Five years ago, I spent time as a fellow in a lab at the Safra Center for Ethics at Harvard that was devoted to studying “institutional corruption,” and what I particularly appreciated about the lab was that it provided a clear method to investigate and conceptualize the problem. The framework was this: Identify “economies of influence” that may corrupt the behavior of individuals within the institution, document the corruption, and explore the resulting social injury.
Lisa Cosgrove and I joined together in studying the “institution” of psychiatry through this lens, and we focused on its institutional behavior since 1980, when the American Psychiatric Association published the third edition of its Diagnostic and Statistical Manual. This was when the APA adopted its disease model for categorizing mental disorders, with the profession then taking up the task of selling this new model to the public. This was the particular guild interest that arose in 1980, and has shaped its behavior ever since. We’re all familiar with the second “economy of influence” that has exerted a corrupting influence on psychiatry—pharmaceutical money—but I believe the guild influence is really the bigger problem.
In our book Psychiatry Under the Influence, we then documented the corrupt behavior, which could be found in every corner of psychiatry: the false story told to the public about drugs that fixed chemical imbalances in the brain; the biasing of clinical trials by design; the spinning of results; the hiding of poor long-term results; the expansion of diagnostic categories for commercial purposes; and the publishing of clinical trial guidelines that inevitably promoted the use of psychiatric drugs.
At the end of our investigation, I had a new way of conceptualizing the social injury that was caused by this corruption: our society had organized itself around a false narrative, one that was presented to us as a narrative of science, but was belied by a close examination of the actual evidence.
Now, with the publication of a new study in the American Journal of Psychiatry titled “The Long-term Effects of Antipsychotic Medication on Clinical Course in Schizophrenia,” we have a new opportunity to observe this “institutional mind” of psychiatry at work. The article, authored by former APA president Jeffrey Lieberman and seven other psychiatrists, is meant to serve as an evidence-based review that defends the profession’s current protocols for prescribing antipsychotics, which includes their regular long-term use. By closely examining this review, we can assess, once more, whether this is a profession that can be trusted to honestly evaluate its evidence base and use that evidence to guide its care.
The Context
In 2010, I published Anatomy of an Epidemic, and in that book, I wrote about the long-term effects of antipsychotics, and concluded that there is a history of science that leads to this conclusion: on the whole, antipsychotics worsen the long-term outcomes of people diagnosed with schizophrenia and other psychotic disorders. Joanna Moncrieff has similarly written about the hazards of antipsychotics in her book The Bitterest Pills and in published papers. So too has Peter Gøtzsche in his book Deadly Psychiatry and Organized Denial and various journals.
All of this criticism helped to promote further inquiry into this concern, which put psychiatry on the hot seat: did it prescribe these drugs in a way that caused more harm than good? Did their protocols for the drugs—immediate use for all first-episode psychotic patients and then “maintenance” use of the drugs—need to be rethought?
In their newly published study, Lieberman and colleagues perform what they describe as an “evidence-based” review of these questions. They conclude that there is no compelling evidence that supports this concern. In a subsequent press release and a video for a Medscape commentary, Lieberman has touted it as proving that antipsychotics provide a great benefit, psychiatry’s protocols are just fine, and that the critics are “nefarious” individuals intent on doing harm.
Joanna Moncrieff has already published a blog on Mad in America that is critical of the study, and, in particular, of the authors’ dismissal of studies related to the effect of antipsychotics on brain volumes. Miriam Larsen-Barr, who has done research on user attitudes toward antipsychotics, also wrote a blog criticizing the study and press release, focusing on how the authors ignore user accounts about how the drugs affect their lives.
In this MIA report, I simply want to look closely at how Lieberman and his collaborators reviewed the literature and individual studies. We can then see whether they have done so in a way that reveals the mind of a group interested in truly investigating the question of the long-term effects of antipsychotics, with the patients’ well-being uppermost in their thoughts, or whether it reveals the “mind” of a group interested in protecting guild interests.
Then, at the end of this exercise, we can ask this essential question: If we can’t trust the profession to develop “evidence-based” treatments that put the interests of patients first, as opposed to their own guild interests, what should our society do?
The Authors
The eight authors describe themselves as “an international panel of experts in antipsychotic pharmacology, neuroimaging, and neuropathology.” The task they gave themselves was to “review the preclinical and clinical evidence supporting potential adverse effects of antipsychotics on long-term outcomes.”
From an “institutional corruption” perspective, there is additional information that needs to be added to that description: All eight are psychiatrists, and thus there is a “guild” interest present in this review, given that they are investigating whether one of their treatments is harmful over the long-term. As for the influence of pharmaceutical money, five of the eight report financial ties to drug companies, with at least three serving on speaker bureaus for multiple companies. Lieberman reports no such conflicts of interest, but he has a past filled with such conflicts: in 2009, he disclosed having had financial ties to 15 drug companies in the previous two years.
The Issues
The authors, in their introduction, cite papers by Moncrieff, Gøtzsche and me as raising concerns about the long-term effects of antipsychotics. In terms of clinical importance, the review should serve as an examination of evidence relevant to how antipsychotics are being prescribed. Are they being used in a manner that best serves patients, or in a manner that increases the likelihood that a person who suffers a psychotic break will have a poor long-term outcome?
Psychiatry’s current protocol calls for psychiatric drugs to be prescribed to all psychotic patients, and for “maintenance therapy” over the long term. Placebo-controlled trials provide the evidence for the first practice. Withdrawal studies, where patients stabilized on medications are randomized to continued treatment or to withdrawal (usually abruptly so), support the second.
However, the withdrawal studies don’t tell of how maintenance therapy affects patients over the long term. They simply reveal that once a person has stablized on the medication, going abruptly off the drug is likely to lead to relapse. The focus on long-term outcomes, at least as presented by critics, provides evidence that psychiatry should adopt a selective-use protocol. If first-episode patients are not immediately put on antipsychotics, there is a significant percentage that will recover, and this “spontaneous recovery” puts them onto a good long-term course. As for patients treated with the medications, the goal would be to minimize long-term use, as there is evidence that antipsychotics, on the whole, worsen long-term outcomes.
This is the clinical relevance of this “concern.” Does psychiatry need to rethink its drug-use protocols in order to give patients the best chance to recover and function well over the long term?
The good news here is that the authors, with this paper, are seeking to address the main issues raised by critics. Furthermore, as they performed their review, they revisited many of the studies we “critics” have written about. To a large degree, they have retraced the historical path I wrote about in Anatomy of an Epidemic, which provides a sense of agreement on the evidence that there is to be found and reviewed.
Deconstructing Their Review: Part One
The first part of their review is devoted to assessing the evidence base for use of antipsychotics to treat psychotic episodes, including their use in first-episode patients. Is there evidence that supports treating all patients in this way, or is there reason to develop protocols, particularly for first-episode patients, that would give them an opportunity to recover without exposure to the drugs?
A. Placebo-controlled trials in psychotic patients
In 2009, Leucht published a meta-analysis of 38 trials of second-generation antipsychotics and reported a response rate of 41% for the drug-treated patients versus 24% for the placebo group. Lieberman and colleagues cite this study as providing solid evidence for regularly prescribing antipsychotics to patients experiencing psychotic episodes. “This magnitude of therapeutic effect compares favorably with many of the most effective treatments in non-psychiatric fields of medicine,” they wrote.
What’s missing from their review
While placebo-controlled studies may show whether a drug is more effective than placebo in curbing a target symptom (over a short period of time), they do not provide evidence of the benefit-harm effect that the drug has on all patients so treated. To make that assessment, reviewers need to calculate the NNT in the trial data, which is the number of patients that need to be treated to get one additional positive response. This identifies both the percentage of patients that benefit from the treatment and the percentage that may be harmed by exposure to a treatment they don’t benefit from (e.g., those who would have recovered anyway or are non-responders to the treatment.)
In the meta-analysis cited by Lieberman, the NNT is 6. Although 41% of drug-treated patients are responders, 24% of the placebo patients are too, producing a net increase in responders of 17%. That means for every six patients you treat with the drug, you will get one additional responder, and this is the group that could be said to benefit from the treatment.
The remaining 83% fall into the harm category. There are the non-responders (59%) who didn’t benefit from the treatment but are now exposed to the adverse effects of antipsychotics, and the placebo responders (24%) who would have gotten better without such treatment but are similarly exposed to the drugs’ adverse effects.
If you have a treatment with minimal side effects, then an NNT of six may justify a one-size-fits-all protocol. The additional chance of responding to the treatment justifies taking a risk of exposure to a drug with minor side effects. But in this case, given that antipsychotics have such severe side effects, the Leucht meta-analysis of placebo-controlled trials provides an evidence-based argument for avoiding antipsychotics as a first-line therapy for all patients, and attempting instead to see if other approaches—psychosocial approaches, sleep aids, and so forth—can produce a similar response rate over the short term (41%), without exposing everyone to the hazards of the drugs. The drugs might then be tried as a second-line therapy for non-responders.
The point, for the purposes of this MIA report, is this: reviewers seeking to promote their drug treatment as effective will look solely at whether it produces a superior response to placebo. This leads to a one-size-fits-all protocol. Reviewers that want to assess the benefit-harm effect of the treatment on all patients will look at NNT numbers. In this instance, the NNT calculations argue for selective use of the drugs, for you would want protocols that allowed for “placebo responders” to emerge without being exposed to the drugs, and did not call for drugs to be prescribed on a continual basis to “non-responders.”
B. Placebo-controlled trials in first-episode patients
The Leucht study cited by Lieberman implies that 24% of psychotic patients will recover, or at least partially recover, from a psychotic episode within a six-week period (the usual length of placebo-controlled trials.) However, the trials in the Leucht meta-analysis were conducted in patients who had been exposed to antipsychotics, with the “placebo group” composed mostly of patients abruptly withdrawn from the drugs. They aren’t a true placebo group, and this raises an essential question: What is the recovery rate for first-episode patients who aren’t treated with antipsychotics, and how does this compare to the recovery rate for first-episode patients treated with the drugs?
In their paper, Lieberman and colleagues provide this answer: “No placebo-controlled trials have been reported in first-episode psychosis patients.”
This is a rather startling confession. Since the introduction of antipsychotics in 1955, there has never been a placebo-controlled study in medication-naïve patients to see if the drugs are effective in this group. Yet this initial drug treatment regularly becomes a defining moment in their lives, because psychiatry’s usual protocol is to maintain patients on antipsychotics indefinitely.
This alone should give psychiatry reason to re-examine its practice for treating first-episode patients. It is not evidence-based, and it would seem that the profession, which likes to present itself as practicing evidence-based medicine, would want to remedy this extraordinary deficiency.
