Readers of this website might be aware that antidepressants can cause suicide, other violent behavior and even homicide. These can be side effects or adverse drug reactions from the medication taken. Not only can antidepressants cause these side effects, but basically every psychoactive medication can put patients at risk. Few people may know that there are DNA tests that can identify individuals who might be prone to these adverse drug reactions.1
To understand what kind of information such a test would provide, it might be helpful to explain the science behind these DNA tests.
In general, human cells contain 23 pairs of chromosomes. The father donates half of the chromosomes; the other half comes from the mother. Every chromosome contains many genes. A gene is the part of the DNA that codes for proteins, and proteins cause hereditary characteristics to be expressed. A gene can have two forms, called alleles. If someone inherits the same allele from the father and the mother, the person is called homozygous for that trait; if they are different, the person is heterozygous.
Medication needs to be metabolized to be expelled from the body. This is done by certain proteins called enzymes. Most medications that interact with brain chemistry are metabolized by an enzyme system called Cytochrome P450 (also known as CYP450 or P450). There are many different P450 enzymes, and they are divided into families and subfamilies. Cytochrome P450 family names are denoted by an Arabic number (e.g., CYP2), the subfamily by a Roman uppercase letter (e.g., CYP2D), and the individual enzymes by another Arabic number (e.g., CYP2D6). The alleles are indicated with an asterisk and a number, separated by a forward slash.
If someone inherited the same allele from both his father and his mother, this could be, for example, CYP2D6 *1/*1. If someone has been given two different alleles from his parents, you get two different numbers, e.g. CYP2D6 *1/*3.
While an individual normally has only two alleles for each gene, there may be many different alleles that are possible for that gene, a situation that is known as genetic polymorphism. This genetic variability in specific P450 enzymes may influence a patient’s response to prescribed drugs, including antidepressants.
If somebody has two normal alleles (known as “wild type”), such persons are generally referred to as “Extensive Metabolizers.” Not all alleles produce enzymes that are equal in their biochemical ability. Variant alleles usually encode P450 enzymes that have reduced or no activity. People possessing these alleles are called “Intermediate Metabolizers,” and, if the alleles have no, or virtually no, activity, they are designated “Poor Metabolizers.” Some variant alleles produce enzymes that metabolize at a significantly higher rate than normal, and individuals with those alleles are referred to as “Ultra-Rapid” metabolizers.
The efficacy of the Cytochrome P450 enzyme system is additionally influenced by factors such as age, sex, other diseases and extrinsic factors such as diet, smoking, substance abuse (drugs, caffeine, alcohol) and co-medications. These different reactions can result in significant drug-drug and drug-gene interactions, which can lead to unexpected side effects and/or therapeutic failure.
If a drug is not metabolized and expelled from the body, it will accumulate. This could lead to intoxication and adverse drug reactions.
There are several mechanisms that can cause accumulation of drugs. The first one is inhibition: a drug can diminish the expression of a CYP gene. That causes a gene to produce less enzyme. Less enzyme means less capability of metabolizing the substrate, in this case a drug.
The second mechanism that can cause drug accumulation is substrate competition. With a limited amount of CYP enzyme, having two or more substrates may mean that neither get metabolized effectively, and both drugs might accumulate in the body. The third mechanism is when a CYP gene produces a CYP enzyme that is not working properly, that is, the alleles have reduced metabolic ability. The first two are drug-drug interactions. The third one causes drug-gene interactions. I will give examples of all three.
Patients are seldom put on just one drug. One medication (A) can influence the function of a CYP gene, e.g. slow down the expression of that P450 enzyme. This can happen even if that drug does not need that CYP to be metabolized. This is called “inhibition,” see table 1:
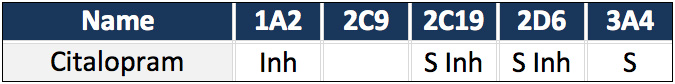
Table 1: Citalopram metabolized by CYPs2
Citalopram is metabolized, used as what is called a substrate (S), by CYP2C19, CYP2D6 and CYP3A4. It inhibits (Inh) CYP1A2, CYP2C19, and CYP2D6.
But if another medication (B) is metabolized by one of those CYPs that are inhibited, then drug B could accumulate in the body (see table 2). The interactions shown in color indicate the danger of side effects — the darker the color, the bigger the chances of adverse drug reactions.
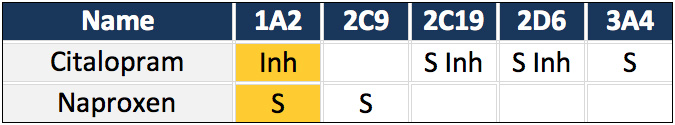
Table 2: Drug-drug interactions2
Naproxen is metabolized by CYP1A2, but because citalopram inhibits CYP1A2, the levels of naproxen could rise, increasing the chances of side effects.
Another form of drug-drug interaction is when two drugs need the same CYP to be metabolized (see table 3).
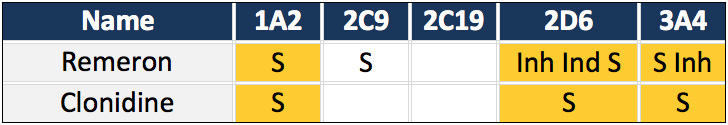
Table 3: Drug-drug interactions2
In this example, Remeron is combined with clonidine. Both drugs are metabolized by CYP1A2. Thus, there is substrate competition for this CYP enzyme. This means that the levels of both drugs could rise.
For CYP2D6, there is substrate competition as well, and, at low levels of Remeron, this CYP will be inhibited. As the drug levels rise, Remeron will stimulate the production of this CYP (Ind = induction). That will not be of much help, since the competition between the two drugs will slow down the metabolic rate of the drugs anyway. For CYP3A4, the situation could be worse: there is competition between the two drugs and Remeron inhibits CYP3A4. The metabolism of both drugs could be significantly reduced.
These drug-drug interactions can be extremely dangerous, even if the CYPs are genetically normal. In a 2006 study in older patients, the mean number of medications was 8.1 with a standard deviation of 2.5.5 Reducing the number of drugs by two decreased the mortality rate significantly.5 7 This is no exception. It is easy to see why medication use is now the third leading cause of death.8
This picture becomes even more grim if we take into account drug-gene interactions. If drug-drug interactions, by themselves, are hazardous, they are even more so when CYPs (which are supposed to get rid of the drugs) are not working properly. It has been estimated that around 99% of individuals have one or more variant alleles that could influence the enzymes that metabolize drugs.9 10 Most prescribers and patients are not aware of this. If doctors prescribe drugs assuming the patients have no problems metabolizing these medications, they jeopardize the health of their patients. Those people with problems metabolizing — the vast majority of patients — are at great risk of side effects.
Let us look at the example again in which citalopram is combined with naproxen. But now, through DNA testing, we have discovered that the individual has some loss of function alleles, so he or she is an Intermediate Metabolizer. In this case, the CYP genes for which there is loss of function alleles are colored in red.
