t care” attitude which is truly a downer. You feel a lack of passion and direction in one’s life. The passion does come back, though. To live–this means you are striving for something. We need to have something we want, whether it is to run 5k faster, to get a better job, to earn enough money to feel secure, to find a mate, to raise kids, or to help a charitable cause.
Report comment
I have to disagree about Medicare. I’ve had some very expensive surgeries this past year and underwent other expensive procedures as well as trips to the Emergency Room. All of these things amounted to tens of thousands of dollars in bills, bills that I’d never be able to pay on my own. Medicare has taken care of almost everything for me. I’ve ended up having to pay about four thousand dollars of my own money, which is a tiny fraction of what the bills actually were. The problem is not with Medicare but with the hospitals and doctors who charge outrageous prices for their services. There’s something badly wrong with the medical system when you end up being billed ten dollars for a Band-Aid. And the interesting thing is that Medicare refuses to pay certain parts of the bills and the hospitals and doctors accept whatever Medicare gives them without any flap at all, which tells me that they’re still probably getting paid more than what they should be.
I have only great things to say about Medicare. Without it I’d never be able to have any medical care at all.
Report comment
Something is really wrong with the medical system when you go to the ER and get charged $800 for a bag of saline solution that they gave me intravenously for rehydration. Something is greatly wrong with the system when I was given two fizzy potassium pills in a glass of water and was charged $400 for them. Medicare takes one look at bills like that and reduce the price that they’ll pay the hospital and the hospital takes it with no problem. This tells me that they could be giving these services for lower prices in the first place but they do this because they can gouge insurance companies.
Report comment
Stephen Gilbert, Julie has a psych “diagnosis.” If you don’t, that might account for better care from Medicare.
Report comment
I would assume he does have such a “diagnosis.”
My fear about Medicare is that it might start forcing people to get “wellness checks,” blood tests, etc. and, if they want to “treat” you for something and you don’t want their help, using such a “diagnosis” in one’s past to forcibly administer unwanted and potentially deadly “treatments,” even when the person has a reasoned holistic approach, for their “own good.”
Report comment
I too have a psych diagnosis so I don’t think that has any bearing on the situation, and it’s not a good one either. Not quite as bad as the dreaded “paranoid schizophrenic” but right up there near the top.
Report comment
Very sad what happened to your dad, Roberta, but I am glad that you and your family took the bull by the horns and got him off all those meds! We are trained to trust doctors and be compliant, but anymore I don’t trust doctors! I was one to take ADs for over 20 years with GPs renewing my scripts. And they never did the wonderful things they were supposed to do. I’m angry at myself for continuing to take them despite that, yet I bought the “chemical imbalance” explanation and so it went.
When Robin Williams committed suicide, I KNEW it was about the meds, treatment resistant depression or worse. No one wanted to look at his mental health history and history of meds. It HAD to be about Parkinson’s or Lewey Body, with a passing acknowledgement that he had antidepressants in his system. Well, all the good THEY did! How is it that so many who suicide have antidepressants and/or other psych meds in their systems? And no one gives it any consideration. Well, we know the answers thanks to folks like Robert Whitaker.
Report comment
Exactly. The answer is always “more treatment,” even when they were receiving treatment for YEARS prior to their suicide.
Report comment
And if you get worse instead of better they accuse you of “pill shaming.” Defend pills by shaming patients for becoming disabled or dying.
I’m not out for shaming gel capsules or tablets. Those who should be shamed are the lying hucksters who hurt people and call them crazy for suffering. Too bad they’re shameless.
Remember Dr. Farid Fata, the cancer specialist? If he’d gone into psychiatry he would have gotten away with it. 😛
Report comment
What a great story Roberta, and a good writer you are.
I was expecting a different ending and loved the “fast forward”.
I appreciate you touching on RW’s death and very much appreciate you for not giving up on your dad.
Perhaps, different personalities are okay? Perhaps being miserable sometimes is okay or being ‘depressed’, or ‘anxious’.
You are exactly right, they are “experimenting”, “on”, “you”. Yet even after their experiments fail, they refuse to concede.
I am old enough now to know there is something not right with and about these treaters and I am very much starting to wonder if in some crazy way, they are projecting.
That all along it is really about some repressed need for power for psychiatry.
And possibly many occupations.
But within psychiatry, that need is a weapon.
Report comment