C. Studies that have reported recovery rates in first-episode patients, or a cohort largely composed of first-episode patients, that involved treating them with psychosocial care and without antipsychotics
1) Odegard and McWalter
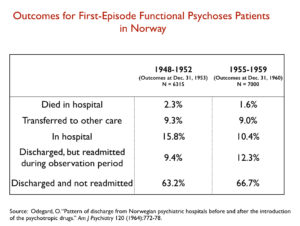
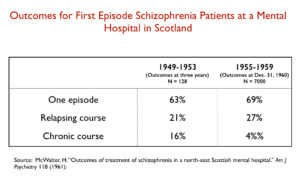
These are two early studies cited by Lieberman and colleagues that compared recovery rates immediately before and after the introduction of antipsychotics. They wrote that these studies showed “increased rates of discharge and reduced rates of hospitalization associated with initial antipsychotic treatment.”
In other words, they are stating that these studies support the immediate use of antipsychotics in first-episode patients, and that this use leads to superior long-term outcomes. It isn’t placebo-controlled evidence, but evidence of a different sort that supports their current practice.
What’s missing from their review
They did not provide any data from these two studies, which, if presented, would argue for selective use of antipsychotics. Here are the data:
In both studies, more than 60% of first-episode patients treated without antipsychotics recovered and never relapsed in follow-up periods of three to five years. They had an episode of psychosis, rather than becoming chronically ill (and thus in need of continual drug treatment.)
It is also notable that the recovery rate—and the longer-term stay-well rate—didn’t really change with the introduction of antipsychotics. At this time, there was not yet the practice of maintaining discharged patients on antipsychotics, and thus the good stay-well rate seen in these studies is for patients who are not being maintained on medications long term.
- May
In the early 1960s, May randomized 228 first-admission patients to psychotherapy, milieu treatment, antipsychotic, ECT, and drug plus psychotherapy. There was no placebo control, but the milieu group provided something close to an “untreated” group. “Patients assigned to antipsychotic (alone or in combination) or to ECT spent less time in the hospital over the subsequent three years and exhibited superior social functioning,” Lieberman and colleagues wrote.
This study is being presented as showing that initial use of the drug led to a better three-year outcome for patients so treated.
What’s missing from their review
They fail to report this important result: 59% of the patients randomized to milieu therapy were deemed “successes,” and over the three years, May reported, “the initial of successes from milieu functioned over the follow-up at least as well, if not better, than the successes from the other treatment.”
Indeed, the milieu successes had the best scores of any of the five groups on social relationships and overall adjustment, which led May to write: “Even though some treatments get worse results on the average, their successes might be of higher, or more enduring quality.”
This is a finding relevant to whether a significant percentage of first-episode patients can be successfully treated without medications, and how such “successes” fare over the longer term. Once again, it shows that about 60% fell into this group, and that this group of “successes” appeared to be of “more enduring quality.”
- Schooler
In the early 1960s, the NIMH conducted a study of 229 acutely ill inpatients with schizophrenia who were randomized to one of three antipsychotics or to placebo. Fifty percent were first-episode patients. While the drug-treated patients had higher recovery rates over the short-term, Lieberman and colleagues noted that “individuals who received placebo during the initial 6-week trial were less likely to relapse after hospital discharge compared within individuals who received phenothiazine.”
Having reported on the better one-year outcomes for the placebo patients, Lieberman and colleagues then dismissed that favorable result in this way: “Because dropout rates due to non-response during the initial randomized trial differed substantially between treatment groups (2% in the phenothiazine group compared with 29% in the placebo group), it is highly likely that the sample for the follow-up study of discharged patients contained a disproportionate number of poor-prognosis patients in the phenothiazine group, since these subjects would not have achieved discharge if treated with placebo.”
What’s missing from their review
First, they failed to report that 67% of the placebo group were discharged, and thus were in this “best outcome” group at the end of one year. This is a finding that appears to duplicate the results in the May study.
Second, in their effort to dismiss the better results for the placebo patients, Lieberman and colleagues assume that it was “poor prognosis” placebo patients who dropped out from the study. However, as modern longitudinal studies have shown (such as Harrow), the drop-outs may be better characterized as “non-compliant” patients, and this is the group that has the better long-term outcomes.
Third, when Schooler sought to explain the better 1-year outcomes for those treated with placebo, she found that the placebo patients were “more likely to have fathers who were mentally ill,” which was a risk factor that “increased the likelihood of rehospitalization.” This difference in the patient groups, Schooler wrote, “would make a higher rehospitalization rate of placebo patients more, rather than less, likely.”
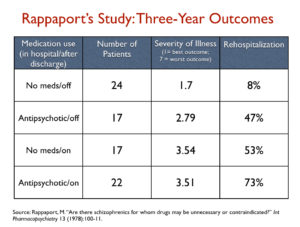
- Rappaport
In this 1970s study “of acutely psychotic patients, most of whom were medication naive,” 127 were randomized to either placebo or chlorpromazine, and followed for three years after discharge. Lieberman and colleagues wrote that Rappaport “reported poorer outcomes over a 3-year follow-up” in the chlorpromazine group, but then dismissed the better outcomes for the placebo patients.
The design, they wrote, is “confounded by unequal attrition rates during the initial treatment phase—45% of placebo-treated patients dropped out compared with 26% of patients treated with chlorpromazine. After correction for the unequal loss of poor-prognosis patients in the placebo group, differences in the outcome were no longer significant between groups.”
What’s missing/wrong with their review
First, at the end of three years, there were 41 in the placebo group who were still in the study versus 39 in the drug group. So there was no unequal “attrition” by study end (see graphic below).
Second, Rappaport wrote that it was “during the follow-up period” that there was a larger attrition of subjects from the placebo group, rather than in the initial treatment phase, as claimed by Lieberman. If this is so, then there must have been a larger attrition of subjects from the drug group in the initial treatment phase (for the numbers in each group to be equal at study end.)
Third, of the 80 patients still in the study at the end, 14 in the placebo group were seen as “bad prognosis” patients at the start of the study, and 14 in the drug group were so designated at the start. Thus, there was no “unequal loss of poor prognosis patients” that confounded the three-year results.
Fourth, the differences in outcomes between the two groups were dramatic. Two thirds of those randomized to placebo were off medication at the end of the follow-up period, and it was this group that, by far, had the best three-year outcomes. At the same time, 57% of those randomized to drug remained on an antipsychotic for the three years, and it was this medication-compliant group—following the prescribed protocols of today for antipsychotic use—that had the highest rehospitalization rate, roughly nine times higher than for the never-exposed group.
Here are the outcomes that Lieberman and colleagues did not present:
Finally, in an effort to investigate the higher attrition rate for the placebo patients in the follow-up phase, Rappaport did this analysis: he threw out the four worst scores in the chlorpromazine/off group, and with this smaller sample size, there were now no significant differences between the never-medicated group and the patients randomized to drug who then stopped taking the medication during the follow-up phase. Rappaport also threw out the five worst scores in the chlorpromazine/on group, but even with this manipulation, the significant differences in outcomes between the placebo/off and chlorpromazine/on groups didn’t disappear.
In sum, Lieberman and colleagues, in their review of this study, didn’t report the actual outcome data from this study, and dismissed the much better outcomes for the off-med groups with an inaccurate description of Rappaport’s investigation into the effect of attrition rates. Lieberman and colleagues, in their bottom-line summary of the study, stated that there were no significant differences at three years between those randomized to placebo and those randomized to drug, when, in fact, the study told of placebo/off patients doing quite well, and medication compliant patients doing quite poorly.
Rappaport made this clear in the study abstract: “Our findings suggest that antipsychotic medication is not the treatment of choice, at least for certain patients, if one is interested in long-term clinical improvement. Many unmedicated-while-in-hospital patients showed greater long-term improvement, less pathology at follow-up, fewer rehospitalizations, and better overall functioning in the community than patients who were given chlorpromazine while in the hospital.”
- Ran
Lieberman and colleagues cited this Chinese study in a section of their paper devoted to this question: “What is the clinical evidence that initial treatment affects long-term outcome?” In this section, they also cited the Odegard, McWalter, May, Schooler, and Rappaport studies, and thus they are positioning the Ran study as one that provides findings on patients treated initially with and without medications, who are then followed for some time.
Ran’s study, they said, was a “14-year follow-up comparing medicated with never-medicated individuals,” and they described the results in this way: “Outcomes were poorer in the never medicated group, including rates of partial and complete remission, homelessness, and mortality. Approximately 10% of individuals who had never been treated achieved remission, and approximately 8% were partially remitted compared with 30% and 37%, respectively, in individuals who regularly took medication.”
Given the context, the readers are left to understand that this study provided evidence that initial treatment with medication, and subsequent “regular” medication use over the next fourteen years, produced superior outcomes.
What’s missing/wrong with their review
This study did not compare the long-term outcomes of non-medicated psychotic patients, beginning with the identification of such patients early in the course of their illness, to a similar group of medicated patients. Lieberman and colleagues have completely misrepresented this study: its design, the makeup of the patient cohorts, their medication use, and, apparently just for good measure, their outcomes.
In the study, Hong Kong investigators surveyed a rural community of 100,000 in China, and identified 510 people who met the criteria for a diagnosis of schizophrenia. This was in 1994, and at this baseline moment, there were 156 who had never been treated and 354 who had received antipsychotic medication at least once, and thus were deemed the “treated” group.
The “untreated” group were on average 48 years old and had been ill for 14 years. Anyone in this rural community who, in the years before 1994, had suffered a psychotic episode and recovered without treatment would not have shown up in this study. In layman’s terms, the investigators had identified a group of “chronically crazy” people for their “untreated” group they would now follow for 14 years.
The “treated” group were not, in fact, a “regularly” medicated group, not even at baseline. They were simply a cohort of patients who had received antipsychotic medication at least once before the start of the study. There is no information given on how many in this group were taking a medication in 1994, when the study began.
At this baseline moment, the chronic, untreated group was much more severely ill than the “treated” cohort, the investigators noted. The untreated cohort was “significantly older, less likely to be married, more likely to have no family caregiver and to live alone, had a lower education level, and fewer family members.” The untreated group also came from families with a significantly lower economic status, and they were more likely to have been abused by their families. In addition, the never-treated group had a “longer duration of illness; higher mean scores on the PANSS positive subscale; and had higher PANSS negative subscale and general mental scores.” Eighty-three percent had “marked symptoms/or were deteriorated,” compared to 54% of those in the treated group.” Only 17% percent were in partial or complete remission at baseline, compared to 47% of those in the treated group.
Over the next 14 years, there were many in the “untreated” cohort who continued to go without treatment, and the researchers reported the remission rate for this “never-medicated” cohort at study end. As for the “treated” group, the investigators did not report on their medication use during the 14 years. They do note that in the last year of the study, 2008, only 11% of this “treated” group took a second-generation antipsychotic even once. There is no information given about whether any in this group were taking a first-generation antipsychotic at that time.
In their review, Lieberman and colleagues did not mention this. They present it as a long-term study that compares medicated to unmedicated individuals, when in fact it is a study that compares a select group of older chronic patients to a less ill group that, at some point in their lives, were “treated.” Patients in this second cohort who weren’t taking an antipsychotic at baseline and did not take any medication over the next 14 years would still have been counted in the outcomes for the “treated” group. Yet, Lieberman and colleagues describe them as “regularly medicated” during the 14 years.