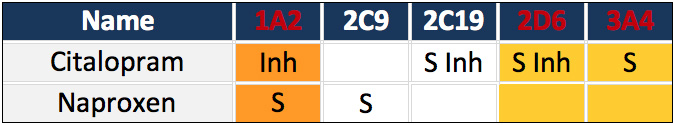
Table 4: Drug-gene interactions2
Let’s look at CYP1A2 in table 4. This CYP has only one functioning allele, which is inhibited by citalopram. The function of this CYP will likely be diminished to such a degree that the person will convert from an Intermediate Metabolizer into a Poor Metabolizer. For CYP2D6 and CYP3A4, similar problems arise concerning Citalopram. With two out of three designated CYPs practically nonfunctional, this patient will be depending on CYP2C19 to eliminate Citalopram. With so much loss of function, the levels of Citalopram will likely rise and cause toxicity.
Citalopram is strongly associated with violence.12 This patient is put at great risk by their doctor prescribing this medication to someone who is basically a Poor Metabolizer for the CYPs necessary to expel that drug from the body. Drugs that are metabolized by CYPs for which patients are Poor Metabolizers should not be prescribed. Poor metabolizers can hardly metabolize drugs, so side effects are expected.
Other prescriptions for disaster for people with variant CYP alleles are combinations like Cymbalta and Xanax.
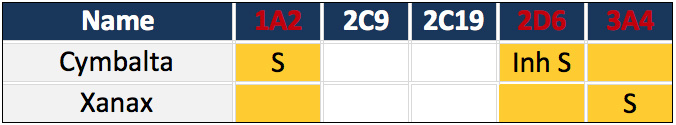
Table 5: Drug-gene interactions2
Cymbalta is metabolized by CYP1A2. If the individual has one loss of function allele, CYP1A2 will not metabolize Cymbalta at a normal rate. CYP2D6 can also metabolize Cymbalta. Unfortunately, this individual has one loss of function allele for this gene. In addition, Cymbalta will inhibit its own metabolism. If the normal enzymes are limited in metabolizing their usual substrates, CYP3A4 is the backup system.14 In this case, that will not be very helpful. There is an additional loss of function allele for CYP3A4, and Xanax is a competing substrate. These are simple interactions, but they are responsible for many side effects, which can result in death.
CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A4 metabolize more than 90% of medication.15 Generating a DNA profile of these CYPs will provide the physician with valuable information. It is a fact that doctors can spend only so much time with a patient. To assist prescribers, there are drug interaction databases available online to screen drug-drug and drug-gene interactions — for example, the Pharmacogenomics Knowledge Base https://www.pharmgkb.org/index.jsp and Transformer SuperCyp http://bioinformatics.charite.de/transformer/.
Within minutes, a doctor can get a clear indication whether the medication he or she is about to prescribe can be a danger to the patient. If those extra minutes can save a patient’s life, they are well spent.
Other enzymes are also involved in metabolizing psychotropic medication, and other medication besides antidepressants, antipsychotics, tranquilizers, mood stabilizers, AHDH medication, etc. can cause acts of violence. For example, Varenicline (Chantix®) as an aid to quit smoking, isotretinoin (Absorica®, Accutane®, Amnesteem®, Claravis®, Myorisan®, Sotret®, and Zenatane™) against acne, oxycodone against pain, or interferon alfa to regulate the immune system.12
These drugs are not primarily prescribed to patients with social, psychological or psychiatric problems. The argument that violence is caused by an underlying psychiatric disorder has been proven wrong repeatedly (see papers by Bielefeld and Maund and their colleagues at the Cochrane Collaboration)17 18, and also the blog by Peter Gøtzsche from November 16, 2016).
The technology for genotyping these five CYPs is widely available and would cover most of these dangerous drugs. I am convinced that once doctors start realizing that they are responsible for senseless suffering and that there is a way to, at least, diminish the chances of such horrific side effects as suicide and homicide by a simple DNA test, they will fully embrace “personalized medicine.”














This is a fascinating article, thanks.
Although, I think the ideal solution for many people is to never take psychiatric drugs, or to stop taking psychiatric drugs entirely if possible. Working out difficult feelings and thoughts interpersonally and in terms of what resources in the environment help was always better, in my experience.
Regarding this,
“The argument that violence is caused by an underlying psychiatric disorder has been proven wrong…”
This is misleading because there are no discrete psychiatric disorders that are the cause of anything (as Insel, Frances et al admitted, these categorizations of distress lack validity and are mere descriptions of clusters of behaviors, not well-defined illnesses). Distress and decisions to take action based on distress arises from complicated interactions between a person and their environment over time. No one “gets” or “has” a “psychiatric disorder” called things like “schizophrenia” or “bipolar” that then “causes” them to be violent. This whole way of thinking is so hard to understand; one might assume it comes from doctors who do relatively little intensive psychotherapeutic work with clients and thus do not understand that saying that “psychiatric disorders cause things” makes no sense.
Report comment
Matt,
I couldn’t agree with you more.
Report comment
Selma, Thank you so much for this vital Personalised Medicine information.
Thanks also for your (and your co-authors) publications relating to the importance of psychotropic drug induced AKATHISIA and iatrogenic causation of violence against self and others.
After forty years of medical practice, I have studied psychopharmacology over the last five years.
I have found your own and your colleagues outstanding work and invaluable writings on CYP 450 genomic variants afforded absolutely critical insight and understanding into the behavioural, emotional and psychological toxicities of these drugs.
(In addition to the physical harms, and withdrawal syndromes – which include akathisia).
It is a cause of much devastating injury that prescribing psychiatrists and PCPs not only refuse to accept patient/relative appeals for understanding and acceptance of their ADRs which include akathisia, aggression and violence; but they also misinterpret agitation and akathisia as “symptoms” of deteriorating “mental health” and proof that their “medications” are not only justified, but are needed in greater dosage and in combinations such as SSRIs plus antipsychotics.
They currently appear programmed to ignore the now grossly akathisic patient, pacing and clawing at their skin in front of them.
This is evidenced by recent documentaries which have filmed this phenomenon with psychiatrist and patient totally unaware of the true nature of this intense iatrogenic suffering and its correct aetiology.
There can be no excuse for such dangerous prescribing, nor for lack of awareness and understanding of widespread, individual metabolic variation and biological intolerance of some of the most toxic drugs licensed for human use.
The deaths and destruction of so many could be largely overcome if your vital work became part of the core curriculum of both undergraduate and specialist medical training.
Those who themselves (or whose loved ones) have had their lives destroyed by such careless, casual and naive prescribing are duty bound to alert their own physicians to: –
“CYP TESTING TO HELP PREVENT DANGEROUS ADVERSE DRUG REACTIONS”, and also to urge professionals to read, understand and act upon all the eighteen compelling references you have cited.
You state: –
“The technology for genotyping these five CYPS is widely available and would cover most of these dangerous drugs. I am convinced that once doctors start realising that they are responsible for senseless suffering and that there is a way to, at least, diminish the chances of such horrific side effects as suicide and homicide by a simple DNA test they will fully embrace “personalised medicine”.
Most UK prescriptions for SSRIs and other psychotropic drugs are written by PCPs/ GPs.
The U.K. Royal College of General Practitioners is committed to the doctrine: –
Cum Scientia Caritas: – Care Through Science, or
(With Science – Care).
The recently published deconstructions of paediatric antidepressant trials and the exposure of academic misconduct and malfeasance suggests that the “science” upon which they base SSRI antidepressant prescribing is more science fiction than a valid evidence base for safe, careful and compassionate prescribing.
It seems that few SSRI prescribers are able to promptly diagnose and manage akathisia, even though it is the most dangerous and life threatening of psychotropic ADRs.
