On November 15, Mad in America published a report on the marketing of two new drugs for tardive dyskinesia (TD), Ingrezza and Austedo, which cost up to $7000 per month and are being touted as “breakthrough medications.” The report provided an in-depth look at the financial influences present in their development and marketing, and told of how these expensive new medications are really “me-too” compounds, with little benefit over an existing generic used to treat TD symptoms.
Given that TD is a disorder caused by antipsychotics, there is an obvious outrageous element to this story: the pharmaceutical industry is now profiting by developing drugs to treat the harm caused by its own products.
There is another aspect to this story, one that can be dug out from the scientific literature, that needs to be known. TD is regularly presented as a disorder of involuntary movements, and thus a dysfunction of the basal ganglia. But this common conception of TD obscures a more devastating truth: TD should be understood as drug-induced brain damage that leads to a global decline in brain function. The motor dysfunction is often accompanied by an increase in psychotic symptoms, a decline in cognitive function, and an increased risk of early death.
Moreover, while the new drugs may reduce the visible manifestations of TD—the tics, spasms, and other motor abnormalities—they do nothing to repair the brain damage caused by antipsychotics. Indeed, an examination of the “mechanism of action” of the TD drugs reveals that they can be expected to worsen brain function over time. These drugs impair the normal functioning of multiple neuronal pathways in the brain.
This is the latest chapter in a long-running story of medical harm on a grand scale, to which psychiatry—and our society—has mostly turned a blind eye for decades. History is repeating itself, and to a tragic end.
The First Wave of TD
When chlorpromazine was introduced in the 1950s, clinicians noted that it regularly caused Parkinsonian symptoms—tremors, muscle rigidity, slower movements, and so forth. Researchers soon came to understand that chlorpromazine and other new “neuroleptics” worked by blocking dopamine receptors in the brain, thereby thwarting the neuronal activity in the basal ganglia that controls motor movements.
The Parkinsonian symptoms were understood to be an acute effect of the drugs. The first case reports of what came to be known as tardive dyskinesia were published a few years later, and they told of a more lasting dysfunction in motor movement. In 1959, French psychiatrists described the symptoms:
“The tongue [is] is permanently projected forward and backward following a rapid rhythm; at times the projection is to the side, sometimes to the right, sometimes to the left . . . the lips participate in this dyskinesia in the form of stereotyped suction motions, pursing, rolling and incessant champing in synergy with rhythmic contractions of the jaw.”
This strange movement disorder appeared to be related to the Parkinsonian symptoms that appeared with the initiation of antipsychotic treatment, and yet opposite in kind. The Parkinsonian symptoms arose from a deficit in neuronal activity. The bizarre orofacial movements that characterized tardive dyskinesia appeared to be related to a hyperactivity of these same dopaminergic pathways.
Over the next decade, case reports fleshed out the scope of this dysfunction. People suffered from jerky, spasmodic motions of all types. Arms, ankles, fingers, toes, torso, neck and larynx could all be affected. Those suffering from TD could have difficulty walking, sitting or standing. At times, their speech became incomprehensible, and they had so much trouble swallowing that eating became problematic.
In 1973, National Institute of Mental Health physician George Crane wrote that TD, in its severe forms, resembled “in every respect known neurological diseases, such as Huntington’s disease, dystonia musculorum deformans, and post encephalitic brain damage.”
This was also not a rare side effect. At least nine studies in the 1960s told of how TD afflicted more than 10% of all schizophrenia patients, with one report stating that the percentage might rise to 40% of all patients who were on the drugs for longer periods of time.

A Direct Effect of the Drugs
Although the etiology of TD is still not fully understood, it is thought to be due, at least in large part, to a “dopamine supersensitivity” induced by antipsychotics. This hypothesis was first put forward in the late 1970s and early 1980s.
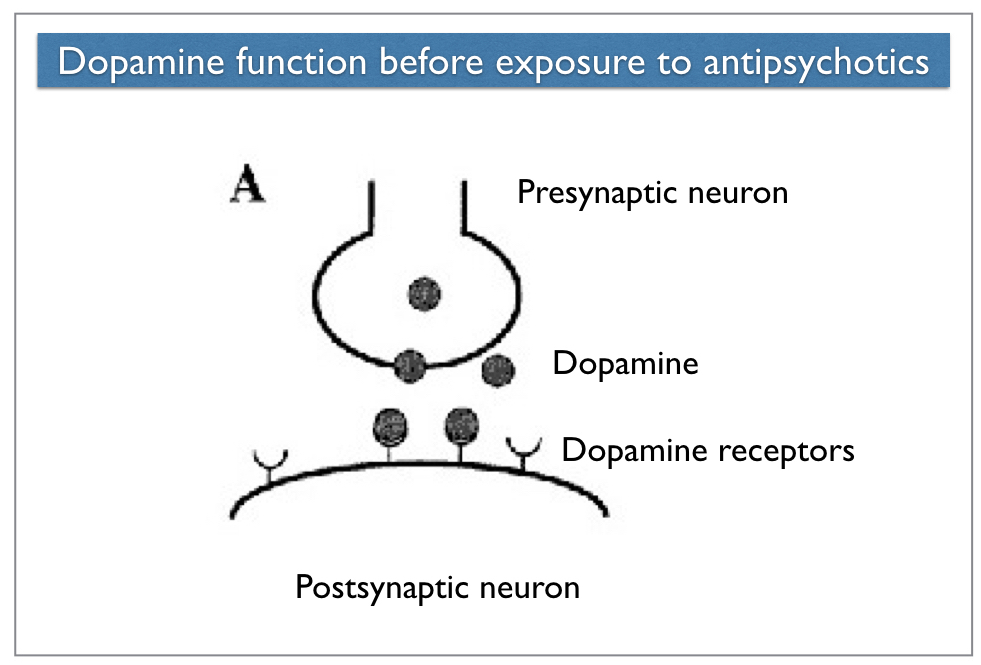
Neurons in the brain communicate in this manner: A “presynaptic” neuron releases a neurotransmitter (or chemical messenger) into the tiny gap between neurons, which is known as the synaptic cleft. The neurotransmitter then binds with receptors on the “postsynaptic” neuron. Dopamine is a neurotransmitter that excites the postsynaptic neuron and causes it to fire.
Antipsychotics “work” by blocking dopamine receptors in the brain, and in particular, a subtype known as a D2 receptor. At a therapeutic dose, antipsychotics block 70% to 90% of D2 receptors in the brain, thereby thwarting the activity of dopaminergic systems that are critical to the normal functioning of three regions of the brain: the basal ganglia, the limbic system, and the frontal lobes.
In response to this blockade, the brain tries to maintain the functioning of these pathways by increasing its own dopaminergic activity. Presynaptic neurons release more dopamine than normal; postsynaptic neurons increase the density of their receptors for this molecule. While the first compensatory mechanism—extra release of dopamine—seems to burn out after a period of time, the increase in dopamine receptors remains. The brain is now said to be in a “dopamine supersensitivity” state, with 30% to 100% more D2 receptors than normal.
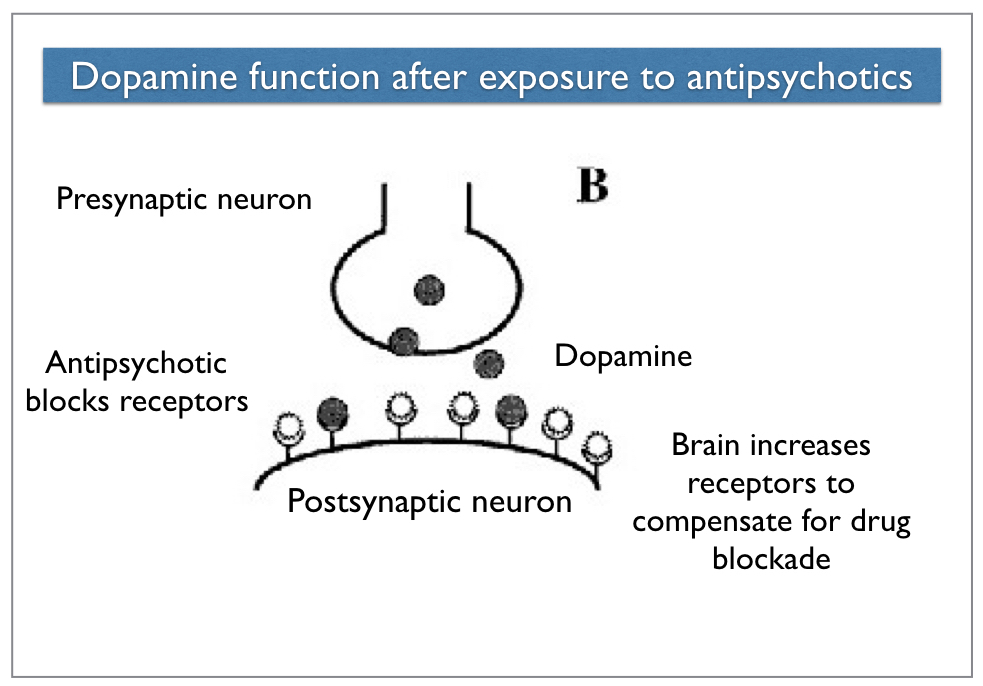
In this new state, the dopaminergic pathways may become hyperactive. The dysregulation of the dopaminergic system in the basal ganglia can lead to the constant firing of neurons that control motor movement, and hence produce the rhythmic and bizarre movements that characterize tardive dyskinesia.