In addition, Lieberman and his co-authors also got the remission numbers wrong. At the end of 14 years, the remission/partial remission rate for the chronically ill, unmedicated group was 30% (not 18%), and it was 57% for the treated group (not 67%.) They deflated the remission rate for the group they described as “unmedicated,” and inflated the rate for the group they wrongly described as “medicated.”
And this is a study they cited as providing evidence that initial treatment with medication produced better long-term outcomes.
- Seikkula
In the past 15 years, Jaakko Seikkula has regularly reported on the five-year outcomes of first-episode psychotic patients treated with Open Dialogue Therapy in Western Lapland, a protocol that avoids immediate use of antipsychotics. Two thirds of their patients have not been exposed to antipsychotics at the end of five years, and are asymptomatic and functioning well. However, Lieberman and colleagues do not cite this study, even though it provides evidence, consistent with earlier studies, that 60% of first episode patients, when provided with psychosocial care, can recover without the use of antipsychotics.
- Duration-of-untreated psychosis studies
To make their argument that initial treatment with antipsychotics leads to better long-term outcomes, Lieberman and colleagues cited a meta-analysis of 33 studies that found “modest correlations between a longer duration of untreated psychosis and residual positive and negative symptoms and impairments in social functioning.” They also noted one “quasi-experimental study” that found a reduction in “the gap between onset of psychotic symptoms and treatment with antipsychotics was associated with improved long-term outcome,” with this study lasting two years.
What’s missing from this review
These duration-of-untreated psychosis studies do not compare initial treatment of a psychotic patient with an antipsychotic to a no-medication regime. All of the patients in these studies are treated with antipsychotics; the difference is that one group has been ill a shorter time than the second group before getting into treatment.
As Sandy Steingard wrote in an MIA blog several years ago, there isn’t a clear picture, from these studies, of whether shortening the time of psychosis before treatment with an antipsychotic produces a meaningful difference over longer periods of time. The results have been conflicting. But researchers did find that a longer delay in patients getting psychosocial care led to an increased likelihood that patients would be suffering from negative symptoms at six years.
Early treatment with psychosocial care may produce a benefit, and perhaps that early treatment would be even greater if combined with the absence of neuroleptic treatment.
Deconstructing their Review, Part Two
In the second part of their study, Lieberman and colleagues focus on the “long-term effects of antipsychotic medication on clinical course in schizophrenia.” They reviewed longitudinal studies, evidence on whether antipsychotics shrink the brain, and concerns that antipsychotics induce a dopamine supersensitivity that make patients more biologically vulnerable to psychosis over the long term.
A. Longitudinal studies
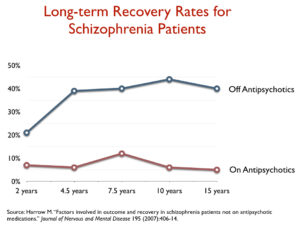
- Harrow
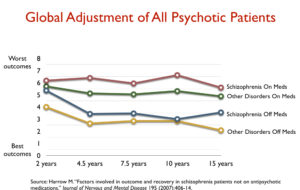
This is the best prospective, longitudinal study that has been conducted in the modern era. Harrow, with funding from the NIMH, followed a large group of psychotic patients, including 64 diagnosed with schizophrenia, for more than 20 years, and periodically assessed their outcomes, with patients grouped according to their use of antipsychotics. Here is what Lieberman and colleagues wrote—in entirety—about this study, which they lumped together, in the same sentence, with their report on a Finnish longitudinal study by Moilanen.
The two studies, they wrote, “found superior outcomes in individuals who were previously treated but not taking medication at the time of assessment compared with individuals taking medication. However, nonmedicated patients had more favorable premorbid characteristics in the study by Harrow and colleagues and had less severe illness in the study by Moilanen and colleagues, suggesting that in naturalistic uncontrolled studies, medication status may in part be the consequence of whether patients are doing well or poorly rather than the cause.”
In short, they acknowledge that the outcomes were “superior” in the Harrow study and also in Moilanen’s, but dismiss these outcomes by stating that the unmedicated patients were less severely ill at baseline.
What is missing/wrong with their review of Harrow’s study
There is no other longitudinal study in the literature that rises to the level of Harrow’s in terms of providing rigorous, comprehensive data on the different long-term course of medicated and unmedicated psychotic patients. He enrolled 200 psychotic patients into the study, from two Chicago-area hospitals (one public, and one private), and they were a young group, with a mean age of 22.9 years. Nearly half were first-episode patients, and another 21 percent had only one previous hospitalization. All were treated in the hospital conventionally with medications, and after they were discharged, Harrow conducted regular follow-ups that charted their medication use, their symptoms, and their functioning. He divided his patients into different subgroups: good-prognosis and bad-prognosis schizophrenia patients, and patients with milder disorders. At the end of 15 years, he still had 77% of the 200 patients in the study, which is an extraordinary feat. In drug studies, the drop-out rates in even short-term trials will be much higher than that.
Yet, Lieberman and colleagues, in a paper said to investigate the long-term effects of antipsychotics, don’t present any details that would tell of this study’s rigor, and they don’t present any of the outcome data. Moreover, their explanation for the unmedicated patients —that it was because they had a better initial prognosis—is belied by Harrow’s data, and the reason that this can be shown is precisely because Harrow divided the patients into groups with different prognoses.
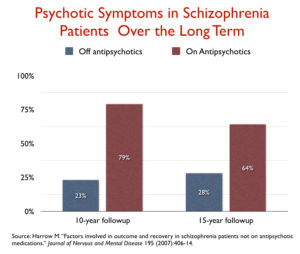
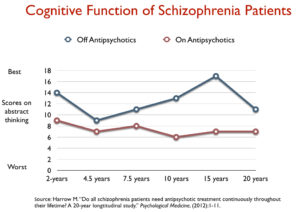
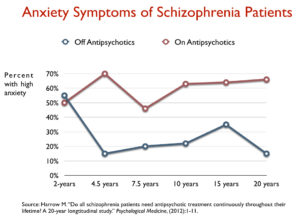
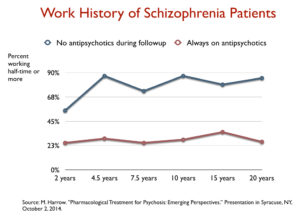
There was a dramatic difference in outcomes, across all domains, for the unmedicated patients, which showed up beginning with the 4.5-year follow-up and remained during all of the subsequent assessments. For those with a schizophrenia diagnosis, the long-term recovery rate for the off-med group was 40% versus 5% for the medicated group. The unmedicated patients were much more likely to be working, they scored better on cognitive tests, and they had less anxiety at every follow-up assessment. Perhaps most notable of all, they were much less likely to have psychotic symptoms at each follow-up, starting with the 4.5-year assessment. Here are the results that Lieberman and colleagues failed to present and discuss:
Having failed to present this data, Lieberman and colleagues then dismiss the “superior outcomes” for the unmedicated patients by stating that this group had more “favorable premorbid characteristics.” There is an interesting history behind this explanation for the difference in outcomes, which psychiatry has clung to even after it was revealed to be false.
Harrow, in his 2007 report, did attribute the better outcomes in the unmedicated group to a difference in premorbid characteristics, as it was the good-prognosis patients who were more likely to go off medication. However, that explanation was belied by this fact: the good prognosis schizophrenia patients who got off did better than the good prognosis schizophrenia patients who stayed on, and that was true for all other subgroups (bad-prognosis patients who got off did better than the bad-prognosis patients who stayed on, and that was the same for those with milder psychotic disorders.) Most compelling of all, schizophrenia patients who stopped taking antipsychotics did better than those with milder disorders who kept on taking the medications.
In his more recent publications, Harrow has acknowledged that this is so. In every subgroup, the on-med groups had notably worse long-term outcomes. In a 2013 article, he summed up his thoughts in this way:
“How unique is that the apparent efficacy of antipsychotics could diminish over time or become ineffective or harmful? There are many examples for other medications of similar long-term effects, with this often occurring as the body readjusts, biologically, to the medications.”
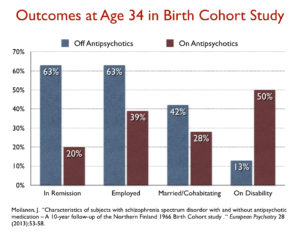
- Moilanen
As noted above, Lieberman and colleagues lump this study in with Harrow’s and dismiss it in the same sentence, stating that the unmedicated patients were less severely ill at baseline.
What is missing/wrong with this review
In this study, Finnish researchers identified 70 patients born in 1966 who were diagnosed with schizophrenic psychoses. They assessed the status of the patients in 2000, when they were 34 years old (with a mean duration of illness of 10.4 years.) At that time, the 24 patients off medication were doing much better than the 46 patients on antipsychotics: they were more likely to be working, more likely to be in remission, and had better clinical outcomes. In short, it wasn’t that the non-medicated group in this study were “less severely” ill when initially diagnosed, but rather that a decade after initial diagnosis, those off medication were doing much better than those on the medication.
The researchers then followed the 70 patients for another nine years, and those who used antipsychotics less than 50% of the time were more likely to function well, be in remission, and have a good clinical outcome.
As was the case with their presentation of the Harrow study, Lieberman and colleagues didn’t report the data, and they explained the “superior outcomes” away with a claim—that the unmedicated group was less severely ill—that is not found in the study itself.
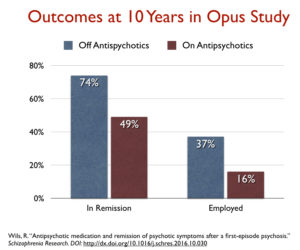
- Wils
There is one other longitudinal study that provides long-term outcome data based on the patients’ use of antipsychotics. This one is a Danish study of 496 first-episode schizophrenia-spectrum patients diagnosed from 1998 to 2000. At the end of 10 years, there were 303 patients still in the study, 121 of whom were deemed “non-compliant” and off medication. There were no differences at baseline between the non-compliant and on-medication groups at 10 years.
Here are their 10-year outcomes:
This study was not cited by Lieberman and colleagues.
- Tiihonen
In their review of longitudinal studies, Lieberman and colleagues spent one sentence on the Harrow and Moilanen studies, didn’t cite the Danish study, and then wrote that “other naturalistic studies have found improved outcomes in individuals with schizophrenia who continued antipsychotic medication compared with those who did not.” They gave no details of these other naturalistic studies, but cited two reports by Tiihonen and his Finnish colleagues.
What is wrong with this review
The Tiihonen articles are not outcome studies at all, and they are not studies of specific known patients. They are both reports by a Finnish group that mined a national registry of drug prescriptions to report relapse and mortality rates for psychotic patients, organized by their current antipsychotic use.
In the first study, they identified 2230 adults hospitalized for a first episode of schizophrenia from 1995 to 2001, and then charted their medication use for every 30-day period following discharge (based on a national database for community prescriptions of antipsychotics). Any relapse or death during a 30-day period was chalked up to outcomes for the particular antipsychotic they were on, or chalked up to “not antipsychotic drug” if they didn’t fill a prescription during that month. Given this methodology, anyone who came off a medication and relapsed would show up in the outcomes for “no antipsychotic drug,” and if someone committed suicide after discontinuing a medication, this too was chalked up to the outcomes for “no antipsychotics.” They found that there was a higher risk of relapse during months of “no medication,” which, as much as anything, may be due to the high risk that comes with being placed on an antipsychotic and subsequently trying to come off it.