They need REAL SCIENCE Selma, and you and your colleagues have now made that real science available to them.
Thank you all.
TRM 123.
Retired Consultant Physician.
Report comment
Very well said! Thank you for posting! Now… if they will just listen… and change.
Report comment
Always appreciate when you point out the drug side effect Akathisia. I didn’t know what it was and I suffered greatly from this drug-induced toxicity. I paced the floor all night, I couldn’t stop moving my hands to touch things, I couldn’t lay down because my body wouldn’t allow it, I shook and it was all due to drug induced Akathisia. My psychiatrist said he was perplexed as I deteriorated more and more into my so-called “mental illness”. What did he do about it? It added more drugs.
Report comment
Aria, I am always amazed at the lack of insight I hear about in the psych field! I cannot believe these are trained doctors and they fail to see the obvious that they were trained to see, time after time. I am amazed that they have degrees displayed on their walls and that they are still allowed to “treat” patients. I am also amazed at the frequency that they claim their patients are the ones with “brain deficiencies” and that patients cannot understand their own shortcomings. Your example points out quite clearly the hypocrisy so widespread in the profession.
Report comment
Aria,
You capture the intensity of suffering which is caused by akathisia with such clarity that it creates a deeply distressing and painful video picture in my mind.
If they learned about akathisia from their patients, they would immediately realise that they are causing, misdiagnosing and exacerbating this grotesque human suffering and destruction as a routine part of their everyday practice.
Then they exacerbate the suffering, toxicity and risk of death by prescribing, often enforcing, more of the drugs that cause it.
It is barn door obvious akathisia when presenting as you describe.
You also capture the appalling diagnostic incompetence and ignorance of psychopharmacology/ toxicology which predominates in day to day psychiatric prescribing.
They will rarely, if ever, be taught the realities, extent, complexities, prevention, emergency management and prevalence of akathisia by their trainers,
or via their “Continuing Professional Development”.
They only learn and believe that which the psychotropic drug manufacturers and marketing departments require them to believe, supported by their anointed Key Opinion Leaders.
Their professional lives are then spent surrounded by neurotoxic, drug injured patients whose evident, acute, sub-acute and chronic akathisia movements and appearance are assumed to be due to the “severity of their mental illness”.
Now they have become diagnostically blindfolded to akathisia.
This form of “PSYCHIATRY IS NOT MEDICINE”.
Julie,
Isn’t it more as if they are trained, or indoctrinated, not to see akathisia?
If it is not too distressing, please see: –
My Baby Psychosis and Me – A lesson in How Not To Make a Documentary. Rai Waddingham. MIA. November 26th 2016.
The link to watch the documentary gives credence to this.
If the agonised pacing feet, in close up in the introduction – and emphasised at 26 minutes is not akathisia, it would be truly astonishing?
Report comment
SORRY FOR DUPLICATION, I was unable to delete.
Aria,
You capture the intensity of suffering which is caused by akathisia with such clarity that it creates a deeply distressing and painful video picture in my mind.
If they learned about akathisia from their patients, they would immediately realise that they are causing, misdiagnosing and exacerbating this grotesque human suffering and destruction as a routine part of their everyday practice.
Then they exacerbate the suffering, toxicity and risk of death by prescribing, often enforcing, more of the drugs that cause it.
It is barn door obvious akathisia when presenting as you describe.
You also capture the appalling diagnostic incompetence and ignorance of psychopharmacology/ toxicology which predominates in day to day psychiatric prescribing.
They will rarely, if ever, be taught the realities, extent, complexities, prevention, emergency management and prevalence of akathisia by their trainers,
or via their “Continuing Professional Development”.
They only learn and believe that which the psychotropic drug manufacturers and marketing departments require them to believe, supported by their anointed Key Opinion Leaders.
Their professional lives are then spent surrounded by neurotoxic, drug injured patients whose evident, acute, sub-acute and chronic akathisia movements and appearance are assumed to be due to the “severity of their mental illness”.
Now they have become diagnostically blindfolded to akathisia.
This form of “PSYCHIATRY IS NOT MEDICINE”.
Report comment
Selma,
This is a very serious question which I just don’t know the answer to, and can’t even think about how I might answer it for myself. Maybe I *AM* “over-thinking” it, and maybe not!
In talking about these CYP450, etc, the current (Western Industrialized) system of nomenclature you’re describing uses “Roman”, and “Arabic” numbers and letters, in both upper and lower case, etc.,
Just how widespread is this scheme, globally? Does China, say, or Indonesia use the EXACT same system, or are there differences? I can see how easily confusion might arise, with different nations, countries, languages, etc, getting involved. India has literally many “Official” languages, for example. How well does this translate into ALL of them? You see where I’m going with this? It’s making my head hurt, trying to learn just what’s presented above! I’d have to spend at LEAST a couple hours serious study, just to understand what’s presented here in your article, above.
Yes, I get the basic gist of it, but the technical details are above my formal education.
Also, a related question – it seems to me, that if America, let alone the “Western World”, adopted wide-spread genetic testing for possible “genetic contraindications”, which is what this article is basically leading to, – wouldn’t we see that *YES*, psychiatry *HAS* been grossly over-drugging some people?
Psych drugs did me FAR MORE HARM than good. That’s true for far too many OTHER VICTIMS.
I’d like to see at least some answer, here, Selma, THANK-YOU! ~B./
Report comment
The system of naming these enzymes is globally the same. That is why “pulpamor”, see below, had identical results in Mexico and the US. If she/he would go to China, the results would still be the same. I agree that doctors – and not only psychiatrists – prescribe way too much medications. By doing the CYP testing the damage might be reduced.
Report comment
Yes. It is an international nomenclature. China, upper Mongolia, Iran, Greece and Bosnia all produce population studies. Australian psychiatry is informed by professors funded by pharma and regulators are advised that it is nonsense. President Bush gave it $10 billion and there are huge curated data bases. Obama talked of Precision Medicine in his penultimate State of the Nation address. It gets 1.8 million hits on Google, and hundreds of thousands of hits on Scholar. It is the bedrock of personalised medicine. Craig Venter, Mr Human Genome, pointed out that drug companies do not want doctors knowing it as they make more profits if we don’t know. One size does not fit all. Watch for pharma shills. An eminent Australian psychiatry professsor told me in front of 400 people: I have done two tests and I think pharmacogenetics is nonsense. The test has limited utility unless you know drugs,doses, age, gender and general health of the patient. For forensic purposes. However it flags a possible problem if done before prescribing.
Report comment
I’ve have a great deal of queasiness concerning this sort of cyborgized medicine. Specifically, I question whether assimilation into The Borg is the best of all possible goals for our species to strive for.
Personalized medicine is a problem only in so far there is any question as to whether the individual being treated actually has a medical condition, and this issue has never been adequately resolved in the case of psychiatric disorders, however here is another ingenious method for a medical technician to make money, and a patient to feel necessary…as a patient, that is, a perpetual consumer of medical technology.
Regardless, we know what the effort, ‘one size’ or many sizes, is directed at, assimilation into The Borg.
Report comment
“Patients are seldom put on just one drug.”
Yep, drug cocktails are certainly an issue with me, especially when they contribute to a person’s, excuse me, “dysfunction” and early death.