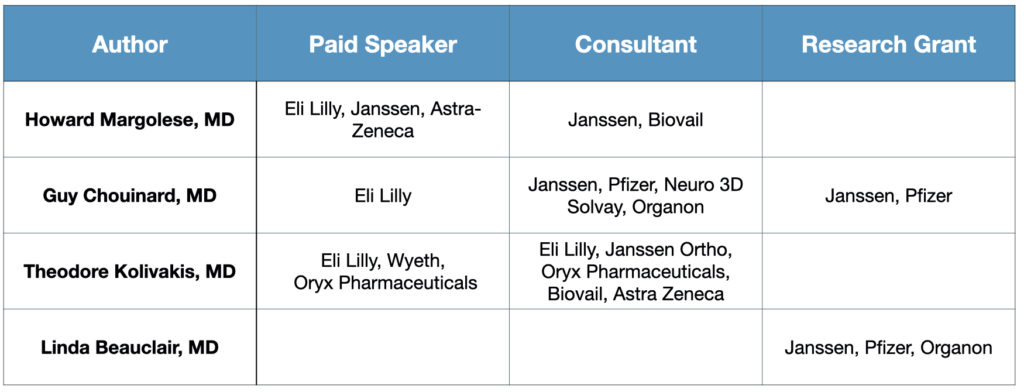
This understanding was first pieced together by two Canadian researchers, Guy Chouinard and Barry Jones, who published multiple papers on the topic in the late 1970s and early 1980s. Subsequent research, most notably by Philip Seeman and colleagues, fleshed out this picture. They determined that not only did antipsychotics stir an increase in D2 receptors, it pushed them into a high-affinity state (D2High) that increased their firing activity, and thus exacerbated this dopamine supersensitivity.
While dopamine supersensitivity is still seen as a primary cause of TD, researchers have hypothesized that antipsychotics may also damage the basal ganglia in direct ways. In rats, antipsychotics have been shown to cause a loss of cells in this brain region. Autopsy and magnetic resonance imaging studies have found lesions in the basal ganglia of some TD patients, leading researchers to compare TD to the degenerative process characteristic of Parkinson’s and Huntington’s disease. Still others have argued that antipsychotics damage neurons because they “elevate levels of oxidative stress.”
While the etiology may remain uncertain, it is evident that antipsychotics are causing neuronal damage that dysregulates their normal functioning. Moreover, TD was found to be “irreversible” in most patients, remaining after the offending antipsychotic was withdrawn, evidence that the brain damage was permanent.
Tardive Dyskinesia, Tardive Psychosis and Global Decline
Tardive dyskinesia has regularly been presented, both within the psychiatric profession and to the public, as a motor movement disorder. However, dopaminergic pathways are also essential to the normal functioning of the limbic system and the frontal lobes. The dysregulation of dopamine pathways could be expected to impair the functioning in these areas of the brain too, and, if so, cause a more global decline.
The limbic system is thought to be a mediator of psychotic symptoms, which led Chouinard and Jones to theorize that dopamine supersensitivity could lead to chronic psychotic symptoms. In a study of 216 schizophrenia patients, they put their theory to the test and determined that 30% were suffering from tardive psychosis. In more severe cases, Chouinard wrote in 1991, the “illness appears worse” than ever before. “New schizophrenic or original symptoms of greater severity will appear.”
Seeman, in his studies of drug-induced dopamine supersensitivity, concluded in 2007 that this was why antipsychotics fail over time. The drugs, which initially thwart dopaminergic activity, promote a dysregulated, hyperactive firing of neurons over the long term, with this pathology resulting, in particular, from the switch of D2 receptors into a high-affinity state.
This research reveals that antipsychotics may worsen the very symptoms they are supposed to ameliorate over the long term. Numerous other studies have found that TD is associated with a global decline in brain function. Many patients with TD show accelerated impairment in learning, memory, and a variety of other intellectual tasks. “The relationship appears to be linear,” reported Medical College of Virginia psychiatrist James Wade in 1987. “Individuals with severe forms of the disorder are most impaired cognitively.”
The list of impairments associated with TD goes on and on. In one study, 44% of TD patients weren’t even aware of their motor dysfunction, evidence that they had lost the capacity of mind to monitor their own physical well-being. As one researcher concluded, the weird tongue movements may warn of a “larval dementia.” People with TD may lose their “road map to consciousness.”
This was the understanding of TD that emerged during the era of “first-generation” antipsychotics (FGAs). It told of drugs that caused disabling brain damage, and did so with great regularity. Studies concluded that 5% of patients developed TD within one year of exposure to the drug, with an additional 5% developing it with each additional year of use. TD, researchers determined, was also associated with increased mortality.
Yet, in spite of these findings, psychiatry mostly turned a blind eye to TD, or discounted the severity of this disorder, for more than 20 years.
Turning a Blind Eye to TD
Although the first case reports of TD appeared in the late 1950s, and studies in the 1960s found that it afflicted more than 10% of all schizophrenia patients, the FDA did not step in and require the pharmaceutical companies that sold antipsychotics to warn of this risk. The American Psychiatric Association also ignored this risk during this time, with psychiatrists regularly prescribing chlorpromazine, haloperidol, and other antipsychotics in high doses.
It was this inaction that led George Crane to publish repeated reviews of the scientific literature related to TD. In his articles, the first of which was published in 1968, Crane did not argue for the withdrawal of antipsychotics from the marketplace. Instead, he wanted this risk to be known and acknowledged so that psychiatrists could learn how to mitigate this risk. Prescribing antipsychotics at lower doses and taking patients off these drugs when TD symptoms first appeared could help minimize the harm done. Crane urged the APA to mount a public education campaign, writing that “mailing informative material to all physicians is essential.”
Crane’s colleagues did not respond kindly to his efforts. He was, they suggested, making a mountain out of a molehill. Tardive dyskinesia, wrote Nathan Kline in 1968, was a “rare side effect” that is “not of great clinical significance.” Jonathan Cole, who previously had directed NIMH’s Psychopharmacology Service Center, described Crane as “a Cassandra within psychiatry” who was needlessly “foreseeing doom in many aspects of our current scientific and clinical operations.”
Yet another physician, John Curran, chastised Crane’s alarms as “not only premature but misleading,” and reasoned that even if the drugs did cause brain damage, that wasn’t reason to stop using these drugs. “While it is true that any psychosis can remit spontaneously, I honestly do not see how one can withhold a treatment of proved efficacy for fear of inflicting or aggravating putative brain damage.” Others chalked up TD to brain damage from earlier therapies, particularly lobotomy and electroshock, or attributed it to the disease.
Meanwhile, Daniel Freedman, editor of the Archives of General Psychiatry, dismissed Crane’s call for a mailing to physicians. Psychiatrists already had at their disposal “considerable data and guidelines to help determine sound judgments,” he wrote.
All of this frustrated Crane to no end. “The majority of clinicians continue to ignore the existence of this complication,” he wrote in 1973. “The neglect of a serious health problem for so many years has deeper roots than mere ignorance of facts.”
That year, the FDA did begin requiring the pharmaceutical companies to warn about TD in their labels. But the APA continued to dawdle, and as Crane had written, there were “deeper roots” for its lack of action.
American psychiatry was in the process of turning away from talk therapy and embracing drugs as first-line therapies. The arrival of chlorpromazine, it was said, had made it possible to empty the asylums, and had kicked off a “psychopharmacological” revolution. The new drugs for schizophrenia, while initially called “neuroleptics,” were now understood to be “antipsychotics,” a name that told of how they were specific antidotes to psychosis. This was a narrative that enabled psychiatry to see itself in a new light, as physicians in white coats, and there was a financial incentive at work too: a psychiatrist could earn more by prescribing drugs than by talking to patients.
TD threatened all this. If the field came to understand that antipsychotics caused brain damage in a significant percentage of patients, that entire narrative would burst.
And so the APA dawdled. In the early 1980s, more than 20 states—responding to the APA’s lack of action—passed laws requiring physicians to tell their patients about this risk. Yet, even this legal mandate failed to have any marked effect on prescribing practices. A national survey found that disclosure rates about the risk of TD were lowest in states where it was mandatory.
Indeed, America’s psychiatrists were busily ramping up this risk with their prescribing habits. From 1973 to 1985, the average daily doses of prescriptions of antipsychotics doubled, with psychiatrists prescribing the drugs at dosages that were four times higher than those prescribed by non-psychiatrists.
In 1984, Thomas Gualtieri, a physician at the University of North Carolina, summed up this dismal record: “A review of the history of TD demonstrates nothing as clearly as this fact: since 1957, published guidelines, scientific articles, presentations at professional meetings and draconian admonitions in the Physicians Desk Reference seem to have had little, if any, effect on actual physician behavior with respect to neuroleptic drugs.”
Finally, in 1985, after several highly publicized lawsuits found psychiatrists negligent for failing to warn patients of this risk, the APA sent out a letter to its members. Financial concerns were noted in the missive. “We are further concerned about the apparent increase in litigation over tardive dyskinesia,” the APA wrote.
The history told here—of a profession that turned a blind eye to TD for decades—is well known, even within the field. In a 2006 editorial on TD published in the American Journal of Psychiatry, John Kane revisited it one more time:
“The history of tardive dyskinesia holds many instructive lessons regarding long-term adverse drug effects. First described in the late 1950s shortly after the introduction of antipsychotics, it took many years before its prevalence, incidence, and long-term course were well investigated. At first there was resistance and skepticism from many quarters as to the risk of this condition and its apparent association with long-term exposure to antipsychotic medication . . . Some might argue that it was until the threat of litigation became more and more a reality that clinical practice included adequate consideration of and monitoring for tardive dyskinesia.”