In the second study by this same group, they reported on mortality rates of patients with schizophrenia based on length of exposure to antipsychotics over a 11-year period. The researchers reported that “long-term treatment with antipsychotic drugs is associated with lower mortality compared with no antipsychotic use.” They did so by mining the same database of community prescriptions of antipsychotics.
This study, while not an outcome study, has been cited as evidence that long-term use of antipsychotics reduces mortality in schizophrenia. However, as critics of this study have found, deaths of hospitalized patients were not counted, which led to an exclusion of “64% of deaths on current antipsychotics.” In addition, the group with the lowest mortality rate, by far, were those who used antipsychotics less than six months over the 11-year period, as opposed to those who used antipsychotics regularly.
As such, the Tiihonen studies cannot be described as “naturalistic studies” that found “improved outcomes” in medicated patients. They weren’t studies of known patients; they didn’t chart outcomes over longer periods of time (severity of symptoms, cognition, and functional measurements); and there is reason to argue that mortality rates were lowest in those patients who used antipsychotics for only a short time.
B. Brain shrinkage
Lieberman and colleagues review a number of studies regarding the effects of antipsychotics on brain volumes, and whether such changes are associated with clinical worsening, cognitive decline and functional impairment. The conclusion they came to can be summarized in this way:
- It’s not clear whether the brain shrinkage seen in schizophrenia patients over time is due to the drug or the disease.
- It’s not clear whether this loss of gray matter in schizophrenia patients is associated with clinical worsening, cognitive impairment, or functional impairments.
- The matter needs further study.
What’s missing from their review
An effort to assess the long-term effects of antipsychotics requires, most of all, seeing if evidence of different types fits together. The question of their long-term effects arises from the longitudinal studies: why do the unmedicated patients in Harrow, Molainen, and Wils have better long-term outcomes, and on every domain that is measured? The conventional belief has been that antipsychotics are an essential treatment, and yet the longitudinal data belies that belief. This leads to a search for research that might provide a biological explanation for the outcomes seen in the longitudinal data.
The brain-shrinkage data needs to be viewed in that light. What does research show? There is evidence from multiple researchers, in the U.S. and abroad, that antipsychotics shrink the brain, and that this shrinkage is dose related. The same neurotoxic effect can be seen in studies in rats and monkeys, and in those animal studies, the shrinkage cannot be attributed to the disease. And as Joanna Moncrieff noted in her blog in response to Lieberman’s article, there “are no studies that show progressive brain changes in people diagnosed with schizophrenia or psychosis in the absence of antipsychotic treatment.”
There are also studies that have found that this shrinkage correlates with increased positive symptoms, increased negative symptoms, and declines in cognition and functioning. This is data that completes the picture: Longitudinal studies tell of worse outcomes for medicated patients, and MRI studies tell of drugs that shrink brain volumes, and that this shrinkage is associated with worse outcomes. The two data sets combine to tell a coherent story.
In her blog, Moncrieff provides a detailed critique of the review by Lieberman and colleagues of the brain-shrinkage literature. But their biggest failure in presenting this research could be said to have begun in the earlier part of their paper, when they failed to present the outcomes from the three longitudinal studies, and pretended that Tiihonen’s two published articles represented naturalistic studies that found better long-term outcomes for medicated patients. They never presented the longitudinal data that fits together with the brain-shrinkage research to present such compelling evidence that long-term use of these medications worsens aggregate outcomes.
Yet, even though they failed to present the longitudinal data, their review of the brain-research still led them into an intellectual quagmire. How could it be that the reduction in brain volumes seen in psychotic patients was related entirely to the disease and not at all to the drugs, when the shrinkage has also showed up in animals treated with the drugs? They came up with this explanation: “The relevance” of such findings “is uncertain, due to species related differences and because animals lack the pathophysiology of schizophrenia.”
With that explanation, they were setting up the notion that drugs that shrink the normal brain don’t affect the “psychotic” brain in the same way, and this led them to speculate about whether the reduction in brain volumes observed in schizophrenia patients, even if due to the drug, is a bad thing. Yes, in normal people the loss in gray matter correlates with a drop in IQ, but perhaps it has the opposite effect in people with psychotic diagnoses. “It is possible that antipsychotics may have deleterious effects on normal brain but protective effects in the presence of schizophrenia-related neuropathology.”
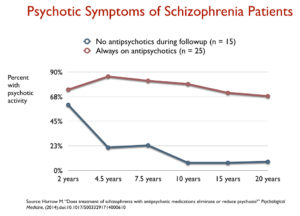
C. Dopamine supersensitivity
In the late 1970s, Lieberman and colleagues write, the concern arose in psychiatric research circles that antipsychotics induced a dopamine supersensitivity—a change in the density of dopamine receptors—that could make patients more vulnerable to relapse than they would be in the normal course of their illness. This could explain why relapse rates are so high in withdrawal studies, and why so many patients treated with antipsychotics become chronically ill.
Lieberman and colleagues do acknowledge that antipsychotics induce a “rapid increase in D2 receptor density.” But, they said, two withdrawal studies provide reason to doubt that this is a problem. In one, the speed of tapering (abrupt vs. gradual) did not produce different relapse rates for the withdrawn patients, and in a second report, a meta-analysis of studies that had charted relapse following withdrawal, the investigators found that withdrawn patients continued to relapse at a fairly steady rate throughout the first year, and while so did the medicated patients, the difference in the relapse rates between the two groups was sustained throughout the twelve months.
With such withdrawal literature as their guide, they concluded that “clinical studies have not provided compelling evidence that treatment with antipsychotics worsens the course of illness, increases risk of relapse, or causes cognitive deficits.”
What’s missing with their review
As was the case with the brain-shrinkage issue, any investigation of drug-induced dopamine supersensitivity needs to start with outcome data that raised the concern in the first place. In the 1970s, reports of higher long-term relapse rates for medicated patients, as compared to patients not treated with antipsychotics, which were found in the studies by Schooler, Bockoven, Rappaport, Mosher, and Carpenter, presented the field with a conundrum. The withdrawal studies they had conducted showed that patients withdrawn from the drugs relapsed at a much higher rate than the drug-maintained patients. This supported a conclusion that the drugs reduced the risk of relapse. But the outcome data told of higher relapse rates for the medicated patients. How to explain this conundrum?
This led Carpenter to ask a profound question: What if the patients had never been put on drugs to begin with? Perhaps the drugs induced a biological change that made patients more biologically vulnerable to psychosis. This could lead to an increased risk of relapse following drug withdrawal, which would show up in the withdrawal studies. Yet, if patients stayed on the medications, drug-induced dopamine supersensitivity could lead to an increased risk that they would become chronically ill. This would explain the poor results for the medicated patients in the longitudinal studies. The withdrawal studies may not have been measuring the return of a disease, but the risk of going off a drug after the patient’s brain has been changed by it.
Chouinard and Jones fleshed out a biological explanation for what appeared to be going on. The drugs blocked dopamine receptors, and in response to the blockade, the density of dopamine receptors increased, and this made patients more biologically vulnerable to psychosis. They conducted studies in their patients that confirmed their theory, and they concluded that this drug-induced change could lead to more “severe symptoms” than the patients had ever experienced before.
That was the research that was published in the early 1980s, and the modern longitudinal studies, which found higher remission rates in unmedicated patients over the long term, provide new evidence to support the conclusion that drug-induced dopamine supersensitivity increases the risk that a person will become chronically ill (see Harrow, Moilanen, and Wils). To specifically investigate this question, Harrow reported on psychotic symptoms over a 20-year period for those who were medication compliant throughout the study and those who never took any medication from year two onward. Here are the results:
That is the story of dopamine supersensitivity. But Lieberman and colleagues did not present this historical context, and they don’t mention the modern longitudinal data, or Harrow’s investigation of it. They didn’t present the research that makes a compelling case that drug-induced dopamine supersensitivity may worsen long-term outcomes.
All is Well in the Land of Psychiatry
What can be seen here, in this deconstruction of the review by Lieberman and colleagues, is that they presented information, time and time again, in a way that protects guild interests and their current protocols for prescribing antipsychotics.
- They never provide data from the studies showing that 60% or so of first-episode patients may recover without the use of antipsychotics.
- They always dismiss the better outcomes for unmedicated patients in cited studies, arguing that it is an artifact of an unequal comparison for some reason or another (Schooler, Rappaport, Harrow, and Moilanen).
- They report no data from modern longitudinal studies that tell of much better long-term outcomes for the unmedicated patients.
- In their discussions of drug-induced brain shrinkage and dopamine supersensitivity, they fail to discuss information from the larger body of scientific literature essential to assessing whether these drug effects could explain the poor long-term outcomes seen in the longitudinal studies.
Having reviewed the literature in that guild-protective manner, Lieberman and colleagues then drew these conclusions:
- There is “little evidence” that initial use of antipsychotics or maintenance treatment with the drugs have a “negative long-term effect.”
- There are just a “small number” of patients that may “recover from a first episode of psychosis without pharmacologic treatment or may discontinue medication and remain stable for extended periods of time.”
- Randomized clinical trials (Leucht) and drug-withdrawal studies “strongly support the efficacy of antipsychotics for the acute treatment of psychosis and prevention of relapse.”
They were an “international group of experts,” and they had come to a comforting conclusion for the guild: The drug-use protocols the profession has been using for decades are just fine.
The Press Release (and public denunciation of the critics)
In our book Psychiatry Under the Influence, Lisa Cosgrove and I wrote about the duty of a medical profession to honestly assess and report on the evidence for its treatments in medical journals, and to communicate such information in an accurate manner to the public. The article published by Lieberman and colleagues in the American Journal of Psychiatry served as their communication to the medical profession; a May 5 press release by Columbia University Medical served as their communication to the public.
The press release deserves to be deconstructed too, for it ratchets up the telling of a narrative that supports guild interests. The authors are described as an international group of experts, who conducted this review to respond to critics who were raising concerns about antipsychotics that had the potential to “mislead some patients (and their families),” and thus cause them “to refuse or discontinue antipsychotic treatment.” After conducting a “comprehensive examination” of all possible evidence, they made a definitive finding: “For patients with schizophrenia and related psychotic disorders, antipsychotic medications do not have negative long-term effects on patients’ outcomes or the brain. In addition, the benefits of these medications are much greater than their potential side effects.”
If anyone dared to doubt this finding, Lieberman said in the press release, they “should talk with people whose symptoms have been relieved by treatment and literally given back their lives.”
The drugs were once again cast as essential and even as miracle agents (life-savers), and this became the narrative promoted to the public, and was repeated in stories published by UPI and on such websites as Science Daily and Medical News Today. Meanwhile, Lieberman also touted the importance of the study in a Medscape video, describing it as a “major development in psychiatry.” Dressed in a white coat, he said the study “came to a very firm conclusion as to the unquestionably positive benefit of these drugs,” and then he took aim at those who had dared to question their merits in the first place.