I think we have a real problem with the drug, drug, drug mentality in psychiatry all the way round. The way to health is not through drugs. This post, although well-intentioned in many respects, with the hope of limiting potential harms, plays into the predominate paradigm IMO. I just feel like you’re taking designer drugs to a whole nuther level (What? Drugs to suit an individual’s genes?) when maybe drugs are not the best answer to ‘problems in living’, and going there, despite the demand, is problematic in and of itself, at least for me, alcohol and weed nonwithstanding. I think certainly, in some instances, it might have a positive effect, but in general it’s just another way to maintain patients on drugs, drugs that are ultimately damaging. I think we need to work on changing the paradigm, and that’s not what I’m seeing here.
Report comment
Frank, I concur.
While CYP testing is a step forward from the haphazard and careless prescribing habits I see today, it is still just another step in “finding the right drug” instead of finding a solution, or a method of coping or surviving a difficult time.
When CYP testing becomes rampant, er, “standard procedure,” the drug companies will all struggle to find drugs which are not metabolized by the CYP system at all, and we will find new metabolic pathways to destroy by drugs. Oh joy. A new generation of “safe drugs,” a new generation of disconnect from emotions, and side effects that nobody believes in because “these drugs are safe for you.”
Just like the last ones were touted to be.
Feel like Don Quixote sometimes.
Report comment
Why are there drug pushers on this forum? All we need to know are the proper procedures for safe disposal. If people are acting like these drugs might be ingested, then they are still taking the view that the drugs are helpful and that mental illness is real.
Nomadic
Stop Collaborating With the Mental Health System:
http://freedomtoexpress.freeforums.org/fighting-to-eradicate-the-mental-health-system-and-incarcerate-the-practitioners-f2.html
Report comment
Problems with P450 enzymes are only one source of adverse drug reactions. Genotyping might help prevent the accumulation of too much drug and therefore prevent some bad side effects. But can’t even desirable levels of a drug wreck havoc with the body? For example, a statin may lower cholesterol, but since cholesterol is used by every cell in the body can’t that cause severe disruptions? And might not the increased level of seritonin in the brain caused by taking an SSRI cause unforeseen problems even at drug levels that are deemed desirable.
Report comment
I totally agree. We don’t even know what a desirable level is or whether there is a desirable level. I recommend CYP testing to at least get an idea about what not to prescribe.
Report comment
Absent any correlation between blood level and adverse effects, how is this supposed to screen for potential adverse effects?
Report comment
Um, isn’t the idea that certain genetic configurations mean the person might be a “slow metabolizer”, and thus the “therapeutic dose” could build up to toxic levels?
Or that a “fast metabolizer” could excrete the drug too fast to be effective? That’s what *I* think this is saying. I mean no personal insult, Stuart, but aren’t psychiatrists first MD’s? (yeah, I know, “sorta”….) Based on my empirical experience, some drugs are toxic at “therapeutic levels”, and the “tranquilizing effect” masks the damage being done. The psych drugs I was given, did me far more harm than good. The drugs actually *caused* the very “symptoms” that I was supposedly being “treated” for…. Have you been paying attention here?
“Precision medicine” is nothing more than the “PhD/MD Elite” monetizing their retirements, at the taxpayers expense. And on top of the bodies of the PhRMA-drugged victims. As has been noted elsewhere, there is NO serious discussion, in any detail, about exactly what the “therapeutic effects” of psych drugs actually *ARE*….(They most benefit the banksters, and the medical mafia….
Report comment
ADRs correlate well with genotype. They occur on toxicity as well as on sudden changes up or down. Side effects like suicidality persist well beyond five half lives it takes to clear the drug. Five weeks to 81 days for Prozac. No drug in body. Pill taken 8AM produces different blood level after different periods. And higher levels in reduced metabolisers. Danger periods on starting and fast stopping. Blood levels and doses of two drugs can be normal but they might be synergistic for ADRs. Steady state is a myth. IMs are at greater risk than PMs as side effects creep up unrecognised and are not as dramatic as PMs. Most at risk of suicide or death from intoxication are UMs. They die from prodrugs like Tramadol and oxycodone and from drugs with toxic first metabolites. And respond to nothing.
Report comment
CYPs are also expressed in the brain. We don’t know the levels of drugs in the brain.
If we know someone has polymorphisms which lead to altered levels in the blood, we also know that person has problems with levels in the brain, so we can adjust the dose or not give drugs at all.
Report comment
I am organizing a Precision Medicine Symposium in the Houston, TX area on May 6, 2017. Are you available for speaking engagements? We would love to have you talk about this subject in particular… Please let me know. Thank you!
Report comment
Hi, where can I find information about this symposium?
Thank you for your reply
Martha
Report comment
Hi Martha. We are designing the webpage and content right now. If you wish, you can send an email to [email protected] and I can forward you the info when it is complete.
Report comment
I’ve had my CYPs analyzed in two countries: Mexico and the US. I was first introduced to this genetic testing while I was studying in Mexico City. My medicator insisted that he get the results before prescribing anything to me and he was surprised to learn that it was not common practice in the US since we pay an arm and a leg for healthcare. I went to one of the research hospitals in Mexico City and got the genetic testing for around $550. Mexico is where I was introduced to this study.
When I returned to the US, I need to find a new prescriber. After 9 years of being on psychiatric drugs in the US, this time the prescriber insisted that he know my CYPs. I told him that I already had the results, but he was skeptical and didn’t believe that the results from one of Mexico City’s leading research hospitals could be correct. He was in fact incredulous. He insisted that I redo the genetic testing, so I did. And, I admit that at the time my medicator was skeptical enough that I started to doubt the validity of my results. Well, the results came out to be identical! The cost to have it done in the US was picked up by insurance, so I don’t know what the real cost was.
Perhaps if I’d have did this information when I started psychiatric drugs, it would have spared me from some of the absolutely horrendous experiences these drugs can and do create!
Overall, however, I find this CYPs a waste of money and resources unless you’re willing to mess around with the never-ending trial and error game. For me, the results came when I was exiting psychiatry’s revolving door.
in the US didn’t believe the results that I had
Report comment
I agree, great article, I hope you will continue to research drug interactions, and absolutely believe every doctor should be legally required to give “a simple DNA test,” prior to prescribing, especially, any of the psychiatric drugs.
Today the medical community believes that if your grandmother was briefly given Stelazine, and quickly taken off of it due to a horrendously adverse reaction to that neuroleptic, then you must be given every single new neuroleptic on the market, plus lots more drugs, prior to being weaned off the drugs due to extremely, likely genetic, adverse reactions to the psychiatric drugs. And today’s psychiatrists also believe this gives them the legal right to unjustly defame your grandmother in your medical records, as well, which is disgusting and easily disprovable. Although I’ve since learned this is also because the psychological and psychiatric industries, historically, have enjoyed profiteering off of defamation of women to cover up medical evidence of child abuse, too. This unethical behavior should end.
But I’d love to see you do this type of comparisons of drug interactions, especially on all of the “bipolar” drug cocktail interactions, since the likely drug interaction sites the doctors utilize, and the Federal government ones that are available to us “regular people,” are so poor.
It wasn’t until the third “bipolar” drug cocktail I was put on, all of which made me “psychotic,” that I finally found the medical evidence that combining the antidepressants and/or antipsychotics actually causes “psychosis,” via anticholinergic intoxication syndrome.