TD in the Atypicals Era
After the APA sent out its warning letter in 1985, the field’s recommended “best practices” did change. Antipsychotics should be prescribed at the lowest possible dose, physicians were told, and with certain groups of psychotic patients, such as those who had suffered a brief psychotic episode, they should try to limit their long-term use.
The risk of TD was finally being acknowledged. This was a serious, irreversible disorder and prescribers needed to keep it in mind when treating psychotic patients. And the risks of these drugs were such that they shouldn’t be used “off-label” for less severe conditions.
But then risperidone and olanzapine were brought to market in the mid-1990s, and a new story emerged. The field now had safer drugs that didn’t carry this same risk.
When risperidone was approved for sale, Janssen told of how its new drug didn’t appear to cause Parkinsonian symptoms. The risk was said to be the same as “placebo.” And if this was so, it seemed likely that that the longer-term risk of TD might dissipate too. Soon published reports from one-year extension trials, funded by Janssen, told of how the one-year year incidence of TD with this new drug was 0.3% or even less.
Eli Lilly told much the same story about Zyprexa (olanzapine). The risk of Parkinsonian symptoms with this new drug was much less than with the FGAs. The company also reported that in an extension trial in schizophrenia patients, the one-year incidence of newly emergent TD was 0.52%, compared to 7.45% in the haloperidol patients. “Our results indicated a significantly lower risk of tardive dyskinesia with olanzapine than with haloperidol.”
This became the common wisdom, and subsequent reviews of the industry-funded extension trials further cemented this understanding. A 2005 review of seven one-year trials of risperidone reported there were only two cases of TD among 1,156 patients treated with the drug (0.2%). The incidence rate was 0.4% for those treated for longer than one year. The same review reported that while the data from three extension trials of olanzapine weren’t quite as good, the incidence of TD (2.6%) was still markedly lower than in those treated with haloperidol (8%).
Yet another review reported that the annual incidence of TD in children treated with second-generation antipsychotics (SGAs) was 0%.
Worries about TD faded away. Newly trained psychiatrists, fresh out of medical school, could have concluded that this was a harmful side effect from the distant past. “It is not surprising that tardive dyskinesia has been somewhat less of a focus among clinicians and investigators,” Kane wrote in his 2006 editorial. “The current preponderance of prescriptions of second-generation antipsychotics means that a new generation of clinicians has been trained without the extensive exposure to TD that older clinicians and patients experienced.”
A 2007 review in Current Drug Therapy summed up the good news. The annual incidence of TD with the first-generation antipsychotics had been 5%; it was 0.5 to 1% with the second-generation antipsychotics. TD with the new drugs developed “five to ten times less often” than before, the authors wrote.
Upon Further Review
Those were the published results that enabled the manufacturers of the “atypicals” to promote their use for off-label purposes: as adjuncts to antidepressants and bipolar medications, for anxiety and sleeping disorders, and for pediatric uses. Although these drugs were known to cause adverse metabolic effects, the specter of tardive dyskinesia had more or less disappeared.
However, that benign picture of the second-generation antipsychotics (SGAs) had emerged from short-term RCTs and open-label extension trials that had been funded by the makers of these drugs. The authors of those reports regularly had financial ties to the pharmaceutical companies; the 2005 review was authored primarily by members of the speakers bureaus for Janssen and Eli Lilly.
A different result emerged from studies of the new drugs that were publicly funded, or when researchers looked more critically at the industry-funded research, identifying the ways those trials had been designed to make the new drugs look better than the old.
In 2003, Stefan Leucht and colleagues reported that there was no significant difference in TD when the second-generation drugs were compared to low-potency drugs from the first generation at similar dosages. Next, in 2005, results from the NIMH-funded CATIE study were published. This study compared four SGAs to a first-generation drug, perphenazine, and researchers found there was no significant difference in their effectiveness or tolerability.
Moreover, the NIMH reported, “movement side effects (rigidity, stiff movements, tremor, and muscle restlessness) primarily associated with the older medications were not seen more frequently with perphenazine than with the newer drugs.” There also was no difference in the emergence of TD in those treated with the older drug.
A government-funded RCT in the UK, known as the CUtLASS study, produced similar results. There was no difference in outcomes for those treated with FGAs compared to those treated with SGAs (if anything, quality of life was better for the FGA group). The incidence of newly emergent TD was the same in both groups as well.
Next, in 2010, Scott Woods from Yale Medical School reported on the emergence of TD in 352 patients treated at a conventional health center from 2000 to 2003. At baseline, this group of patients did not show signs of TD, and then, during the study, the disorder developed in 6.6% of patients each year (the incidence rate.) Researchers had studied a similar group of patients at the same community center in the 1980s, and the yearly incidence of TD in that study was 5.3%, or slightly less than in this new “atypicals” era. The severity of the newly emergent cases in the two eras was the same too.
Moreover, the prevalence of TD in all patients treated at the community center during the 1980s and during the 2000s was the same: 33%. TD was very much the same problem it had been before the arrival of the SGAs.
“Despite the feeling among some clinicians that TD is much less of a problem now in the atypical era, such a conclusion may unfortunately be premature,” Woods and his collaborators wrote. “In the 1960s and 1970s, there was some well-intentioned resistance and skepticism about conventional antipsychotics being associated with risk of TD, and now, during the atypical era, we are perhaps not immune to some of the same forces. Until we are certain that we have developed antipsychotics that carry minimal risk, we should continue to inform patients prescribed antipsychotics about TD and continue monitoring for it.”
Meanwhile, researchers were also now looking at TD in children and adolescents, and the results were chilling. Investigators at the University of Maryland reported that 10% of 116 pediatric patients they studied developed TD after they had been on SGAs for one to two years. Spanish investigators found that 38% of children and adolescents on antipsychotics for longer than one year showed signs of mild TD.
There is still an ongoing debate regarding the comparative risk of TD with the FGAs and the SGAs. Various authors have concluded that the one-year incidence rate with the SGAs is 3% or a little lower, or about two-thirds the incidence rate with the FGAs. However, the FGAs are still being prescribed to a small percentage of patients diagnosed with schizophrenia, which could lead to a higher overall prevalence rate. Polypharmacy, which is a common practice, increases the risk of TD as well. As a result, the prevalence of TD among long-term users of antipsychotics today may be only slightly diminished from earlier decades.
There is one other factor at work now with TD: the expanded prescribing of antipsychotics exposes a much larger number of people to this risk.
“Given the increased use of SGAs in today’s clinical practice, including frequent off-label use for non-psychotic conditions (major depressive disorder, personality disorder, autism spectrum disorder, sleep disorder, etc.) the occurrence of TD and its burden may continue to rise,” the authors of a 2014 report concluded.
The “New” TD Drugs
At the start of the atypicals era (1997), .8% of the U.S. population was prescribed an antipsychotic in an outpatient setting. A decade later, this percentage had risen to 1.3%. Today, according to a survey of outpatient antipsychotic usage from 2013 to 2018, 1.6% of all adults are using the drugs. That’s 3.8 million adults.
This number doesn’t include usage of antipsychotics in institutional settings (psychiatric hospitals, nursing homes, and so forth). It also doesn’t include the prescribing of antipsychotics on an outpatient basis to children and adolescents. Such prescribing virtually never happened prior to the arrival of risperidone on the market, but has become almost commonplace since then, with prescriptions for an antipsychotic written at one in every 62 outpatient visits by children and adolescents, ages 4 to 18, in 2010.
This would put the total number of people exposed to antipsychotics each year to well north of four million, and even if the yearly incidence of TD is 3% (compared to higher findings of 5% in some studies), this would lead to more than 100,000 new cases of TD each year.
For its part, Neurocrine Biosciences, the maker of the TD drug Ingrezza, estimates that there are 500,000 people in the United States with TD, and that only 20% of this population has been so diagnosed. With Neurocrine and Teva Pharmaceuticals selling their drugs for TD at a yearly cost of $80,000 per patient, this would, in theory, create a $40 billion annual market for these medications.