“The critics who gave rise to this notion that antipsychotic treatment adversely affects long-term outcomes were sowing seeds of untruth and, in their pursuit of some ideological goal or need for self-serving acclamations, were ignoring entirely the harm that they were causing many people who unwittingly would accept these as credible statements and follow their guidance. As I film this video, the contents of the new article are embargoed, so I cannot reveal the contents just yet. But let me just say that this is an extremely well-composed paper that provides a scholarly and rigorous review of relevant lines of evidence. It comes to a very clear and definitive conclusion that we all should take note of the findings, apply them in our clinical practices, and use them where need be in the education of patients and against the reputation of individuals who are really trying to create mischief for their own nefarious purposes.”
Such were the communications of Lieberman and the Columbia University Medical Center, and a few days ago I received an email from a friend in Iceland, who has been an activist in the user community for some time, that neatly summed up their effects on societal beliefs.
“I was talking to some doctors the other day,” she wrote. “They were very excited about a newly published article. Many doctors from many countries had contributed to this research and the bottom line was that meds are good and they are surely helping.”
The Harm Done
In his video, Lieberman talks about critics “sowing seeds of untruth” and how such “untruths” can cause harm, and I have to agree that sowing seeds of untruth can cause harm. We can see it so clearly in this case of institutional corruption.
The studies that tell of 60% of unmedicated first-episode patients recovering, and of better long-term outcomes for unmedicated patients, speak of an opportunity for psychiatry to grasp: they could change their protocols and give a chance to people who suffer a psychotic episode to recover and get on with lives unburdened by the many adverse effects of antipsychotics. There is an “evidence base” that tells of new possibilities for people so diagnosed.
But Lieberman and colleagues did not present that possibility in this review. Rather they hid it from view. That is an action that does harm to millions of “patients” and their families, and thus to all society. We will continue to live in a society organizing its care—and its laws regarding psychotic patients—around a false narrative, one told to serve guild interests, rather than the best interests of patients.
The Challenge for Our Society
In a study of institutional corruption, the ultimate goal is to present ideas for solving the corruption. Lisa Cosgrove and I admittedly struggled with this section of our book. While problems in psychiatry have become well known to our society, societal focus has been on curbing pharma’s influence over psychiatry. But how can the influence of its guild interests be curbed?
I really don’t know. The problem is that the power lies with the guild and its academic psychiatrists, who pen articles such as this one. They have the standing in society as experts; their papers are published in “medical journals”; and they have access to the press. Mad in America is meant to serve as a forum for critiquing that conventional narrative, but I am pretty sure that psychiatrists in Iceland will not soon be talking about the “untruths” sowed by Lieberman’s article in the American Journal of Psychiatry.
But I do have one wish. I wish that all psychiatric residents would familiarize themselves with this controversy, and read the research articles that have been cited, and then ask themselves: Is this published report, the ensuing press release, and Lieberman’s video the work of a medical profession they are proud to join? Or are they the work of a medical profession that needs to be thoroughly remade, with this remaking to be their gift to the mental health of people everywhere? That could be quite a legacy for a new generation of psychiatrists.





Wonderful article, Robert. Thank you.
Report comment
Thanks for the Great Article.
Schizophrenia:-
Most doctors don’t seem to know what “Schizophrenia” is.
Todays understanding seems to be that “Schizophrenia” is a long term serious chronic and DISABLING mental disorder.
In 1980 I was happy to refuse medication – but In 1983 I could not go without it.
In 1984 I learned that I would have to withdraw very carefully from the Drugs . This was what I did – and this was when my longterm DISABILITY ended.
Report comment
Know what it is? They can’t even define it.
Report comment
truth793810,
I don’t believe there’s any such thing. When I was in hospital (years and years ago) I came across a lot of people with problems but not nothing too special.
Myself, when I stopped major tranquilizers / “medication” I suffered from terrible anxiety – but I found practical ways to cope.
Report comment
schizophrenia is an atheistic, secular world’s explanation of negative spirituality, in addition to the process by which to weed out society’s weird and strange creatures. there’s also things like shock and trauma that impact a person’s well-being. then there’s neglect and malnutrition, lack of education and support, and impoverishment issues. then there’s classism (a ruling class looking to squash and silence the weeded out weird and strange creatures).
schizophrenia is a catch-all but it especially targets spiritual nature (so-called hallucinations).
Report comment
“Most doctors don’t seem to know what ‘Schizophrenia’ is.” If it exists at all, Fiachra. Thank you for this excellent analysis of Lieberman’s claims, Robert. As one of the 83% who fall into the harm from neuroleptics category, I’d just like to also point out that the antipsychotics can create both what appears to the doctors to be the negative symptoms of “schizophrenia,” via what is actually neuroleptic induced deficit syndrome, and what appears to the doctors to be the positive symptoms of “schizophrenia,” via what is actually anticholinergic toxidrome.
https://en.wikipedia.org/wiki/Neuroleptic-Induced_Deficit_Syndrome
https://en.wikipedia.org/wiki/Toxidrome
And since neither of these antipsychotic induced illnesses, that mirror the symptoms of “schizophrenia,” are listed in the DSM they are almost always misdiagnosed as one of the billable DSM disorders, since this is the only way the doctors can get paid. Plus, out of sight, out of mind.
But since the “treatment” for “schizophrenia” can create both the positive and negative symptoms of “schizophrenia,” it is likely that most “schizophrenia” is primarily an iatrogenic illness, as opposed to a “genetic” illness, as the psychiatrists have incorrectly claimed, with zero proof, for decades.
Report comment
Hi Someone Else,
It’s nice to see you again.
You’re Completely Right:-
By not taking their medication (very carefully, with support) the “Schizophrenics”can make Full Longterm Recovery – this can be proven.
Report comment
Thanks, Fiachra, and even without support (other than a nice nurse following my family from PCP to PCP to try to protect me and my children from future iatrogenic harm by more doctors) those of us weaned off the toxic psychiatric drugs can recover.
Although the unrepentant, unceasing, and massive in scope iatrogenic crimes against humanity committed by today’s psychiatric industry will, I think, always be heart breaking to me, especially their defamation and torture of millions of innocent children.
Report comment
You’re 100% right,
I think “Recovery” should concentrate on what actually works – not on wishful thinking.
In the 1930s in parts of Europe people turned a blind eye to killings of the vulnerable as well – and afterwards once the scale was exposed
they hung their heads in shame.
Ireland has a large Pharmaceutical industry and this is sponsored by the Universities and Health Regulators – but it is also experiencing an Epidemic of Homicide Suicide from people taking these drugs.
All of this will have to be accounted for at a later date.
Report comment
Great article, Robert. Your deconstructions of their nonsense and non-science is first class. I’m not sure if I can wait for a new generation of psychiatrists to create a legacy for themselves though as I’m seeing it cause too much unnecessary suffering every day with people I work with who have already been through often horrific suffering. I’m running out of patience. It is monstrous what psychiatrists are doing to people (either unknowingly or knowingly). Psychiatry, as a system of beliefs and ideology, is as bad as Nazism, in my opinion and it is already killing the ‘undesirables’ 15 to 25 years before their time and chemically restraining those who are seen as deviants to social cohesion/genetic purity and it’s all done in the name of compassion and the greater good. Just like Churchill and the British did not wait for reformation and stood firmly against the evil of Nazism before it consumed all its path, I think it is about time MIA stood firmly against the evils of psychiatry and declared itself anti-psychiatry before psychiatry does any more damage to us and our societies. I know that there are good people within the field of psychiatry but its overall emphasis and focus is warped and incredibly dangerous. For me, your outline of what its ‘leaders’ think convinces me more that it is beyond reformation and dangerous ideologies must be challenged head on and not given the respect they feel they deserve. Their lies are not just ruining people’s lives but it is having a huge impact on our communities and societies. I don’t think we have time for a new generation of psychiatrists to make the necessary changes and I honestly don’t see this happening. Bad ideas die or they fester and live on. The sooner the ‘chemical imbalance’ and ‘the psychiatrist knows best’ theories die the better. Most psychiatrists are disabling and killing people and they are trying to silence people that speak the truth. Psychiatry must be stopped before it expands its empire any further. Thanks for all your efforts in being a light to many and continuously speaking the truth. Keep fighting the good fight against the evil forces that are trying to shut you down and discredit you. All the best.
Report comment
I am now age 49. I was diagnosed seriously mentally ill at age 19. If I had taken the psychiatric drugs continuously I would be worse off today from the brain damage. Numerous studies show brain damage from psychiatric drugs. I and all mentally ill people need a fully functioning brain for reason, to be able to reason and communicate.
Any sane person knows you should not punish people before they commit a crime (those in authority image will happen), only after a crime. I never committed any crime to justify my drugging at age 19.
Thank you for criticizing the system Robert Whitaker.
Hopefully, in the future many peoples lives will be extended and they will become better functioning people. Not just slabs of living meat.
Report comment
Regarding “sowing seeds of untruth”. It is they, the psychiatrists who are sowing the seed of fear (of the future). A fear of life without an antipsychotic/a magic pill. A life without a psychiatrist. But reason and logic come from a fully functioning brain not a drugged/medicated one.
Bible “A farmer went out to sow his seed. As he was sowing, some seeds fell along the path, and the birds came and devoured them. Some fell on rocky ground, where they did not have much soil. They sprang up quickly, because the soil was shallow. But when the sun rose, the seedlings were scorched, and they withered because they had no root. Other seeds fell among the thorns, which grew up and choked the seedlings. Still other seeds fell on good soil and produced a crop—a hundredfold, sixtyfold, or thirtyfold.”
How many successful psychiatric patients on antipsychotics VS psychiatric patients off of drugs?
Success being defined as employed and having children. All the other living creatures on the planet have offspring to be considered a success.
Report comment
Comment removed for moderation
Report comment
You’ll love THIS! – youtube put a “must-watch” Trintellix ad on the video.
(Trintellix is pushed for those for whom their regular “anti-depressant” just ain’t workin’!. Trintellix is “Indicated” for so-called “MDD” – Major Depressive Disorder,- only…..
Doesn’t GENERAL Depressive Disorder outrank MDD?
And MDD in turn outranks both Lieutenant and Sergeant depressive Disorder….????….
Ask you health-care provider if drug advice from a TV ad is right for you….
Report comment
Instead of trying to justify the constant use of psych meds, these authorities would be better occupied tramping the Northern Pacific rain forest from Oregon to northern British Columbia, searching for the elusive Sasquatch.
Report comment
if they were truly intelligent, wise, smart people they would know what a sasquatch is.
ever heard the saying “got a hair across your axx”? it means a person is bothered, annoyed.
when someone is covered in hair (SUPER EXTREMELY bothered and annoyed) they decide to abandon society (or society drives them out) and they go live in the woods.