And to this day, anticholinergic toxidrome is not listed on most of these drug interaction antidepressant and/or antipsychotic drug cocktail drug interaction sites, nor is it listed in the DSM as a possible cause of “psychosis” when prescribing the recommended “bipolar” drug cocktails. No doubt, this is causing as much iatrogenesis, as the massive misdiagnoses of the adverse effects of the ADHD drugs and antidepressants, that resulted in what Robert Whitaker pointed our as the American “childhood bipolar epidemic.”
As a “regular person,” with only a BS and a BA listed after my name currently, but as one who did also get in the top 99.95% of my math SATs, so I’m probably “genetically” smarter than most of today’s doctors. I’ve tried to point out to the Mayo Clinic that their current “bipolar” drug cocktail recommendations, especially combining the antidepressants and/or antipsychotics, is unwise, to no avail.
As a doctor, perhaps you may be able to medically explain to the psychiatric industry better than I, that combining any of the antidepressants and/or antipsychotics can make a person “psychotic,” via anticholinergic toxidrome? And misdiagnosing anticholinergic toxidrome as “bipolar” or “schizophrenia” or “borderline” is iatrogenesis, not “proper medical care.” Especially when it comes to the psychiatric and psychological industry’s desire to cover up the pedophile crimes of our sick, current world leaders.
Report comment
Educating the patients is just as important as education the prescribers. Both should be aware there are other, better ways to help people in psychological need. By doing the CYP testing as a doctor, or by demanding it as a patient, there is some objectifiable evidence why pharmacotherapy can go so horrible wrong. It is a way to prove the iatrogenesis.
Report comment
Even now, into my 36th month of significant impairment after quitting Klonopin? I’m sure the many other psych meds over the last 10 years didn’t help, either.
It would be *wonderful* for this iatrogenic damage to finally be acknowledged, at the very least, and compensated for. Really, I’d much rather have my life back…and with no end in sight, at times it’s hard to hang on.
Everyone on BenzoBuddies (<30,000 registrants) and Surviving Antidepressants would like some *proof*, I'm sure. Because right now, as it is, no one believes us.
Report comment
Cnsidering commercial interests involved, I would like see disclosures regarding this author. In addition to fees for court testimony, any consulting relationships with the companies doing this testing? Given Whitaker’s writing on COI, these disclosures (presence of absence of them), would be helpful.
Report comment
Good point.
Report comment
Fair point! I seldom get paid for the work I do on a CYP investigation. I work for the defense, who’s clients are either in prison or in a psychiatric hospital. Sometimes the court pays or a client who can afford it, but most of the time I pay for the testing and the report from my own pocket. So I have no conflict of interest.
Report comment
But you do get paid for your services as an expert witness, don’t you?
Report comment
Most of the cases I work on don’t go to trial. If they go to trial, it is still no guarantee I get paid. Sometimes I get paid only for the few hours I testify, not for the testing or the time it took to wrote the report. In 2 cases the court paid me for both.
Report comment
Another question I have concerning genotyping is the extent to which it would add to preventing adverse drug reactions over what is already available. Physicians can easily access information on drug-drug interactions (although, unfortunately many don’t do this). They should also take into consideration a patient’s age when determining drug dose (also not always done). If another test is going to be added to the numerous tests Americans undergo it should be cost effective. And the genotype test itself should be tested to see how well it works in practice, not just in theory.
Report comment
I use the CYP testing in cases where violence as a side effect had been occurred. From what I have learned so far it is clear that had testing been done the side effects were predictable.
Report comment
Dear Dr Selma,
I was nearly killed several times by the drugs below in the early 1980s in Ireland (and have 30 years of Solid Recovery as a result of stopping them).
From the LINK below :- E. Fuller Torrey.
“….Dosage, however, is a critical issue. It seems to be sometimes forgotten today that there are huge differences in how individuals metabolize antipsychotic medication. For example, a study published in 1982 reported that when a group of patients with schizophrenia were each given 20 mg of fluphenazine, the difference between the highest and lowest blood level of the drug was 40-fold…….”
http://www.psychiatrictimes.com/psychopharmacology/better-without-antipsychotic-drugs
AND:-
A 1983 Study on Fluphenazine, Suicidal Reaction and Akathisia, from Dr Allen Frances and others.
https://www.researchgate.net/publication/16313058_Suicide_Associated_with_Akathisia_and_Depot_Fluphenazine_Treatment
Recognition of this in prescribing could definitely save lives, but I don’t see psychiatric drugs as medicine, and I don’t think there’s such a thing as a suitable dose.
Report comment
Many patients don’t want to go without drugs. Those are the ones that could benefit from testing, at least in the sense that they might not be put on medication that increases the changes of violence as side effect.
Report comment
Thanks Dr Selma,
I understand what you’re saying.
Report comment
I believe this Irish Phenomenon to be ‘medication’ related.
https://www.google.co.uk/amp/s/www.irishtimes.com/news/ireland/irish-news/murder-suicide-now-a-regular-phenomenon-1.2772334%3fmode=amp
“…..Murder-suicide appears to have become a regular phenomenon of recent years, said Deputy State Pathologist Michael Curtis in 2013 when a study on dyadic deaths was published. …”
Report comment
This suggests that risk of violence is dose related. What is the data to support this? This seems potentially helpful for reducing risk of QT prolongation which is a dose related phenomena.
Report comment
Not all adverse drug reactions are dose related. Consensus is that the higher the level, the more chances of side effects from toxicity. But they can occur at low levels as well. When someone is in withdrawal and there are no levels of medication at all, the effect on the brain chemistry is still there.
With regard to violence the changing blood levels are very dangerous.
Report comment
Pardon my cynicism, but even if these tests are accurate that doesn’t mean shrinks will want to use them. They’re probably too expensive and time-consuming. Therefore this would eat into the profits.
Furthermore, if a lot of people are shown to have genetic sensitivities to these brain drugs, how will the psychiatrists be able to prescribe the poisons they so sorely need? And bill Medicaid for it?
My guess is, if there is any merit to these tests, the pharmapsychiatry mobsters will hush it up. Profit is everything to them.
Report comment
I can understand why you feel discouraged. But chance will come from the bottom up. If a patient or a family member speaks up, the prescribers have to listen. I have done many cases where patients or relatives warned their doctors the medication was making things worse. By asking for a CYP test they can force the doctors to become aware of the dangers involved in (any kind) of medication.
Report comment
I think this is extremely important but I don’t think should be used in everyday instances to encourage drugging or to increase use of the Medical Model. I do think, though, that for those who have already committed violent acts and are involved with the courts, who are in prison for these acts, who are awaiting trial, who are stuck forever in the mental-penal system, or the “I didn’t really do it because I am insane and now I’m locked up forever” system, yes, this could very well be crucial information that could tip a court case one way or the other. This information could also be used in cases where the victim committed suicide, and families are seeking justice. Wasn’t there a story on here recently about a woman who killed her child after taking psych drugs, and is now locked up? The story was posted by her therapist, and that was recent. Monica Casani reposted the story in her blog as well. And Reid Bertino, too, perhaps this information would be helpful. Any of these folks and their attorneys can use this information. Or even suggest the *possibility* to the courts! And if the author is available to testify, this, too, would be extremely helpful to those who are locked up.