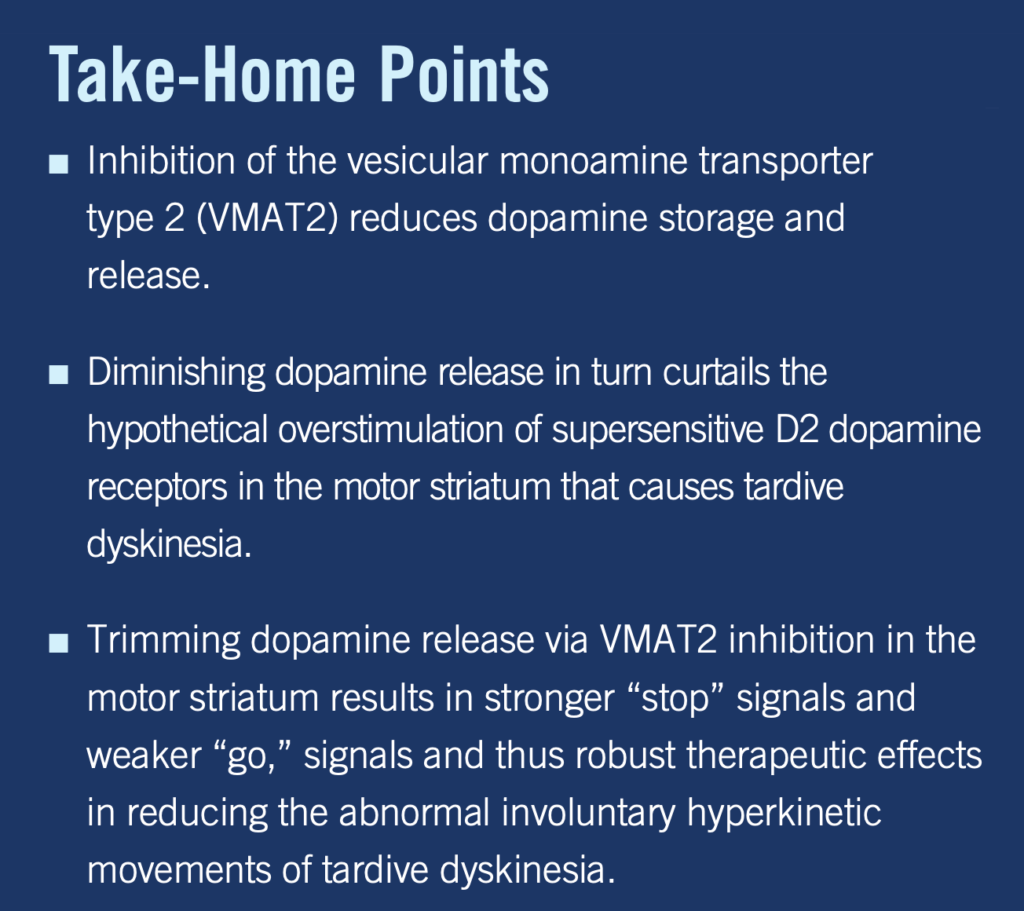
The new drugs—valbenazine (Ingrezza) and deutetrabenazine (Austedo)—are both VMAT-2 inhibitors, as is a generic that has been on the market since 2008, tetrabenazine. These drugs inhibit the release of monoamines—doapamine, norephinephrine, serotonin, and histamine—from presynaptic neurons, and thus diminish neuronal activity along those neurotransmitter pathways.
Their inhibition of dopamine release means that VMAT-2 inhibitors have an effect similar to antipsychotics on motor movement. VMAT-2 inhibitors reduce dopamine levels in the synaptic cleft; antipsychotics block D2 receptors on the postsynaptic neurons. They are different mechanisms but with a common end: they both put a brake on dopaminergic activity in the brain and thus still motor movements.
A 2018 paper in CNS Spectrums summarized their effects in this way:
As can be seen in this description, valbenazine and deutetrabenazine do not provide any remedy for the pathology—antipsychotic-induced dopamine supersensitivity—thought to be a primary cause of TD. Rather, these drugs interrupt neuronal activity essential to normal brain function, the release of dopamine and other common neurotransmitters into the synaptic cleft.
The makers of these new TD medications urge patients to continue taking their antipsychotic medication. This mix of antipsychotics and VMAT-2 inhibitor leads to a double dose of agents blocking normal dopamine activity in the brain, which act in opposition to dopaminergic neurons that are primed to fire in a dysregulated, hyperactive manner. It’s a bewildering mix of stop and go signals.
This isn’t the end of the disruption in brain function that occurs on this antipsychotic-VMAT drug mix. VMAT-2 inhibitors also diminish the release of serotonin, norephinephrine, and histamine. SGAs also block serotonergic, histaminergic, muscarinic, and adrenergic receptors. Multiple neurotransmitter pathways are now being perturbed in ways that impair their normal functioning.
In clinical trials, the safety and efficacy records of the two TD drugs were much the same. The list of common side effects for both drugs includes fatigue, sedation, somnolence, insomnia, depression, restlessness (akathisia), agitation, and nausea. Less common, yet potentially more serious risks with VMAT-2 inhibitors include severe depression, suicidality, symptomatic hypotension, prolongation of the QTc interval (a risk for cardiac arrest), and neuroleptic malignant syndrome.
The Abnormal Involuntary Movement Scale (AIMs) was used to assess efficacy in the trials. This is a 28-point scale based on physician ratings of the severity of abnormal movements (0 to 4 for seven items).
In a 12-week randomized trial of deutetrabenazine, symptoms in the medicated group dropped 3 points, versus 1.6 points for the placebo patients. While this 1.4-point difference was statistically significant, it didn’t translate into clinically noticeable differences as measured by the Clinical Global Impression of Change and Patient Global Impression of Change instruments.
In a six-week trial of valbenazine (KINECT-3), symptoms in the treated group dropped 2.9 points, while the placebo group worsened slightly.
The valbenazine patients were then entered into a 46-week extension study. Their symptoms improved slightly during the first 42 weeks, and then, once valbenazine was withdrawn, their symptoms quickly worsened. Their AIMS scores climbed back toward baseline figures, evidence that the treatment had not done anything to ameliorate the underlying TD pathology. The drugs—by reducing dopaminergic activity and thus quieting movement—had simply reduced the visible symptoms of the disorder.
The period of worsening following withdrawal of valbenazine, the researchers concluded, was evidence of “the need for continuation treatment.”
The Harm Rolls On
In their promotional materials, Neurocrine Biosciences and Teva Pharmaceuticals tell a story of medical progress. Antipsychotics are presented as essential medications that help people diagnosed with schizophrenia or some other serious disorder live normal lives, surrounded by family and flourishing in the workplace. TD is presented as an adverse side effect of antipsychotics and other psychotropic drugs that leads to tics, spasms, and other abnormal movements—there is no mention of other impairments. Thanks to the new TD drugs, there is now an effective remedy for the motor impairments, the ads featuring “patients” who smile brightly and move about their worlds with a physical ease.
The articles on TD published in medical journals, while sober and academic in tone, ultimately tell a similar story of medical progress and benefit from psychiatric drugs. There is little or no mention of antipsychotic-induced “brain damage.” Most of the articles focus on the abnormal motor movements as the primary impairment associated with TD; there is little mention of how TD is associated with a worsening of psychotic symptoms and global impairments. Their articles tell of how valbenazine and deutetrabenazine have been found to be “safe and effective.” Few readers of this literature would know that VMAT-2 drugs work by blocking the normal release of dopamine and other essential neurotransmitters into the synaptic cleft.
Together, the promotion of these drugs to the public and the articles in the medical journals protect current prescribing practices. The prescribing of antipsychotics for off-label purposes can continue. So too the prescribing of antipsychotics to children and adolescents. The risk of developing TD is described as low; most cases of TD with the SGAs are described as mild; there are now drugs that can quiet TD symptoms.
A recently published study tells of how the TD epidemic can be expected to roll on. The number of American youth treated with psychotropic polypharmacy nearly tripled from 1999 to 2015, with 293,492 put on such a regimen during the years 2011 to 2015. The percentage prescribed an antipsychotic as part of their drug cocktail rose from 38% to 75%. There were even a significant number of children 0 to 4 years old put on such cocktails.
Here are the type of questions that go unasked in the medical literature: How many of these children and adolescents will develop TD? How many will develop severe cases? How will their lives be impaired as a result?
Today, psychiatry looks back at its earlier response to TD as mistaken, as a past that should serve as a lesson for the future. But starting with the arrival of the SGAs, history began to repeat itself and the TD toll has rolled on and on.
****
MIA Reports are supported, in part, by a grant from the Open Society Foundations






“Today, psychiatry looks back at its earlier response to TD as mistaken, as a past that should serve as a lesson for the future. But starting with the arrival of the SGAs, history began to repeat itself and the TD toll has rolled on and on.”
Does psychiatry look back or forwards? Never. If they do, it is with apathy. Few shrinks practice medicine and few shrink have ethics. It was only ever the public that saw their trail of harm, but what they then did was go underground, by becoming number one drug dealer. It was easy, make people swallow stuff and their misery, reactions, homelessness can be seen as parts of their “illness”, or as “side effects”.
There is absolutely no doubt that psychiatry will continue to unleash more and worse harms. It is simply part of their nature. There is something deeply broken within not just the system of psychiatry, but within the practioners.
No one EVER wants to point to individuals. Pretending that the APA is something inanimate, that causes these malpractices. As if a block of wood is spreading the BS, and the block of wood does the prescribing.
Sure, sometimes we pick on Dr Lies, but what for? As long as we pretend that it is JUST SOME shrinks, we are kidding ourselves.
Like really? Just some? It seems weird that “just some” could do so much harm. That just some could use up so many script pads, and insurance money.
Yes your neighbourhood shrink is the azz that will get people on these “ANTI-TD” drugs. Why? Because he gave them “TD” drugs.
But really, we should not ever use the word “anti-psychiatry”. The word “anti” is reserved for “anti-depressants”, “anti-psychotics”, “ANTI-TD” drugs, and they are all given for this “ANTI-MENTAL ILLNESS” crowd.
Thanks Robert, I do hope a few people besides survivors read the article and I hope a few people will be spurred to tell shrinks to fuck off.
Unless you are the only one that has the guts to try and warn the public. Something tells me that even therapists run chicken.
It’s not an admirable trait to run chicken.
Report comment
Withdrawal can make TD appear worse. All neuroleptic studies take people addicted to the drugs and withdrawal half claiming that is a placebo group. This is one way the psychiatric studies hide how prevalent TD is with these drugs. They compare people who’ve been given brain damage from the drugs and are going through withdrawal to just people taking the drugs.