Report comment
Definitely a much needed post. What have you got from Lieberman and company? Of course, ‘guild interests’ speaking. Bias speaks more loudly than the evidence which is being conveniently swept under the rug. Just imagine, we can’t say that anti-psychotic drugs cause brain shrinkage because none of the animals whose brains shrunk after we gave it to them had schizophrenia. As usual, the evidence is presented so selectively as to reinforce their biased presumptions. Somebody has to illustrate, as you have done, that this really isn’t a rigorous effort to get to the truth, instead it’s a matter of reassuring people that all is okay in mental-health-treatment-land, even when it isn’t.
Report comment
But with the right kind of basic help, a person can get well and stay well.
Report comment
Sure, a person can be “in recovery”, and financially dependent, as opposed to ‘fully recovered’, for a lifetime. “Get”ting “well and stay”ing “well” becomes very problematic for the person who “consumes” (uses) “mental health services”, especially when true “mental health” must be a matter of rejecting mindless and lingering continual “consumption” of “mental health services”. “Wellness”, in fact, must become a matter of ceasing to “consume” services. I’d say this “consumption” is one bad habit that requires a bit of moral fortitude to be overcome, moral fortitude that corruption within the ranks often makes all the more difficult.
Report comment
OK, Frank, but how do we *KNOW* that animals don’t have so-called “schizophrenia”? I think you and I will agree, but how do “they” *KNOW* that animals don’t have schizophrenia? See what I mean? What evidence is there, that animals don’t get so-called “schizophrenia”? If the shrinks claim to have “proof” that animals don’t get/have so-called “schizophrenia”, then exactly what is that evidence? I’ll grant that animals can become “anxious”, or “depressed”, but aren’t those simply natural reactions to harmful environments/stimuli?
Report comment
What about the kids? They hand the stuff out like candy to five year olds? What happens to them?
Report comment
….they become cu$tomer$ for LIFE….. Duh!….LOL….
Report comment
Bob,
This is a fantastic post – measured, detailed, incisive. Thank you.
It is truly amazing the degree that Lieberman et al have to distort, avoid, deny, spin, and massage the data of numerous studies in order to deny that there may be significant harm coming from long-term antipsychotic use.
I couldn’t help imagining a fragile house of cards when reading this piece. The long-term use of antipsychotics is extremely fragile, in terms of being totally without a scientific basis of efficacy.
Another metaphor for neurotoxins that came to mind was of a real estate salesman who shows people a perfect looking house – what the visitors don’t see is that the salesman has concealed massive cracks in the foundation, hides the fact that the appliances are non-functional, doesn’t talk about the fact that the floors are rotting away just beneath the surface, and generally minimizes any concern while presenting the few surface “good” elements.
This is why I call neurotoxins when presented as “antipsychotic medications” “simulacrums” – this term means that they give the surface appearance of being effective and genuine, but are in fact shams that are insidiously harmful for most in the long term.
This weekend I watched the disturbing movie Alien: Covenant, which I imagine some here may have seen. In this movie there is a traitorous character, the android David, who gives every evidence of being a friend and protector to visitors newly arrived on a dangerous planet (perhaps a metaphor for newly psychotic patients). His real plans become evident later, when he sacrifices the humans in horrific experiments designed to breed aliens using the human as literal breeding vessels.
I could not help but think that neurotoxin drug treatments work like this: they are presented as something benign and “good”, but over the years they more often than not eat the person away from the inside, literally and metaphorically colonizing their mind and body. Their real aim is eventually revealed (to some who research outside the psychiatric narrative) as making profits for the drug companies and sustaining the status of the professionals. An important difference is that most psychiatric professionals are not really aware of the true long-term effects of the drugs in many cases; the cognitive dissonance would be too much. David, on the other hand, is quite aware of what he is doing, and thus is a chillingly evil and ruthless character.
Report comment
Bob, another thought I had:
It seems like the psychiatrists are unaware, or forget, that citing a single or even a few quasi-experimental studies about human subjects is not good evidence for anything. As you implied, what is needed is a range of many studies of different kinds that intersect to give the same message. There is a book I recently read, “Brain Storm: The Flaws in the Science of Sex Differences”, where author Rebecca Jordan-Young says,
“Unlike true experiments, where the controlled circumstances of the research can give strong evidence about cause and effect relationships from even a single study, quasi experiments become convincing only when multiple studies, related in specific ways, all point to the same conclusions. Neither individual studies nor even a small set of replications can ever be decisive. Nor can the results of even a vast number of quasi experiments simply be evaluated in an “additive” fashion. Rather, because all the studies are quasi experiments, the overall credibility of the theory depends on how well the studies fit together…. Because quasi experiments derive their strength from their relationships with other studies, a reasonable evaluation must consider all – and only – the studies that examine the same hypothesized (relationships).”
There are so many possible confounds to any single quasi-experimental study that one absolutely must have a range of related studies to say anything convincing. In this regard, it is revealing to see how the psychiatrists unscientifically cling to the Chinese study, as if they hoped to convince an ignorant public that one single quasi-experimental study is proof of anything. What is shocking is how little evidence they really have of any long-term benefits of antipsychotics. It truly is a house of cards.
Report comment
I also find the picture of the white psychiatrist in the lab coat at the top of article fascinating and disturbing. So evocative, saying so much with no words. The white male who defines pathology and wields the power to define others, pointing with his little Powerpoint stick at the version of “reality” that he projects onto the minds of the vulnerable and distressed, presumably…
Report comment
Simulacrum:- Deadly but completely true, Matt.
Report comment
Great article. If only there was an effective movement using direct action to make use of it.
Report comment
Robert Whitaker: –
Compelling, meticulous, intellectual analysis of the key literature.
Objective and effective.
Undertaken in order to disseminate accurate information which is of profound importance.
Powerful potential to alleviate suffering.
In stark contrast to –
Eight International “Experts in Antipsychotic Pharmacology, Neuro-imaging and Neuropathology”: –
Self-serving, selective misinterpretation and exploitation of the same literature in order to fastidiously construct disinformation.
This calculated deception is then spun to the legions of “lesser-psychiatrists” and primary care prescribers of antipsychotics who have a subservient and receptive mind-set, carefully crafted by the pharmaceutical marketing battalions.
The KOLs and their Marketeers then further disseminate these alternative facts, apparently with immunity from ever being called to account.
The press are briefed and are unquestioning, not even capable of addressing conflicts of interest.
Patients and their loved ones are subjected to further cruel deception.
Gift-wrapped false news which will add to their tardive dyskinesia, akathisia, multi-focal brain injury, metabolic syndrome, cardio-toxicity, endocrine impairment, antipsychotic induced pseudo-acne, and to their socio-economic, physical, psycho-social, emotional and personal devastation.
Occasionally, integrity and humility can be conveyed by a psychiatrist: –
“Amazingly, such is the power of the Kraepelinian model that some psychiatrists still refuse to accept the evidence and cling to the nihilistic belief that their exists an intrinsically progressive schizophrenic process, a view greatly to the detriment of their patients”.
“If I had the chance to have a second career I would try harder not to follow the fashion of the herd.
The mistakes I have made, at least those into which I have insight, have usually resulted from adhering excessively to the prevailing orthodoxy”.
Professor Sir Robin Murray: Mistakes I Have Made In My Research Career. Schizophrenia Bulletin. 2016.
This rarely seen, “honest psychiatry” appears to afford minimal, if any, motivation to produce copy amongst those journalists who disseminate the exponential propaganda and disinformation as “ground-breaking” revelation.
TRM 123. Retired Physician.
Report comment
In regards to your wish in the last paragraph. And thanks for the work – it saddens that it has come to this in our research world.
In my area,NAMI had implicit power to expose the medical school students and residents to carefully picked folks who would relate how the status quo of the system worked well for them. These folks were picked by staff who might not have had any professional training. At one meeting another woman and I were dismissed because of our expressed views that did not fit into the narrative. In our area, the journal news venue would come out with a reformed surivi or who had been a media flashpoint and now had seen the light and repented of their ways.
Many medical residents that see folks may not have received trading in the states. This creates a double edged sword hanging over patient’s head because they are dealing many times with medical folk who are only told the one narrative and may come with a cultural background that is patricharal and could be elitist.
Their ability to hear people’s suffering and trauma is diminished at times.
With the emphasis on medication so much is thrown effectively down the toilet in terms of any good that the profession achieved at times in the past.
The concept of true Auepiscaplian sp? is lost, torn asunder, and rent to the pyschiatrist’s very soul.
I admire the ones who hold on to the inherent moral practice of the Hippocratic oath. It still is not easy for them.
I would think drastic intervention is the only way to change the power dynamics-
Even if at times chemicals work for some the issue of where the MH world is belies a sense of things being on the right track.
Look at Polio-scabies these conditions showed drastic change not a slippery slope into hell.
Report comment
I agree with you about the fact that many of the psychology and psychiatry students are ONLY exposed to the medical model and are quite ignorant about the idea that patients could possibly do better without the meds. And yes, I think most of them either have no clue about the long term effects of the meds, or they wrongly assume that the patient would be even worse off without the meds.
Sadly, with some of them, they know and don’t care. My former psychologist knew I was experiencing akathisia and chose to say it was just another symptom of schizophrenia.
Report comment
Messed up Auespilican authority
The white coat effect. There was a great book in the past that had a great analysis of medical power in our society.
We give up power to docs but what happens when that contract is corrupted?
Report comment
Talking of white coats – is that the review author in the photo? Wearing a white coat to give a powerpoint presentation?
Report comment
No.
Report comment
Are you talking about Models of Madness, Models of Medicine, co-authored by Humphry Osmond nd Miriam Siegler? That’s the only volume I’ve read that discusses Aesculapian authority at any length (notice spelling, CatNight). I’d suspect these authors would treat Lieberman, et. al. as followers of a muddled model- moral overtones pretending to be medical (“behavioral diagnoses”, etc.).
Report comment
Not sure. Might have been if it was written awhile ago. I read while working in Social Services on a medical floor in a time where things were better than they are now.
Thanks for the correct spelling.
Report comment
A very interesting article. Is there any chance of getting anything corrected in the review?
Report comment
The arrogance of Lieberman & company is enough to make me pull my hair out! (And, as an EX-patient of psychiatry, I can do that and NOT get caged or raped with a needle!) Their latest self-regulatory PR stunt further solidifies the public’s negative perceptions of psychiatry, ALL of which are well-founded and GENUINELY researched. No other profession can LITERALLY shove its own version of its “success” down the throats of those people who, supposedly, “need” it. Of course, one reason they can do that is because psychiatry’s targets are, invariably, the “deplorables” of society. But, those people who aren’t “deplorables” can and do resent “professionals” who flaunt their offensive entitlement to “work” under the LOWEST possible bar of accountability. As a result, the majority of people STILL harbor a disrespect and distrust of psychiatry, despite its excellence at preserving their able-normative privilege. Call it “perp guilt” or “rage against the elites”, but mass “acceptance” of psychiatry IS NOT PROTECTING IT FROM ITS VICTIMS. The complicit public IS biting the hand that feeds it, in tiny, soft, steady nibbles.