Report comment
Julie, it is vital that those who have allegedly “committed violent acts”, entirely as a result of professional failure to recognise prescription drug induced aggression, violence and toxic delusion, are afforded access to CYP 450 genomic sequencing.
I believe that the “patient” value is far wider than this.
It takes great courage and the highest professional integrity for any doctor to challenge the psychiatry establishment and the vast commercial interests which drive the current, widespread abuse of psychotropic drugs.
SSRI induced psychosis, mania, agitation, aggression and akathisia are NOT DIAGNOSTIC of “Bipolar Disorder” or “Schizophrenia”; they are manifestations of IATROGENIC NEUROTOXICITY.
The mis-diagnosis of these common psychotropic Adverse Drug Reactions (ADRs) –
with defamatory labels-for-life, imposes an unbearable life and soul destroying tragedy upon individuals, their loved ones and their families.
It is by abuse of extreme powers, so inappropriately vested in psychiatry, to ignore basic ethics and basic human rights;
By abuse via incarceration, coercion and enforced drugging of normal, healthy people: – that extreme levels of fear, indeed terror are generated.
It is this terror of repercussion, and of even greater and more prolonged abuse and injury, which negates protest and complaint.
This terror denies entirely valid malpractice litigation.
Thus is denied any hope of justified, high level financial redress.
SSRIs cause: – Emotional Blunting, Akathisia, Disinhibition, Aggression, Violence, Homicide and Suicide.
Without routine CYP 450 genomic sequencing, these ADRs will continue to be routinely misinterpreted by psychiatrists.
Without routine CYP 450 genomic sequencing there is no driver to limit, decrease and cease the marketing-driven, abusive and excessive prescribing of these profoundly toxic drugs.
“I believe the SSRI era will stand as one of the most shameful in the history of medicine”.
Genomic sequencing affords the opportunity to expose this shame.
This technology not only affords all of us a vital opportunity to limit and control the catastrophic individual and family destruction caused by the extensive, cavalier prescribing of SSRIs and other psychotropic drugs: –
It also affords the opportunity to challenge the routine, day by day psychiatric misdiagnosis of neurotoxicity as “Serious Mental Illness”.
There is now a forensic scientific methodology which at last provides an opportunity to define, quantify and challenge this misdiagnosis.
There may at last be a “calling to account” via evidence based malpractice litigation.
At last, an opportunity to reverse the obscene power imbalance between prescription-drug-dependent psychiatry and abused patients.
Potential to tip the current imbalance of power in favour of compassionate and intellectual patient care.
“Generating a profile of these CYPS” – ( CYP 1A2. CYP 2C9. CYP 2C19. CYP 2D6. CYP 3A4. ) – “will provide the physician with valuable information”.
Agreed, – however the information thus provided to the patient will be often, albeit not always, invaluable.
CYP 450 genomic sequencing is the first available scientific tool which empowers the patient and the patient’s advocate.
It is up to all of us to demand, and to ensure that this invaluable asset is used to the very best possible patient advantage.
Finally; – The words of Arthur Schopenhauer. (1778 – 1860)
“All truth passes through three stages.
First it is ridiculed. Second it is violently opposed.
Third, it is accepted as being self evident”.
TRM 123. (I have no conflict of financial interests).
Report comment
So after all these years they finally pin this down. I am asking, is this the tip of the iceberg here? And now we know about one specific extremely serious genome sequencing problem that will produce results such as violence or death, could there be other genetic or drug-drug disasters yet to be uncovered? I truly believe that even if years back they couldn’t pin it down specifically, surely they knew all along there was a very serious problem, perhaps an unpredictable one. They were well aware that prescribing SSRI’s was like roulette, they knew SSRI’s COULD cause mania or psychosis and acted like they were blind to it, or lied and claimed it was rare, or claimed the usual lie of “underlying condition” since this is the Grand Malpractice Default Mode. If all else fails, Never Admit You Did It. It was Mr. Mustard in the Kitchen with the Lead Pipe.
Report comment
You are absolutely “on target” here Julie.
“Surely they knew all along there was a very serious problem, perhaps an unpredictable one”. “They were well aware that prescribing SSRIs was like roulette – ”
Please see, or re-read, MIA post by David Healy. March 6th 2012.
“BREAKING SCANDAL”.
Also: –
“ZOLOFT STUDY, MYSTERY IN LEEDS”.
David Healy’s own Blog, February 26th. 2012.
This relates to an abandoned, 1983 – (phase 1). Trial of Sertraline in healthy volunteers.
“All of the sertraline subjects had problems, as had one of the placebo subjects. The placebo subject having problems, however, had sertraline levels in her blood, making the findings even more convincing”.
“The side effects that seemed most clearly linked to sertraline
were apprehension, insomnia, movement disorders, and tremors”.
“There were wonderful descriptions of AKATHISIA:
– the mechanism later linked to suicide induction on SSRIs”.
These side effects had been described previously – – “they were well known to be linked to SSRIs, and that as such these effects in this study were likely to be due to serotonin re-uptake inhibition”.
Hence, this devastating toxicity would appear to have been deliberately hidden by SSRI manufacturers, apparently in collaboration with their Key Opinion Leader – (KOL) psychiatrists for over THIRTY FIVE YEARS.
How many deaths and destroyed, yet once beautiful and successful human beings could some basic academic rigour, and basic professional ethical integrity have prevented?
How much iatrogenic, misdiagnosed, entirely SSRI-INDUCED, yet alleged by “experts” to be “Serious Mental Illness”, could have been avoided?
WHERE WERE THE REGULATORS OF BOTH THE MEDICAL PROFESSION and DRUG LICENSING?
Gazing down the wrong end of Nelson’s telescope perhaps?
Hence it is surely worth re-stating the quotation: –
“I BELIEVE THE SSRI – ERA WILL STAND AS ONE OF THE MOST SHAMEFUL IN THE HISTORY OF MEDICINE”.
TRM 123.
Report comment
When a client goes into a psychiatrist’s office they are automatically suspect of not being believed. This is the beginning of a messed up doctor-patient relationship because any drug-induced toxic effects will not be seen as what they really are. It’s much easier and profitable to watch the patient become more incapacitated then it is to put the effort into why in the world is this poly drugged client has become incoherent? Stupidity. Even more once the client comes off the drugs they’re not mentally ill. What is the explanation? They call it recovery when it’s really surviving psychiatry.
Report comment
Yes, and I am wondering also they have KNOWN all along that SSRI’s cause sleep disturbance. Whether they knew the precise mechanism or reason doesn’t matter. They were well aware of the association and they have known this for decades. They have also known that these sleep disturbances, plus the akathesia-like agitation (similar to to the pacing from thorazine-type drugs) either one of these could cause an agitation which could drive a person to suicide. Again, knowing the exact reason wasn’t as important as the fact that they were aware of it, well aware, and LIED. DENIED that they knew the association. And people have died. Not a few, but thousands, and tens of thousands have been put out of work and even more dealing with chronic pain issues and facing issues late in life, god-knows-what, such as impending dementia issues we don’t even know of what proportions. With even more now on these high-test stimulants, the problem magnifies further.
I am reminded of the old Star Trek, when Captain Kirk reminded us, again and again, that there were certain realms where Man simply should not go. While it may have been amazing that the Star Ship Enterprise explored where no man had gone before, he always reminded us, often around the end of many of these short TV episodes, or Spock would, that there was a limit, that there were places where they needed to lay off. I think we’ve reached some of those places right here.