The same thing happens with the new TD drugs. Since many people who enter a TD trial have either been on an old TD drug or reduced their neuroleptic dosage they are going through withdrawal. Adding the new TD drug means the drug group is no longer in withdrawal.
You can see this in the TD drug studies where the entire drug benefit over “placebo” occurs in the first 4 weeks. After that period the placebo group has a larger improvement over the drug group but enough time doesn’t pass to overcome the outcomes in the first 4 weeks.
Adverse even data from the corporations show the TD drugs over 12 weeks cause 5.2% of the people taking the drug to develop Akathsia (another painful movement disorder caused by brain damage) verse 0 for the “placebo”.
Taking a new deadly addicting brain damage causing drug to sedate and temporary cover the symptoms of brain damage from the first drug is making the same mistake over and over again.
Some studies have found that taking vitamins B6, magnesium, Iron, Omega 3 and B12 can have some benefits for TD and other movement disorders. Though make sure if you take these not to take huge amounts as very high dosages of vitamins can cause harm.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440239/
Report comment
Abram Hoffer used vitamin B3 and mineral manganese to prevent and treat TD. He claimed that if a little manganese were put in with the drugs, TD wouldn’t occur. Of course, never taking major tranquilizers, going to as low a dose as possible, or stopping are better than the roundabout way of preventing or treating. Here’s a Kunin article, and an orthomolecular journal search engine:
http://orthomolecular.org/library/jom/1976/pdf/1976-v05n01-p004.pdf
http://orthomolecular.org/library/jom/
Report comment
Well, we can’t have something as cheap and accessible as manganese and Vitamin B3 as a treatment! Where’s the money in that? Sheesh!
Report comment
One reason I sometimes think of myself as a secret agent instead of a psychiatric consumer. And my mission is to disrupt psychiatry by providing cheap alternatives to allegedly therapeutic drugs (shh).
Report comment
Yeah, better keep THAT one quiet! They’ll be coming after you for elbowing into their “turf!”
Report comment
Yes, he got the idea from Richard Kunin.
Report comment
Cool. I saw in a book yesterday that B6 has been used like you said, and I’m sure the other ones. Although Dr. Thomas Levy says iron should almost never be supplemented unless a proven low blood count…and same for copper and calcium.
I do wish insurance covered nutrients. My quality fish oil is $75 for 120 high dose capsules. My insurance gives me $240 a year for ‘over the counter’ products, including a number of nutrients, but they are lower quality and with few brands. Not ideal, but I guess it’s a start. I don’t think any other insurance policies I’ve had attempted to do that.
Report comment
Number 1: There is no money in covering nutritional supplements. Number 2:Very Rarely does the FDA “approve” of nutritional supplements like they do “drugs.
And so, back to Number 1. Oh, did I forget, that if you see an advertisement for nutritional supplements, they will be a disclaimer that this supplement should not be used to treat any medical condition without a doctor’s approval. But, then, if you see the advertisements from “legal groups” who claim they will help you get compensated from some harm, you may have received a “drug” there is a tagline that you shouldn’t stop the “drug” without consulting a healthcare professional. Oh, and did, I say, if you read any book that gives you advice or suggestions about supplement or non-traditional medicine, etc. there is also a “medical disclaimer.” I don’t even see that when I read books on law that I must consult a doctor or about religion, I must consult a theologian or my local pastor. And there is a lot of other examples any one of us could name. Thank you.
Report comment
I personally am aware of these very relevant and unfortunate points. Thanks for pointing them out. None of these areas will change anytime soon. In a sense, it is two separate worlds living simultaneously.
I still would like the same kind of financial assistance I get from insurance to be used for nutrients supplements. Out of pocket supplement expenses can get quite pricy if you are hardcore. If it was either seen or ‘proved’ (and FDA ‘approved’) that nutrient supplements could prevent the need for more expensive treatments or illnesses, the doctors and insurers may have a change of heart. But this gets to the crux of the matter. Apparently there has been a recent clinical phased trial of diet/supplements/electric current stimulation for multiple sclerosis. I don’t know if such results could be ‘FDA approved’ and ‘prescribed/covered’.
My insurance gives some money to supplement, to gyms, and I think to dietary aspects in some way. But it’s a roundabout way, and the supplements are a drop in the bucket relatively speaking.
Most psychiatrists don’t care or warn against them. But there are a few….if only one of my first dozen prescribers had helped me in this regard.
Report comment
I also find your points to partially apply to old generics too. My affordable generic ketamine cannot be patented unless big pharma makes a subtle tweak or two and patents that, like they did with the nasal spray. In this case, the generic ketamine is fda approved but is used ‘off-label’. I cut down my tranquilizer by 75-85% simply by using ketamine. This tranquilizer is $1500 retail no matter what dose or how many times a day.
Report comment
It needs to be legally mandated that when these drugs are prescribed, that patients are informed that they work by damaging the brain and inhibiting normal brain functions. ESPECIALLY in regards to child psychiatry/drugging. AND that this damage is permanent, in myriad complexities; you will never be the same.
Just as this class of drugs was once called, a “chemical lobotomy”
Report comment
I wholeheartedly agree with your comment. When prescribed antipsychotic medications, drugs that change brain function resulting in brain damage, the prescribing doctor should be legally obligated to spend a substantial amount of time educating the patient and providing thorough, factual, and objective information regarding the medication. This should include all the short and long term effects on the brain and body; temporary and permanent. In addition, the doctor should be legally obligated to educate- in depth – about the types of tardive dyskinesia (both common and uncommon) that will ultimately occur and be honest about the ramifications of TD including how it can absolutely shatter the lives of patients and families. It is only with this raw knowledge that a person can make an educated decision- weighing out the risks and benefits. Yes, even if the doctor doesn’t agree with the decision. And if the doctor doesn’t possess this information or have the ability and time to thoroughly educate their patient, they shouldn’t be allowed to prescribe this type of drug. At the end of the day, it is the patient that is going to be profoundly affected by this decision regarding medication; not the prescriber. Therefore, in my opinion, the prescriber should be legally responsible to tell the patient the truth about how these drugs affect brain function.
Report comment
I want to point out, that while I completely agree with you, I know many people will read this sort of thing and scoff, thinking this is all just a metaphor for banning drugs. Really though, I think this is how it should be with ALL drugs. Including currently illegal ones, such as cocaine, etc. and like you said, whether the doctor agrees with the decision or not. They should not be authorities; they should be collaborators.
Report comment
Absolutely
Report comment
Would it be cool if they manufactured arsenic-laced throat lozenges, as long as they acknowledged on the label that they’re likely to be lethal?
Report comment
How about the difference in health between patients prior to 65 years ago and patients today? For one thing, there had to be a great deal less chemically induced brain damage back then, and heart damage, etc. Of course, perhaps they made up for a little of it with lobotomies, radical brain surgery.
I hope people begin to get the idea that if they are going to be treating people for “mental ill health conditions”, they shouldn’t be treating them to brain damage, or other and further impediments to good overall physical health. Degenerative ailments are, duh, not likely to improve “mental health” one iota.
Report comment
I’m not sure if i’m completely accurate on this, but I recall reading something in the past that life expectancy was based on data involving senior citizens, and thinking to myself; what about all the people who died BEFORE getting old? Are they in the equation?
Report comment
“This was a serious, irreversible disorder and prescribers needed to keep it in mind when treating psychotic patients. And the risks of these drugs were such that they shouldn’t be used ‘off-label’ for less severe conditions.”
This is opposite of what psychiatry has done, since the antipsychotics/neuroleptics are now recommended for both the “bipolar” stigmatized, as well as those labeled as “depressed.” Why does the psychiatric establishment seemingly always recommend the opposite of what is good for their clients?
“history began to repeat itself and the TD toll has rolled on and on.” Yes, the Nazi psychiatrists were behind the Nazi holocaust, and today the psychiatrists are murdering “8 million” people EVERY year, with their “invalid” DSM disorders and their neurotoxic psychiatric drugs.
https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2013/transforming-diagnosis.shtml
https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2015/mortality-and-mental-disorders.shtml
When will our modern day, staggering in scope, psychiatric holocaust end? Thank you, Robert, for explaining the problems with psychiatry’s newest “wonder drugs.” (Pardon my sarcasm.)
Report comment
I am surprised this comment was allowed by the censors. I will attempt to back it up with online articles
Nazis increased the likelihood of death and decreased the likelihood to have children in their enemies.
Death: increased chance of
“By Marilyn Elias, USA TODAY
Adults with serious mental illness treated in public systems die about 25 years earlier than Americans overall, a gap that’s widened since the early ’90s when major mental disorders cut life spans by 10 to 15 years, according to a report due Monday. ”
https://usatoday30.usatoday.com/news/health/2007-05-03-mental-illness_N.htm
Reproduction: having children
Sexual side effects of pharmacological treatment of psychiatric diseases
“there is consistent evidence to suggest that a large number of psychiatric medications adversely affect one or more of the three phases of normal sexual response: desire, arousal, and orgasm. ”
https://pubmed.ncbi.nlm.nih.gov/20668442/
Report comment
I’ve made the comparison many times, and used to get in trouble for it. It’s a valid comparison. If we can’t learn from what happened then; how ordinary people could commit such atrocities, then we’re perhaps destined to be doomed.
Report comment
Except it’s not a “comparison”; psychiatry was literally responsible for developing the methodology and setting up the infrastructure for “euthanizing” psychiatric inmates, which was later used on the Jews. And after the Nazi defeat psychiatrists were discovered still “euthanizing” psychiatric inmates.