Report comment
Nice deconstruction Bob – so scary to see this. You attribute the motivation more strongly to guild interests than Big Pharma interests – but have you considered both of these as expressions of political interests? Foucault’s “Society must be defended” lecture series and other works of that time argues that ever since Machiavelli societies have allowed or facilitated the slaughter (Foucault’s word) of some of its population in order to govern – usually by the withdrawal or supply of resources – allowing some to flourish and others to be left to wither. Following the apparent success of Pinel & Tuke (1800) asylum building took off with a flourish – and the medics got to be in charge, not because Pinel (a medic) was more successful than Tuke (a non-medic) but because the doctors convinced legislators they could detect dangerousness even when it was not obvious to the naked eye. Not only that, as Foucault also showed, Western societies have increasingly (since the 12th century) been governed (ordered) by keeping people in a constant state of self-observation and self-discipline, fabricating (Foucault’s term) the excessive individualism their economic systems were built upon. So DSM psychiatry facilitates this self-diagnosis/discipline (as the confession once did).
Seikkula is not only showing us how to respond to psychosis, but also to our collective madness. His thinking is closer to Tuke’s moral philosophy than Pinel’s medical engineering approach, as it stresses “being with” than “doing to”. This way of thinking is now finding expression in 4E cognition – the idea that “mind” is not in the head (noun-like), but embodied (verb-like) – and socially, group cognition precedes individual cognition (as Merleau-ponty saw – and Descartes didn’t). ‘We’ comes before ‘I’ – as most indigenous cultures recognise (e.g. ubuntu). Recognition of our humanity – our “we-ness” (as the Delphic Oracle suggested) leads to the kind of self-discipline we see in most pregnant women, who give up smoking and drinking with ease -(where care of self and care of other take in each other’s washing). In turn this leads to social ordering processes that are heart-felt and closer to James Cameron’s Na’vi, than the current panopticism does. Tuke comes closer to this ‘way of the heart’ due to the influence on him of Francis Hutcheson’s moral philosophy.
So from this perspective neo-kraepelinian psychiatry is a keystone to maintaining a particular political agenda that is now well-entrenched in Western cultures – one which will no doubt see such continuing rationalisations as Lieberman (its difficult not to make fun of that name) has provided here, reminding us of the rationalisations of the tobacco industry as the evidence mounted. I suspect that as the social implications of 4E cognition mount neo-kraepinianism may find itself in a similar position.
Report comment
Dr. LIE-berman. *not* *funny* Or true…. He *CAN’T* be true! He’s a LIEberman!
It would be like me changing my name to “Bill PsychDrugVictim Bradford”….
Report comment
Brilliant article which explains the corruption loud and clear while at the same time conveying the story of hope. Find any other way to get help except for psychiatry and your chances of leading a fulfilling life is vastly improved. What continues to amaze me is that story of hope is beaten down as a myth and the actual myth is seen as the truth.
I spent 10 years as a chronic ‘schizophrenic’ on the highest disability deemed incapable of functioning without help and support of the psychiatric system, and with their ‘treatment’ it was true. When I found my own way out and got off their drugs I was finally able to return as a whole person, functioning and contributing to society. Had I remained I would just be another person living an institutional life poisoned by drugs. The drugs totally and utterly incapacitated me and sadly I am not the only one.
Listen to the story of hope here and may those 8 psychiatrists one day bow their heads in shame for the destruction and misery they have caused. Shame on them. (And psychiatry in general)
Report comment
Hi Olga,
Your ‘mental health experience’ sounds very similar to mine.
Imagine if a person developing crisis was told “don’t worry we’re sure everything can be fixed up again” – instead of “unfortunately, your life is now over”.
Report comment
Hi Olga,
“….I spent 10 years as a chronic ‘schizophrenic’ on the highest disability ..”
Iatriogenic illness keeps the pharmaceutical companies going and this money gets passed around – but at a very high price to the public purse.
(I was also, NOT “safer” on medication).
Report comment
Olga you are a diamond in the rough my dear! you can consider yourself very lucky you managed to get away from psychiatry where im from in Australia if you end up the public mental health system with a diagnosis of schizophrenia its pretty much game over as far as the drugging gos with very little chance of ever having a drug free life if your caught out not taking your oral medication (drugs) then they just inject you with some anti-psychotic (drug). Like others out there i refer to this form of treatment as rather a form of NAZISM given what we know about these drugs now especially the long term outcomes you certainly would not give these drugs thinking it was in the best interest of the patient.. But im glad there will be survivors like yourself of this Holocaust that has hit mostly first world countries regarding the colossal damage that Psychiatry has caused over the last 40 years… Thanks for telling us your story and speaking out!
Report comment
Between 1933 and 1969, the number of admissions to psychiatric hospitals was greater than the number of discharges. Why then did the number of residents decline from 1955 onwards? Because the mortality rate was extremely high before 1969, and began to decline only from the 1970s.
And why was the mortality rate very high before the 1970s? Because the demographic composition of psychiatric hospitals was totally different. Until 1946, the majority of hospitalized patients were admitted for organic psychoses: syphilis, cerebral atherosclerosis, senile dementia… The antibiotics has destroyed syphilis, the improvement of food safety has removed the psychoses caused by malnutrition, the senile people are now supported outside of psychiatric hospitals.
Please, I need help to clarify these statistics, because I am not a specialist in documentary research. What is certain is that the decrease in the number of residents in psychiatric hospitals has absolutely nothing to do with the introduction of neuroleptics, but with a temporary increase in mortality, because until 1969 the number of admissions to psychiatric hospitals was greater than the number of discharges.
https://docs.google.com/spreadsheets/d/1fYCu3MUbfPEV1Zw0nNydLRAiyk1GVbcwRn2PxyzcKks/pubhtml?gid=2018955832&single=true
https://docs.google.com/spreadsheets/d/1M3FL2aCwpigOO2Uywo3zIkO4aGUn8d9DEwpXfYlQzXg/pubhtml
Report comment
Many assume that the advent of modern psychotropic medications was the catalyst for deinstitutionalization in the U.S. However, large numbers of patients began leaving state institutions only after new laws made unpaid patient labor illegal. In other words, when patients no longer worked for free, the economic viability of many state institutions ceased and this led to the closing of many state hospitals. MORE >> https://www.patdeegan.com/blog/posts/lead-shoes-and-institutional-peonage
Report comment
When prisoners no longer worked for free , you mean.
Report comment
Wow, I was not aware of this. I’m well-versed on prison-labor, which I consider the new slavery. Had no idea mental patients were used for free labor!
Report comment
Psychiatry is as prone to fads and crazes as the fashion industry. The neuroleptics are involved, in that they turned the “dangerous crazies” into passive robots (unless they stopped their neuroleptics). It was also cheaper to let the robots wander the streets than it was to keep them in the hospital.
Report comment
Hi Robert,
thank you for the thoughtful article. To me the most important part is your question at the end: where do we go from here? How do we break the juggernaut of Psychiatry and Big Pharma? But I think that question should also include: how do we change the public’s willing acceptance of the narrative, because, truly, the public, the majority of the families and SO’s of those who are in distress just want a pill they can give to their ‘loved’ one so that they don’t have to deal with unpleasantries. Certainly my wife’s family and mine couldn’t be bothered to help me and our son help my wife/his mother to heal. And most of those who visit my blog have VERY few people, if any, who are willing to do the hard work over an extended time, to be the healing partners these people need.
I’ve spent 7 years blogging about the phenomenal things an SO can do with someone who has d.i.d. So many of the guidelines ISSTD gives for these people, I’ve done the opposite and as a result she’s not even in the same universe as most others with d.i.d. when it comes to how far she has healed, and yet the tiny following I’ve attracted makes me wonder if people really would just rather give the ‘problem’ family member or spouse a pill so that their own lives won’t be disrupted, sigh…
Sam
Report comment
Sam, I’ve read your comments about your wife with fascination. There is a simple answer for why families aren’t willing to be the healers – they are most often the ones who have caused the mental pathology to begin with. The histories of family trauma can’t be ignored, much as the NAMI-Mommies demand absolution. I’m sure you’ve heard of the term “identified patient”. In such dysnfinctional families, there is no motivation for them to be the healers because the IP becomes the person they are free to blame for the family’s dynafunction. If I had to guess, I’d guess your wife was the IP in her family.
Report comment
Hi Kindredspirit,
I do understand that so many families are the perpetrators of the abuse themselves. Fortunately that was NOT the case with my wife’s family. Her parents’ problems were that they themselves had been abused as children and so they were in their own ‘funk’ while my wife was being repeatedly raped as a toddler: and they are still in that funk 50+ years later, sigh, all the while maintaining their ‘perfect Christian family’ display to those around them. It’s beyond my comprehension how that can happen, but I understand it did and still does…
My family? Well I think they’d just rather me get rid of my wife and move on like my older brother did with his second wife and then my mother had the nerve to ‘defend’ his action to me in light of my unwillingness to do the same to my wife…My family is the good conservative family who believes everyone should pull themselves up by their OWN bootstraps…sigh…(took me awhile to unlearn that one…)
I know there are a myriad of reasons why people are unwilling to help, and so even though I highly respect Bob, I think he’s wrong to think that the majority of people will ‘see the light’ once we destroy the biomedical narrative. I still support and applaud his work and others as a key part of this fight, but I think we need something more to take on this Goliath…and even then the history of how cultures take care of their problem members makes me think many people will just find another way to blame and remove the victims rather than taking responsibility for helping them heal…
Report comment
Thank you for your community service; your work has insured you a prestigious place in history!
However, I respectfully disagree with one premise. In 1980, psychiatry abandoned Freudian Theory and lumped neuroses (problems with living) together with their established “diseases” (psychoses); thus, psychiatry “doubled-down” on the “disease model” rather than “adopted” it. Addressing neuroses (social welfare problems) hurt psychiatry’s legitimacy as a medical science so they redefined them as psychoses- medical problems (and abandoned Freudian Theory). Psychiatry has always been based on the “disease model” since it considers itself a medical science.
Your recommendation is a good one; challenge medical students on the legitimacy of their science (or their field). I advocate that mental distress is a social welfare problem and that “First, do no harm” is impossible when believing that natural human suffering from traumatic injustices (or physical problems) is a disease.
Thank you for allowing me to comment on your article and your work in challenging the harm of long-term drug “therapy.”
Best wishes, Steve Spiegel
Report comment
Steve,
I think the power structure at the top needs to be challenged. It’s like groups of individuals are treating publicly funded organisations as their own property.
I think now is the time to challenge this abuse – because parts of Normal Medical Practice have crossed the line into criminality.
For Example:- I’ve attended two top UK Eye Research Hospitals with a serious eye condition; and when I’ve mentioned the historical ‘effects’ of psychotropic use on my eyesight – negative mental health comments have been entered into my notes instead of my own version of my own experience. All the doctors (as far as I could see) were under this influence.
Another example of power abuse would the promoted use of statins and the manipulation of heart disease risk in terms of (isolated) cholesterol. There are lots of similar examples….