Report comment
1boringoldman had a very good article (November 30, 2016) on Akathisia. One of the components was ssris can cause insomnia. Seroquel caused off the charts Akathisia so how in the world was I supposed to sleep? How can any psychiatrist not get the fact that these drugs are neurotoxins?
Report comment
Sorry, you do not think this should be a everyday instances, but only for those who have already committed violent acts and are involved with the courts. Why should you wait for someone to commit a crime? How about the lives you can save before the crime is committed? Are these worthless? I think CYP testing is something doctors should be doing before prescribing their patients. Don’t get me wrong I am against most meds, but when they are prescribed I would like to see it is done with some sense.
Report comment
This is a GREAT article and very easy to understand. Thank you… I will be sharing this with many, many people (both professionally and personally)!
We just received results for my husband’s Pharmacogenetic (PGx) test this past week. 25 genes were tested. While he is not on any psychotropic medications, he does take cardiovascular medications (statin & high blood pressure). VKORC1 shows a “High Warfarin Sensitivity”. We will put that information in our back pocket should a physician (or hospital) want to prescribe that for him one day.
The reason we got my husband tested is for an upcoming surgical procedure. Last February he had a similar procedure and came out of the anesthesia in an extreme amount of pain. The nurse did not understand as the pain medicine given during the procedure (Morphine) should have been strong enough “to last until he got home and was able to get his pain medicine prescription filled and the first dose taken”. That was not the case with him. They wouldn’t give him anything for the pain after the surgery (even though he was shaking and crying) so he suffered until we got the prescription filled. However, that medicine (Hydrocodone) didn’t work well either. While it seemed to work initially, it wore off quickly and he suffered quite a bit. I called the surgeon on a Saturday begging him to call in something stronger but he could not. He instructed my husband to take 2 Vicodin every 4 hours rather than only 1 every 4 hours. It was a horrible recovery. The increased dose caused him to sleep a lot and gave him horrible constipation which delayed his recovery greatly, causing him to take additional time off work.
A year prior to this, in February of 2015, while consulting with an Alzheimer’s facility, the Director of Nursing told me about pharmacogenetic testing. A patient with Parkinson’s was having violent outbursts and the family was required to hire a 24 hour private duty caregiver, on top of the $6000 per month fee for the facility. The results came back identifying one of the drugs given to most Parkinson’s patients was not being metabolized normally in this gentleman. The patient was taken of that drug and his behavior improved. The 24 hour caregiver was no longer needed and the patient was able to stay in the facility. Not only did this save the family thousands of dollars, the patient’s quality of life greatly improved. At that time, only a psychiatrist was able to order a PGx test and most commercial insurance companies did not cover it. Later that year I attended a luncheon where the guest speaker was talking about pharmacogenetic testing and how it was going to change the way we practice medicine. While definitely intrigued by the science and implications, I still did not get involved.
In July 2016, I came across pharmacogentic testing again and began doing a LOT of research. I had been in healthcare for over 25 years and worked as a geriatric care consultant for 13 years so initially I was interested in PGx because of the number of drugs many of my elderly clients took each day. The more I learned, I realized this test was beneficial to ANYONE taking a prescription medication and should actually be done BEFORE ANY medications are prescribed.
As for my husband, after learning more about PGx, we suspected that the genes responsible for processing pain medications must have mutations and INSISTED his PCP do a test on him before his next surgical procedure. I found a lab (after much research) and even took the test and a lab representative with us on the appointment to collect the cheek swab sample. The results CONFIRMED our suspicions. According to his PGx/DNA test results, my husband has an “Altered Response” to Morphine (the drug used during surgery) and the report states “The patient may require higher doses of morphine for adequate pain control.” ALSO, “Altered Response to Hydrocodone” (the prescription for post surgery recovery) with the report stating “Acute postoperative and cancer pain: the patient’s genotype has been shown to be associated with reduced analgesia and increased opioid side effects at standard or high hydrocodone doses. If the patient fails to respond to increased hydrocodone doses, an alternative opioid may be considered.”
There were many other drugs with cautions but these 2 were the ones we needed to know about right now. He can now take this report to his surgeon BEFORE his procedure this month and have PROOF that those pain medications do NOT work for him. Hopefully, we will avoid the horrible post surgical recovery experience we had last year. The lab we used also gives a list of medications that DO work for my husband so we can choose one of those from the list.
Cautions were also given on several psychotropic medications including Zyprexa, Cloazril and Xenazine. While he does not currently take any of those, it is still good to know. Diabetes, Gastrointestinal, Infections and Urological drugs were also covered in the test (in addition to the Pain, Psychotropic and Cardiovascular drugs).
For some reason there is still controversy around PGx testing but the science is REAL. Mayo Clinic has been using this science for years. https://vimeo.com/user49365795/review/159289338/b3e3adae99 St. Jude’s Children’s Hospital now tests ALL new patients upon admission. Many, many other well respected hospitals are using this test and more and more physicians are getting on board.
If you are not convinced of the benefits of PGx testing, it is because you still do not understand it or you just don’t want to. As Mary Relling, Chair, Pharmaceutical Sciences Department, St. Jude’s Hospital stated, “If you knew about this genetic information and you did not act on it, you would not be practicing good medicine.”
Do the research. Get tested.
Report comment
I would like to know if there are any articles out there that show the science behind why people get the most horrific insomnia from antipsychotic drugs (I was on three at once, at the highest possible doses) or pretty much from any sedating drug if taken (prescribed, ha ha) over a long period. I never needed antipsychotic drugs, at all. The insomnia I have had has been comparable to narcolepsy. I cannot describe it in any other way. This has nothing to do with “racing thoughts” nor “my mind won’t stop.” I cannot attribute it to nightmares nor “anxiety” nor does it ever change from one night to another. The only time it improves is if I am completely sleepless for a lengthy period, only then will I have improved sleep. My average, for five years, was about an hour of very light sleep, no dreams, per 24 hour period. I couldn’t believe I did not go into organ failure after that but I was going into mini-sleeps during the day, including while waiting in line at stores, while in waiting rooms, while standing or sitting on bus rides, in ticket lines, and even while walking I felt afraid I would fall asleep, nod off, and fall down. I also lost track of what i was doing and was forgetful, and couldn’t get organized, got lost in stores and lost my way frequently. I did find a solution. Caffeine. I use it to stay awake all day to avoid mini-sleeps, then, a tiny bit, subclinical sedation at night, just to get myself perhaps four hours. I can function now, but I wish I could SUE or something! And I’m wondering if the drug-induced narcolepsy is permanent or whatever. I never went to a doctor, either, I hate the whole profession and I am terrified to see an MD at all! I just figured this out by putting two and two together and doing a lot of reading. I’m very happy to be able to function at least and not worry about my safety in traffic, but it’s not ideal.
Report comment
Julie,
My sleep has stayed interrupted since I’ve been off all the psychiatric drugs for 10 years. There are so many nights I can’t go to bed till the sun comes up. I’m too exhausted to read or do any other activities so I choose to lay in bed quietly in increments. I have met other people that were on psychiatric drugs and they live a sleep-deprived life.
I don’t know where there has been any research on post psychiatric drug disruptive sleep pattern? Like you I don’t go to doctors about it because they don’t have anything to offer me except drugs. If you find any concrete info about this please see it makes it to MIA for others to read.