Report comment
Why do psychiatrists repeatedly use drugs that are bad for patients? Because the salesman who visits the psych’s office tells them it’s OK, that’s why. If the shrink is one of those guys who got into psychiatry because the pharmacology classes were too tough, he’ll willingly agree to whatever the company rep (who never even studied pharmacology) tells him.
Report comment
I support someone at home with severe cognitive impairment and I am terrified of disclosing to medical professionals what we family members observe on a daily basis out of a fear that our loved one will not be correctly diagnosed with an iatrogenic illness and be drugged even more, or worse, be involuntarily committed or institutionalized. We remain isolated without any services to help our loved one recover from the trauma of years of psychiatric abuse. I fear that my loved one is losing her awareness of her impaired cognitive functions and we are stuck between a rock and a hard place with no help in sight. At this point hope for her recovery looks bleak and my focus is how she will receive support with the activities of daily living if I die or become disabled. I dont think that she will ever receive an honest medical assessment, education from a licensed physician to make her aware of her condition, and support titrating off harmful medications. I believe she will be blamed for the ineffectiveness of her ‘treatment’ (they will call it treatment resistance’ every time she experiences a drug induced crisis that not be concealed from an indifferent society) . Although I dont think she will be a beneficiary of any shift in public consciousness or change in clinical practices–because it is likely to be too little too late—I will continue to work for change with what little strength I have.
Report comment
I understand. Take care.
Report comment
And now look at this; https://youtu.be/5EX-IY9W2-4
And this
https://www.facebook.com/groups/427287381619905/permalink/429231301425513/
Someone needs to get a federal prosecutor on the phone. Really. There is a case and beyond and millions of victims in its wake and affecting society as a whole.
Report comment
Thanks for the article. As always, very well written.
Report comment
“This is the latest chapter in a long-running story of medical harm on a grand scale, to which psychiatry—and our society—”
I feel that should read “And our government”. Really, society can’t turn a blind eye to something that is not being presented to them. Our “government”, as an “entity”, knows full well what is going on and chooses to not make this an issue.
Report comment
In a comment on a previous article on the subject, I mentioned seeing an article about manganese 30 or so years ago. I was wrong- the piece was in a 1976 Journal of Orthomolecular Psychiatry (or Medicine as it had a name change). If you want to see it, it’s on archive at the Orthomolecular.org site, which allows you to see back issues. You can look up tardive dyskinesia as a subject, Richard Kunin’s works as an author.
Report comment
Here is a Kunin article and an orthomolecular journal search engine. Abram Hoffer also wrote and used manganese and vitamin B3. He thought if low dose manganese was added to the drugs, TD wouldn’t occur. Never starting major tranquilizers, going to as low dose as possible, or stopping completely, is of course preferable.
http://orthomolecular.org/library/jom/1976/pdf/1976-v05n01-p004.pdf
http://orthomolecular.org/library/jom/
Report comment
You’ve got to remember that Hoffer’s case load was filled with other people’s treatment failures who were referred to him for that very reason. They were the folks likely to wind up on antipsychotics for some time, unless he could pull them free of them.
Report comment
Interesting point I don’t always consider.
I have mixed feelings when Hoffer said that many of these referred people already had a schizophrenia diagnosis, and he usually agreed with the diagnosis.
I live by most of his principles everyday. However, he did not know about the personal and collective unconscious (mythopoetic imagination). It is ironic that he differentiated between ‘psychotomimetic’ and ‘psychedelic’, used psychedelic therapy before they were made illegal, was colleagues with Humphrey Osmond who created the word and who had a great many psychedelic experiences, but yet they both, it (usually) seems to me, saw hallucinated voices and visions only as ‘symptoms’. I guess often constellated with other symptoms. All very complex, but sometimes I wish Hoffer and Osmond were more nuanced in this area, even if ‘treatment’ is necessary. I will still devote part of my website to Hoffer’s field of orthomolecular psychiatry and medicine.
Report comment
Hoffer and Osmond had interesting backgrounds. Hoffer wasn’t a psychiatrist at all. When the province of Saskatchewan offered him his first psych job as Director of Psychiatric research for the province, they sent him to various psychiatric schools and facilities to give him a grasp of 1950’s psychiatry. Late in his career he developed vitamin programs for cancer patients.
Osmond spent World War II as a ship’s surgeon on convoy escorts, after (foolishly?) asking the Admiralty for a shrink’s job on board one of the larger naval units. When he went to Canada, he became superintendent of Weyburn Hospital (at the time, one of the world’s worst mental institutions), doing novel things like converting the hospital’s seclusion rooms into refuges for those with sensory overloads (I know some of the contributors might be shocked to hear that there were patients who had to be talked out of hanging out in them instead of fighting not to be put into them).
Both of them had used hallucinogens of various kinds (Osmond took peyote while participating in a native ceremony). Both were involved in psychedelic therapy for alcoholism, which became routine in the province until the US DEA put pressure on the province’s government to cease and desist from giving patients LSD.
Report comment
bcharris
Sometimes I forget, or am less clear than I’d like, that Hoffer learned most psychiatry on the job so to speak. He did have a medical degree and a degree in biochemistry first. I have seen that one of Hoffer’s first cancer patients he treated was 1977, around the time when Linus Pauling was starting to research it. Hoffer developed it more over time. I see that he had treated 1000 clients with cancer by 1998, with much study in the late 80’s.
I didn’t think Hoffer had tried other psychedelics other than ‘adrenochrome’, which he said would never become a ‘darling’ street drug. The movie psychedelic pioneers is remarkable, showing Osmond and Hoffer’s history, but doesn’t mention nutrients except for maybe briefly once. https://www.cultureunplugged.com/documentary/watch-online/play/50658/The-Psychedelic-Pioneers
Hoffer’s memoirs are like $180 on Amazon. Even Osmond was somewhat tight lipped about his and Hoffer’s nutrient research later in his career. Osmond wrote about hospital design and models later in his career more than nutrients, which were Hoffer’s special focus. I get the impression Osmond didn’t practice full orthomolecular therapy at the hospital in Alabama, very near me. Aldous Huxley and osmond’s letters are fascinating. Osmond elaborates extensively on his mescaline, lsd, and peyote experiences, which were a lot. I believe his diagnostic methods for schizophrenia were, at times, unfair, always considering schizophrenia as psychotic rather than psychedelic, despite his research on how mescaline led to hypotheses of the schizotoxin he sought for. His book Models of Madness is flawed but very useful. The fact that he uses the word ‘madness’ throughout, and as basically a synonym for schizophrenia, is unfortunate. He barely even attempts to define ‘madness’ and says it basically has always been understood as a concept throughout history.
Report comment
Hoffer also had had LSD. I believe I found out from a piece in The Hallucinogens, a very rare out-of-print volume he and Osmond wrote in 1967 (that devoted 120 pages to LSD).
The book is hard to find. If the other owners are like me, they’re more likely to shoot you rather than lend their copies out.
Report comment
bcharris,
I just ordered Hoffer’s & Osmond’s The Hallucinogens from inter-library loan!
Report comment
This is an excellent article. One thing that stood out to me is “chemically induced brain damage.” And there is something that Willoweed said about “drugs to cover up the effects of other drugs.” From my experience with the “psychiatric industry”, that seems to be one of their justifications for “poly-pharmacy.” However, this is a “hidden justification” in a way. They would start with one or two drugs, then, they would say, “here try this drug because of the effects of these other drugs.” I remember having to be taken off “abilify” because it closed my throat to the point I could not swallow. Of course, then they put me back on risperidal, which, they had taken me off earlier for the “abilify” because “abilify” was such a wonder drug!
But, it is the “chemically induced brain damage” that is the most haunting. Even after years off these drugs, it will haunt you. It is also unseen, in many cases, as opposed to a war veteran who might have tragically lost their legs or worse. And, perhaps, even more tragic, is after this happens, you are basically on your own. Traditional medical doctors already think you’re “crazy”, are dismissive, and/or try to return you to the very people who, basically, did this to you. I am not trying to complain or be vindictive. I only wish more people could be aware of this, but, there are few websites or places we can go and with the present “virus” situation”, these places have become less and less. But, I still have hope that all of this too will change in our favor. And, then, not only will our lives improve, but we might be able to help others avoid the terror that we were forced to experience. Thank you.
Report comment
Imagine that scenario happening with any other trauma. A victim of rape being told to go see her rapist in order to get over her rape. A former disabled prisoner of war being told they need to go to the people who imprisoned them to get help for their blown off legs. If the person doesn’t do so they are called crazy, and blamed for not helping themselves. That is what happens to anyone who has escaped the prison of psychiatric drugs.
It is difficult to become okay with trauma. It’s harder when the trauma was society giving you brain damage. It’s even harder when that society insults and blames you for the harm they caused and tell you to go get more brain damage to fix it.
Report comment
How about when you are told that your trauma is a cause for celebration and “pride”?
Report comment
I’ve lived it, being on disability. I have my next CDR (continuing disability review; E.G. “Why aren’t you in treatment? You need to be in treatment. You have to go see these psychiatrists for your consultative exams,” etc.) coming up next spring, where it’s going to become an issue yet again. The last time almost killed me, and I wound up in jail at one point as a result of the binge drinking and emotional turmoil. Just another day in the world of psychiatry.
Imagine someone who were receiving disability for being blind or partially paralyzed, etc, being treated this way.