Report comment
I’m not sure there has been much post-psychiatric drug use research done at all. 🙁
Right now I don’t have insomnia. I’m physically tired all the time, and often lie down. My body feels EXHAUSTED but my mind keeps going. Still sleeping at least 7 hours a night, but my body craves rest more than my brain. Very weird.
Report comment
Might as well add I’m still taking 60% of my original effexor dose. 90 mg rather than 150, and going down.
Don’t know what the end results of my “experiment” will be. Wish I had some help–offline.
Report comment
So glad you mentioned that. One of the biggest factors which PROVES that psychiatry is nothing more than a pseudoscience drug racket and means of social control, – but NOT a legitimate medical specialty – is the FACT that there is almost NO follow-up care for drug effects, or so-called “side effects”, and almost no research. There’s NO hard data about what drugs do or don’t do, long-term. Population health studies DO show that so-called “mental patients” on psych drugs live an average of 25 years LESS than the regular population not on psych drugs. For the 1st time recently, average American life spans showed a slight decrease. Not very optimistic!
On the OTHER hand, check out >beyondmeds.com<. Monica Cassini does a good job with that website.
Off-line? It's very easy to meet people off-line. Coffee shops, church, stores, on the street, various public activities – anywhere there are people, you can strike up a conversation. People always respond well to a smile or kind word.
Just today, I saw an older Navy Veteran wearing a hat showing the name of his ship. A brief comment led to a 10-minute VERY nice conversation! It might seem a daunting task, what I'm suggesting, scary even, but I think you can do it.
You can always call an 800-number suicide hotline, just to talk. You don't have to even say you're suicidal. And NEVER tell a shrink you're suicidal, even if you are! 😉
That's as much as I got right now, FeelinDiscouraged, online. But see what I mean? If you reach out, *some*body* will usually respond…. ~B./
Report comment
Aria, This is my guess. Those of us who have been force-disabled by drug-induced insomnia were generally long-term users of psych drugs. My guess is that most long-term cocktail-users were on the disability rolls to begin with. So who will care? So what if we’re made worse disabled? We weren’t making big paychecks. They aren’t anticipating many lawsuits from those whose lives were already wrecked to begin with. What was the monetary loss? In court, nothing. They don’t give a shit about a mental patient’s quality of life. Now you take a father of four who makes 80,000 a year and give him the exact same drug-induced narcolepsy, that will make it to the courtrooms. Especially if he blows his his head off and takes a few kids in a convenience store with him. And leaves a suicide note saying he can’t sleep and is too exhausted to work because of the drugs he was given and his life us ruined. Maybe then someone will care but no one cares about nutcases. There’s no money in it.
Report comment
Sometimes I wonder, too, since we matter so little, since the reality is that it doesn’t even pay to represent us legally in court, which means we are truly unwanted and devoiced, my guess is that thinking in broader terms these mass shootings represent a desperate attempt of those who were formerly forced into silence to be heard. Drugs do a good job of silencing. Diagnosing discredits a person, weakening or disempowering everything they say. Incarceration or forced appointments (keep the person busy with play-doh) also silence people. Many of us are angry over the the denial and overall refusal to believe us. Many are desperate to to be heard and believed, desperate enough to get very loud I’ll bet, if pushed to the limit.
Report comment
Thank-YOU!, Julie. You’re telling my story, too. You speak the truth.
We need to realize, that psychiatry, and their poison pills, and PhRMA, represents a form of CHEMICAL WARFARE, against a CIVILIAN population. Repeat: A form of chemical warfare against a civilian population. A psych diagnosis is the same thing as a criminal sentence of “life without possibility of parole”. I’m very active in my hometown, and have well over 20 years both alcohol sober, and Rx drug-free. I’ve done my best to help other hurting and disabled folks, but too often, the “system”, and the local “community mental health center”, treat me as if I’m a “dangerous crazy person”. I have made a point of going out and meeting, and maintaining good relationships, with several key persons. That includes cops, City Council, and other local “movers and shakers”. Oh, they “respect” me, alright, but would rather not have to deal with me. I tell the truth, the *TRUTH*, that they don’t want to hear. It’s hard, very hard. But, I do have a good life, and I’m happy with who I am. But I still have IATROGENIC NEUROLEPSIS. That will NEVER go away. Psychiatry is a drug racket, a pseudoscience, and a means of social control. And it’s a form of chemical warfare against a civilian population. *WOOF* to Puzzle, aria, and my other friends here. HAPPY TUESDAY! ~B./ 😉
Report comment
FeelinDiscouraged,
I strongly doubt there is any post psychiatric drug research because psychiatrists don’t want to know we exist. My psychiatrist could not come to grips with the fact that the lower the drug doses I was on the more coherent I became. As I slowly became the old me (psychiatric drug free) my family and friends were delighted and our relationships became stronger.
A good site for tapering and support is “surviving antidepressants”. Good luck with your tapering.
Report comment
Thanks, Aria. (Already belong to SA.) I agree that psychiatrists are in denial. Most have to deceive themselves or the guilt would drive them madder than their victims. Others are sociopaths who lie to everyone else and feel no empathy for the folks they hurt.
Because my Mom thinks “mentally ill” folks who are non-compliant with “meds” behave in irrational, impulsive and often dangerous ways she can’t see what I’m doing under her nose. Even though we live together in a single wide. She can’t understand why I itch all the time, feel exhausted when I get up, ache almost unbearably, have a cough, and developed dry eyes recently. Why? The media doesn’t portray going off psych “meds” that way. Due to program sponsors and their abilify cartoons TV writers that aren’t deceived have to deceive or find another job.
I take one drug now. 90 mg of effexor–I remove 40% of the tiny balls from the gel capsule every morning with one real medicine to supplement thyroxin my body doesn’t make. Mom sees me take these pills in the morning. At night she sees me take a fish oil capsule and a zinc tablet and assumes their pills. Because I have always been a rule-abiding conformist who took her “meds” exactly as prescribed my folks still trust me. Needless to say I hate lying to them!
The only reason I continue to go off, is I believe it’s wrong to alter your mind with drugs. If my parents realized these were the same as street drugs they would feel terrible and support my going off of them.
None of those chemicals in effexor occur naturally in the human brain! So much for the diabetes analogy (lie.)
Report comment
Abilify cartoon TV writers – that’s great – I know which ads you’re talking about. Complete nuts! Psychotropic drug pushing promotion has got to be one of the best and well-funded, well-lubed propaganda juggernauts in our culture. It’s absolutely insidious.
Report comment
MOST of these “adverse drug reactions” could and should be more easily avoided, by simply NOT grossly over-prescribing the DRUGS the first place! But, PhRMA, and the FedGov., and States, and Cities, and the “CMHC’s”,
and the Medical Mafia, all would rather look the other way, ignore the problem, and use that as an excuse for “business as usual”…..Sad.
Report comment
Save us all time, energy, and the potential for lifelong disability. Stop prescribing psychotropic medications.
Report comment
I don’t know if cannabis / CBD oil has been discussed in this context, so I encourage caution as it is a potent CYP2D6 inhibitor as well as inhibiting CYP3A4. There are many other genes involved in the metabolism of CBD and all drugs.
https://www.projectcbd.org/science/cannabis-pharmacology/cbd-drug-interactions-role-cytochrome-p450
Report comment