Report comment
Ugh Jeffrey, sorry you have to endure that.
I guess you could always say “I’m HERE on disability, BECAUSE of treatment” and that it is your, “civil right to avoid further damage
Report comment
Psychiatrists, especially ones called upon by the state, just absolutely love “patients” that are asserting their rights, especially “hostile” ones that are committing heresy. The standard routine is to take a fistfull of benadryl so you’re all sick and drowsy and cognitively impaired, blame it on the “side effects” of the “medication” you get from your GP, then they’ll likely refer you to the community mental health services, which you throw in the trash when it’s over. Talk about how your life and daily activities revolve around avoiding triggers, coping with side effects, etc.
I do believe there is an MIA blogger, Eric Coates, who got sent to a state mental hospital and then put in AOT for essentially doing what you suggest; although in his case went to a psych unit voluntarily in distress, blamed prior treatments, wanted “treatment” without drugs, suddenly was perceived as “hostile” and then off he went. Not even being a blogger here and a former professional publisher (or was it published author?) could help him. In fact in one of his court hearings, his former professional life was mocked as being a grandiose delusion.
Oh, and then of course there was the “candle incident” … smh … something the psychiatrist pulled out of thin air and then moved on, influencing the court into thinking there was some sort of “incident” when there wasn’t. He was even admonished for having a high level of intellect, being told he was too smart for his own good when it came to being a psych patient.
The only way I can avoid a potential fate like this, is to find a source of income and get off disability before the CDR comes up.
Report comment
It’s even harder when that society insults and blames you for the harm they caused and tell you to go get more brain damage to fix it.
Do you have an analysis of why this happens and in whose interest it may be?
Report comment
“I remember having to be taken off “abilify” because it closed my throat to the point I could not swallow. Of course, then they put me back on risperidal, which, they had taken me off earlier for the “abilify” because “abilify” was such a wonder drug!”
And where is your justice? In a perfect world, you’d be awarded millions.
Report comment
Unfortunately, it’s not a perfect world, because, if I ever got those “millions”, I put some of it into something that would help those so damaged by these drugs and therapies. Oh, by the way that incident I mentioned in my comment is only one of many. I could write a book; but, my memory of those years on those drugs; especially, about ten or so years of it is very vague and at times comes and goes. There is no way I could find out what drugs, dosages, and when. Also, many of the psychiatrists, and therapists retired or left the employer. One psychiatrist, in particular, moved to another state, basically across the country. I had one psychiatrist who literally dropped at the end of the session; although I was still on several drugs, because of the health insurance I was on at the time and the deductible associated with it. She said that you people with that kind of health insurance never pay because of the deductible. I remember this because this was actually prior to the about ten years I was so drugged that, well, now really, “lost years” to me. Thank you.
Report comment
When I was in intensive care with Seroquel induced acute pancreatitis my friend called my psychiatrist’s office to tell him that. Because they couldn’t comprehend “pancreatitis” they put in my chart that I was in the “ICU with psychosis”. I know this because I have my psychiatrist office notes.
It took me 16 years until my eyes were open by the fraud of their psychiatry. Add in the years it took me to taper off the drugs. I call those my Rip Van Winkle years. Slowly waking up from a drug fog, the slow recovery of mind and body.
Report comment
I was reading your story. There are some similarities to mine; as, I do ended up in the hospital because of what the drugs did to me. And, all the doctors lied and made up stuff about how I got there and my condition, etc. And, I, had my onw personal “Rip Van Winkle” years; years that are lost and memories that I don’t even have. And, now, I am awake and for the few who still know me, that can be quite disconcerting at times. Thank you.
Report comment
Well, it was a wonder drug all right. You’re probably still wondering why they prescribed it in the first place.
Report comment
Rebel, you said it very well. How many are in just this situation? “Regular” doctors don’t believe psych patients, much less former psych patients, and we have to live in fear of saying too much or saying the wrong thing for fear the doctors will send us back to the ones who caused all the damage in the first place. I’ve been in this exact situation for years. No one who hasn’t been through it understands that it can actually be dangerous for me to seek medical attention if any sort. My body always goes into a trauma response whenever I’m in a medical setting, and my blood pressure shoots up. It’s just an awful situation, particularly as I age and my health problems get worse.
Report comment
I thought it was common knowledge that ‘antipsychotics’ often ‘masked’ the symptoms of Tardive Dyskinesia until the drug was withdrawn. Do the new “TD drugs” operate in the same way?
Report comment
Yes. The drugs for TD like neuroleptics cause cognitive impairment making it harder for the person to recognize what is going on and complain. They also cause sedation; if you’re passed out in bed it’s harder to see/have movement. The new TD drugs being discussed here reduce dopamine, and other neurotransmitter levels. Neuroleptics block those receptors so both drugs have similar chemical effect. The adverse even data from the corporations show these drugs for TD cause other movement diseases. Other drugs for TD also cause cognitive impairment and sedation by causing chemical imbalances.
Report comment
The “atypical” antipsychotics can create the symptoms of TD, when given in egregiously large doses, as is often done by today’s psychiatrists. I know because it happened to me. In as much as my psychiatrist lied, and claimed the movement disorder was absolutely not caused by his treatments. He did start to wean me from the drugs, which did largely cure the problem. I was left with an issue of an occasional wiggly ankle when I wake, but this isn’t a huge problem.
Report comment
I think, what we must not forget, is how much “mainstream media” is involved. Robert F. Kennedy Jr. on his website, Children’s Health Defense. org, has documented how much “Big Pharma” has almost bought and paid for the major networks and cable networks; including their evening news, etc. Thank you.
Report comment
That’s why we really must make direct to consumer advertising illegal again.
Report comment
“TD is regularly presented as a disorder of involuntary movements,” I remember for years that NAMI referred to it as a “muscular side effect” in the 2000’s and early 2010’s, maybe they still do for all I know. Haven’t checked. Outrageous.
Oh yes, when the medicine causes the muscles to become agitated. grrr. Nothing to do with the brain, no brain damage here. And of course the emphasis that the “side effect” affects “muscles”.
Report comment
This may be the most relevant investigation by RW in a while, or at least the most timely given the current spate of TD drugs on the market, each one accompanied by an Orwellian TV commercial..
One of the most frequent targets of the Mental Patients Liberation Movement was the use of drugs that caused TD, primarily Thorazine and the other phenothiazines. The psych industry treated TD the way the tobacco industry treated lung cancer. This was the impetus for a movement-led consumer boycott of the SmithKline Corporation, and supposedly for the development of non-phenothiazine “alternatives” to the original poisons.
It is thus beyond parody that the industry now turns around more than a generation later and trumpets the perils of TD (a form of permanent brain damage) and proudly announces a new neurotoxin to, presumably, suppress the effects of the original one. (No word yet on whether the “patient” still sits like a potted plant but without twitching and jerking muscles.)
Report comment
Reminds me of the Star Trek Next Generation episode where people from one planet got everyone on another planet addicted to a substance only found on the first planet, and then said they all had a “disease” for which their drug was the only “treatment.” And of course it was VERY expensive, but what’s it worth to be protected from this horrible “disease!”
It is beyond despicable to create a “disease” with one drug and then sell another to “cure” it!
Report comment
Creating a disease and then a drug to cure it…sounds so familiar, what could I be thinking of ???
Report comment
Invent a disease and you’ve got a fictive ailment (schizophrenia). For this fictive ailment, a very real drug induced disease (Parkinsons) can be seen as the “cure”, replete with further and more devastating damage in the form of Tardive Dyskinesia, and now they’ve got drugs for the disease created by the drugs. For a get rich scheme, these big pHarma exes really knew what they were doing, didn’t they?
The real dope is, maybe you’d be better off thinking about doing something besides…dope.
Report comment
Isn’t there a prediction made long ago: the love of many shall wax cold? Maybe we have replaced love with chemicals.
Report comment
Up to $7,000 per month equalling (up to) $84,000 per year – Who Pays??
Report comment
The same people who begrudgingly pay $9,000 (or that is, allow a recipient to receive) a year to a person on disability for having been harmed on or having to take such drugs.
Report comment
I’m thinking jeffrey that if the visits to a shrink, the cost of meds, cost of incarcerations were given to the people, then there would be a lot of people out of business. See, those people who treat the kids, are taxpayers, who pay the pittance for the ones they did not help to have bits of success.
It’s the wonderful world of design.
I think we’re still working on the kinks of being human. It’s fascinating that a few get to say who is fucked up.
Report comment
Maybe they should just pay the “patient” the amount they WOULD have paid the drug companies and the doctors. I bet that “depression” would drop markedly as a result!
Report comment
I used to say/point this out a lot. We have homeless people on the streets who can honestly say the tax payers have “invested” millions of dollars on them, and yet there they are. I remember reading an article that described a psychiatrist “panicking” because a revolving door homeless patient had not shown up as usual… Oh no, there goes my cash cow!
Report comment
The really hilarious part is when they give people $9,000 a year then say they have “money management problems.”
The amount of welfare and disability funds dispensed from the capitalist coffers is roughly gauged based on what it takes for most people to sit back and take it, rather than rise against the system itself.
Report comment
Yeah, seriously! I’d love to see any of the “mental health professionals” live on double that a year.
Report comment
I know a chap in London who gets a decent rate for being “mentally ill”, he’s prescribed medication which he can take or not take – and the doctor is happy as well!
Report comment
They’re probably hoping that the government will pay. Psych patients on drugs aren’t exactly at the top of the income ladder.
Report comment
Extraordinary report. Thank you Mr. Robert Whitaker for exposing another example of rapacious avarice occluding common decency and the sensible assessment of evidence. The pile of evidence is clearly pointing at greed as the primary motive for the prescription of psychiatric drugs (and usually of those not in a position where they are obliged often to meet the victims of their prescriptions).
Report comment
TD brain damage produces involuntary movements and behavior that makes a person look crazy to “normal” people. The charlatans want to promote the belief the crazy person is a real thing, a thing that would exist without a psychiatrist and people jerking around does sell the need for a doctor. but the doctor created the problem shhh shhh now.
Narcissism was recently invented and it does describe psychiatry
4 traits
1. They will never apologize. I am helping you! Don’t you want help?
2. They will never assume responsibility of their faults. This article on psych drugs effects , etc
3. They will never be introspective. Is the patient really ill? Am I helping the patient? Am I a doctor?
4. They will never be forgiving. The patient will always be mentally ill or temporarily in remission.
Report comment
Thank you Markps2
Report comment
“4. They will never be forgiving. The patient will always be mentally ill or temporarily in remission.”
Or lack insight into their illness, and have delusional thinking regarding their benevolent doctor.
Report comment
This is where the idea that only psychiatrists should be writing the history of their profession is so ludicrous and vulnerable. Edward Shorter says as much, only psychiatrists should write the history of their profession, but we know objectivity comes from those with some emotional distance from the subject of any study. Not only, in other words, should we be talking back to power, we should be using science and history to expose the wrong actions taken by people in power. History as cover up is not good history.
Report comment
https://youtu.be/gBCiWt-4Cm4?t=50
“The added stigma, is hard to bare.”
And perhaps worst of all, people quit taking the neuroleptics! *gasp*
People need to be empowered to know that their -I imagine- power tripping doctor is right in doubling down for the 50th time and punching home the order that more drugs is the solution.
Oh and what a bombshell! Don’t forget to use #tdawareness when you share this and related articles/content! In fact if MIA hasn’t, they need to go back and re-tweet the announcement of these articles with that hashtag.
Report comment
I coincidentally just stumbled upon an old book that’s been laying around in boxes of such, entitled Tardive Dyskinesia (“Task Force Report 18”), published in 1979 by the APA. If I find anything remarkable before this thread is kaput I’ll report back.
Report comment
I have TD…I’ve had it for years. A sleep clinic diagnosed it as “Restless Leg Syndrome” and prescribed something for it and “it went away” When I started tapering off an “anti-psychotic,” the TD was unmasked again. Now, my legs shake, sometimes violently, when I try to go to sleep and when I wake up. As I sit here typing, my right leg is shaking. I knew someone whose TD was so bad, he couldn’t sit still or fall asleep. It was so bad, he killed himself over the prospects of having TD for the rest of his life…
This article by RW makes me angry over knowing my precious brain is damaged and that the damage might be “global” and spread as I age and continue with my tapering…WOW, angry, angry, angry at so-call “psychiatry.” I fell into the cracks of the “mental health industry” in 1989 and I’m 71 now. I also have debilitating sexual dysfunction that the Urologist says is due to both psychiatric chemicals and diabetes which is also caused by the psych chemicals/neurotoxins.
I “found” MIA four years ago this Fall and appreciated the comment/discussion section on the articles.
I don’t favor lengthy comments. Thank you to all the writers and commentators. Fuck psychiatry!
Report comment
That is so awful! Thanks for sharing your story, and I’m so sorry this has happened to you!
Report comment
Thank you Steve. Yes, it’s “awful” what these neurotoxins do to so many people and will continue to do to even more innocent “victims.” This article about TD makes me think of your book, “Jerk Radar” in that the psychiatric/pharmaceutical industrial complex are the “Jerks,” the domineering, control freaks, who we all need to be cautious about. To use a “street term,” many of us have been “slimed” by the drug pushing prescribers.
Many of us have been “slimed” by the biochemical medical model ideology that acts as a “meme,” a virus in the brain that casts its spell on the minds of its unsuspecting, innocent, victims. The old saying about “putting a bug in their ears” via ingenious copy writing (propaganda) is a tool of choice for these “Jerks.” I’m no longer “under the spell” of the biochemical medical model sales and marketing propaganda campaign…
I’m wondering when Sammi Timimi’s book “Insane Medicine” will be available for purchase. I want to send a copy to my Congressman and plead for a Congressional Hearing on the subject of corrupt psychiatric and pharmaceutical practices. This book is a much needed “whistleblower.”
As I was searching for information about purchasing S. Timimi’s book, I came across a “paper,” published in a journal called Sociology of Health and Illness, about how the WHO is encouraging member states to adopt “Westernized Psychiatry” and that it is “problematic.” Here’s the URL of the paper: https://onlinelibrary.wiley.com/doi/pdf/10.1111/1467-9566.12230
I want the writers at MIA and the overseas affiliates to read this paper and write an article on it. The title of the paper is “Poles apart: does the export of mental health expertise from the Global North to the Global South represent a neutral relocation of knowledge and practice.” This is “Capitalistic Colonization” at it’s rampant worst. The WHO is encouraging the dangerous spread of the oppressive, commercialized, profit driven, biochemical medical model ideological/war that kills people.
I urge everyone to read the above mentioned paper.
Report comment
“Jerk Radar” concepts are most definitely applicable to psychiatry. They try to charm you initially with promises of a better life, try to quickly engage you with them intensely to isolate you from other help, interfere with other relationships by explaining how they have your best interests at heart and that anyone disagreeing with them is undermining the relationship. Big egos abound, with willingness to lie or manipulate to maintain control, and willingness to blame others for anything that goes wrong. Low responsibility – goes without saying. History of abuse, encouraging others to use drugs, employing denigrating labels and comments… the concordance is quite thorough.
Report comment
Thank you, too
Report comment
bill, I am really sorry you go through this. Psych discredits itself over and over.
The TD they have denied over and over to their subjects, now has a drug made for it, which the deniers will now push.
And they will say “no we never denied it”. They use outright lies to hold up their practice.
Report comment
Double entry, sorry.
Report comment
The psychiatric industry has no qualms about destroying lives under their nefarious disguise of providing “help”. It’s a tedious task exposing these corrupt self-serving charlatans for who they really are.
Thank you Robert for another outstanding and vitally important report.
Report comment
Does anyone know how many yearly deaths can be attributed to “psychiatry’s abusive treatments?”
I’ve heard the Psych/Pharma Industrial Complex is as corrupt, if not more so, than the notorious Tobacco Industry.
Report comment
“8 million deaths” every year, according to the former head of the NIMH.
https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2015/mortality-and-mental-disorders.shtml
Report comment
bill from cleveland, I’m so sorry this suffering has been inflicted on you by psychiatry. And Sam, I just saw this quote today as to psychiatry making more drugs to treat the damaging effects of it’s other drugs:
“Psychiatry is the only profession I can think of in which every failure leads to more profit”
Linda Lagemann Ph. D,. April 2017
Report comment
Wow Rosalee, GREAT quote! Bears requoting.
“Psychiatry is the only profession I can think of in which every failure leads to more profit”
Linda Lagemann Ph. D,. April 2017
Report comment
Tranquillisers will always fail over time:-
“…Seeman, in his studies of drug-induced dopamine supersensitivity, concluded in 2007 that this was why antipsychotics fail over time….”
Report comment
And yet has practice changed significantly since then?
Report comment
Unfortunately, because this is something the medical establishment and not just the Psychiatrists, Big Pharma, and others want to hide this from us; partly due to their hiding this from themselves; each one of us is “flying blind” perhaps into a whirlwind or worse. Robert Whitaker and others have done excellent work and research. We also have each other’s stories as commented on this website; which is one of the few we can frankly speak about our experiences. Yet, do any of us know what to expect not just during the withdrawal, but, after the “drugs?” We really don’t even know if they ever even leave our bodies and brains; as the effect, which is in many ways unique to each person is still there. And, of course, our friends and family members, may sadly think we need to go back on the “drugs” because of some of the weird thing we either experience or show to others. And, there is no doubt, that returning to the “drugs” could very well be a more disabling sentence, if not a death sentence for some. Therefore, I wish, we had a good book or two that could at least act a some sort of guide. It would document some of the experiences people have had and some of the problems we may face. And, perhaps, we could share it with those who tragically doubt the validity of our experiences. But, I dream on. Thank you.
Report comment
Thank you for telling me the truth about the drugs I am taking. No one else will
Report comment
Spray some bugs with bug spray (pesticide) and often you will see that they do not die immediately. They look like they have tardive dyskinesia. These people are in the process of dying no different than the bug hit with bug spray. Neuroleptics are derived from pesticides, didn’t you know? Look up Phenothiazines.
Report comment
Thank you so much for writing this. I learned a lot. I took Abilify for 10 years without hearing once about this disorder. I stopped 6 months ago after my toes started digging into the sole of my shoe and I realized I was at risk for having this. My toes are flexing involuntarily 100% of the time and I’ve noticed tongue/mouth movement more recently. I was told by a neurologist who specializes in movement disorders that I ‘potentially’ have TD, Parkinsonism or Early onset Parkinson’s disease. I don’t know what the odds are that my symptoms will ever go away, and I fear things could get a lot worse even though I’m off the medication. Now I’m still on Wellbutrin and Lamatrogine but I’m going to try to taper down and get off all meds.
Report comment