I think the individual doctors have been weakened and need to keep their heads down to survive. So they’ve become enured to a culture of exploitation and power abuse.
Report comment
hi Steve,
here’s the simple version of what you said: treating non-medical conditions medically.
what’s the true cause?
humanity’s lust for knowledge. however, people perverted knowledge when they chose the atheistic, amoral path totally abandoning our true nature which is spiritual.
remember, psyche by definition means spirit.
Report comment
Thanks for all the comments. A few notes:
Matt, I had thought about making a photo of Jeffrey Lieberman the featured image, but then I found this one, of a psychiatrist in a white coat presenting a power point, as representative of the power dynamic in society, just as several of you have noted. This exemplifies the source of the information.
Sylvain, your point about the makeup of patients in state hospitals prior to the 1950s is extremely important–a high percentage had known physical diseases. Syphilis, dementia, malnutrition, and lead poisoning, for instance. (David Healy has a fascinating presentation on how certain types of “madness” disappeared in lockstep with society converting to lead-free gasoline.) The mental hospitals were serving, in large part, as nursing homes for such patients, until they died. The reason for the patient population starting to decline after 1955 was really social policy. The states set this up a goal, particularly with first-episode patients. And then the real emptying of the mental hospitals began after Medicare is set up, and states could discharge their “chronic” patients to nursing homes, group homes, etc., and have the federal government pick up the cost. So the locus of “institutionalizing” such patients changed from the mental hospital to community sites, or other types of institutions. You’re right that this change in patient census has little to do with the introduction of neuroleptics.
Samruck, this is the ultimate question: how do we change the public’s willing acceptance of psychiatry’s disease model narrative. It is a narrative that many in society are eager to adopt and accept . . . it fits the magic-bullet belief. And all I can say is that if people in the public can learn about the critique there is to be made about psychiatry, and how the conventional narrative is better described as a marketing story than a scientific one, then there is the hope of changing that narrative. When people learn about the collapse of the chemical imbalance story they often stop and think, what? Then why were we told this.
Steve, regarding psychiatry “”adopting” the disease model with the publication of DSM–III, or “doubling-down” on it, I get your point.. But with Freudian theory, there was also the thought that some psychoses fit into the framework of a failure to adjust, as opposed to being a pathology. So there was a disease model element in DSM I and DSM II, but it mixed with the Freudian model too.
I appreciate all the comments.
Report comment
Being cynical, but I don’t believe many family members or SO’s really want to know the truth. There may be some who will welcome the truth, but I believe that many people want their own lives and don’t want to worry about doing the very hard work necessary to help a spouse or family member heal. Our culture’s distaste for emotionally ‘needy’ people is one factor. But, the biomedical model also relieves neglectful or outright abusive families of their responsibilities for contributing to a person’s issues, and if a trauma model was generally adopted suddenly there becomes the issue of culpability that the biomedical model neatly attributes to one’s genes.
I love my wife, but dealing with her issues cost us our entire marriage so far, her entire life, and our son’s entire life. At least we finally understand what was happening and now I know how to help her heal, but I simply don’t believe most are willing to do what it costs to help someone heal. I’m not saying that because I think I’m so wonderful and others aren’t, it’s just because I understand the terrible price my wife, son and I have paid trying to undo what was done to her by abuse and neglect of those in her childhood, sigh…
Report comment
Hi Bob,
I hope that you will submit this well written rebuttal to the American Journal of Psychiatry. and maybe to Columbia and the NYT!
thanks for taking the time to provide us with this analysis!
yana
Report comment
I agree. Perhaps they will feel compelled to publish it, as it is a direct response to the article they wrote. Perhaps you can even get other dissident MHPs to sign on to the article?
Fantastic piece of analysis!
Report comment
I’m thankful for the medicine because I think being out of touch with reality and having difficulty performing life tasks is grounds for an illness. Although this is the case I too have a scientific point to address. I formulated this sitting on my back deck late at night having a cup of tea listening to Sam Prekop’s self titled album.
There is one area where the psychiatric profession is near to the point with term schizophrenia.This actually is when someone has an illness that has the strong biological component of the central nervous system as root cause. They then prescribe a psychotropic and the direct result is an alleviation of symptoms because these medicines change behavior of the neurotransmitters.
There are actually three causes of schizophrenia that I have deciphered and there are likely more as schizophrenia is apparently an illness of unknown origin. I’ve mentioned one in the above paragraph. The additional two are hormone regulation and functioning of the endocrine bodily system and an environmental cause such as a history of trauma.
The illusion of the medical profession is that they can treat all cases of schizophrenia with a psychotropic. Knowing that a psychotropic alters the function of neurotransmitters it would hold true that they would only alleviate pain if the schizophrenia was caused by the central nervous system.
If schizophrenia was caused by hormones or a broad range of environmental factors psychotropic wouldn’t assist but would actually make recovery more difficult. You’d also be introducing a new biological component to the body which could even look like an illness, but in theory it would be the pharmaceuticals. This is particularly troublesome for someone that had an onset of symptoms due to an unknown environmental cause.
Report comment
only thing the analysis of reports does is make it look like researchers break the infamous neremberg code because the analysis flat out say the studies lied. Also because it passes our borders into international boundaries.
The medicine alleviates pain for a lot of people so will not appear that ethical laws are in judgement. This wont stand from rebuking studies. It will change minds of a lot people though.
It was interesting to see how latest world health organization statement on depression a few months ago. I think the same statement could be said for schizophrenia too. Victories like that go a long way and are good to see.
Report comment
Whiskey, cocaine and meth also relieve people’s pain. That still doesn’t make them medicine or safe and effective. A lot of psych drugs are more addictive than what you get off the street.
Shrinks don’t like drug abuse or “self medicating.” How can they possibly bill medicaid, after all?
Report comment
It doesn’t follow that if drugs appear to help someone, it means there is something wrong with them. I appreciate the rest of what you said, though. I think the big, BIG problem with schizophrenia is that it’s just a description of some things that happen for reasons unknown. If they were really honest, they’d admit that psychosis was a phenomenon that could be caused by many things and would look at each case and look for subgroups of people who may have similar experiences or physiological findings. But they don’t. Because they WANT their “biological dysfunction” story to be true because it brings them money and professional power and status. That’s pretty much the definition of corruption.
Report comment
What about Wunderink? Does lieberman approach the Wunderink study?
Report comment
Thanks so much for this article Bob! One small detail I can’t help but add:
Apparently the “tardive dyskinesia market” is heating up, according to Pharma sources. A company called Neurocrine Biosciences has brought out Ingrezza (valbenazine), a drug to treat a disease known to be a direct side effect of antipsychotic drugs. A side effect we were told was a remnant of the bad old days, since the new “atypical” antipsychotics allegedly did not cause it.
Neurocrine will be charging $63K a year for Ingrezza. The competition, a Teva drug called Austedo, currently used only for Huntington’s disease but aiming for “TD” approval, costs $60K for now.
http://www.fiercepharma.com/marketing/neurocrine-goes-high-60k-plus-high-price-for-new-movement-drug-ingrezza
You can lie to the patients .. the doctors in the field .. the general public. But you can’t lie to the investors, I guess. That would be a sin.
Report comment
It sounds like a type of wishful taxpayer funded money launder attempt.
Report comment
Ingreeza is being heavily marketed right now.
Report comment
*correction: “Ingrezza”….
imagine, $60K+/year, to ‘treat” the EFFECTS of a DRUG that usually wasn’t necessary, – at least long-term, – in the first place. NOBODY on disability can pay for that! So *WHO* gets stuck with the bill for this “Ingrezza”?…. The Taxpayers?….
PhRMA is even marketing a drug for “OIC” – Opioid-Induced Constipation!….
I’m literally AFRAID, both where all this is going, and where it will end!….
The system is literally MORE INSANE than the people in it!
Report comment
It’s not just the system. The American public is indoctrinated to take pills for absolutely everything. Remember the last statement in drug commercials on television; “Ask your doctor….” Look into the typical American’s bathroom medicine cabinet and see what you find. When we experience the least little problem with anything to the medicine cabinet we run. We need to educate people to be more discriminating about what they accept as gospel truth about all this. It’s a fact that more GP’s are writing scripts for psych drugs than psychiatrists themselves. We have let this run amok and the system takes advantage of it.
Report comment
Hey Stephen, totally agreed. I boggle at the fact that the pharmacy section of my local grocery store is larger than the produce section. Americans are hooked on pills.
Report comment
valbenazine – must be close to tetrabenazine, used for decades for TD (and not terribly effective and many s/e’s of course) – interested in comments on this, thanks
Report comment
I know it’s late, but I’d better mention a paper of Richard Kunin’s a San Francisco MD), who wrote a Journal of Orthomolecular Psychiatry article about treating TD successfully with manganese salts and/or B3 around 30 years ago. This, no doubt, brought terror into the hearts of the orthodox, discussing not only drugless treatments, but also that dreaded word, “niacin”, as a component of such treatments. Kunin is apparently still alive, because he has a web site in which he promotes nutritional treatments of “mental” ailments, which I’m sure no psychiatrist in his right mind would dare scan.
Report comment
It is related to tetragbenazine. The medical center here was doing a trial of another related compound.mthere was a “tweak” to the molecule which they claimed reduced side effects but that one is not yet on the market.
Report comment
CORRUPTION.
In 1980, in my original UK Maudsley/Kings College Hospital notes:- there is no mention of Amsterdam where I had spent the previous months; no doctor takes any real responsibility for suggestions or descriptions made; and details of my personal history are significantly inaccurate.
Two months later when I was transferred door to door to hospital in Western Ireland there were two admitting doctors one young Irish doctor and one young Non European doctor. Me and the accompanying English doctor were interviewed seperately.
The non European doctor describes me (in his notes) in terms of wellness – and the young Irish doctor ‘disappears’. The young Irish doctors notes (with brief reference to Amsterdam) are updated to several days later and copied in by the Consultant Psychiatrist (in his own hand).
I was in hospital in Ireland for two months but I never fully recovered from the heavy duty drug battering of that period.
In 1980 in Amsterdam I had stayed at the same address as a Northern Irishman by the name of Kevin McGrady who impressed me as being a genuine reborn again Christian:-
https://en.m.wikipedia.org/wiki/Kevin_McGrady
I think it’s possible Kevin McGrady was being “groomed” as early as 1980; and that there was interference to the “overall process”.
Report comment
Lieberman says critics of the drugs “create mischief for their own nefarious purposes.”
Really dude my own “nefarious purposes” ?
Nefarious, wicked, evil, sinful, iniquitous, egregious, heinous, atrocious, vile, foul, abominable, odious, depraved, monstrous, fiendish, diabolical, unspeakable, despicable…
All words that describe what you people did the Zyprexa scandal damn drug almost killed me you nefarious criminals called safe and effective and even pushed it on children wile knowing all along it was poison.
What a bunch of complete psychopaths that can never own up to anything. You people are worse then the NAZI war criminals who at least somewhat owned up and tried the “just following orders” defense.
Why don’t you address the countless major crimes by your industry before you even start playing all the games with the numbers graphs and statistics ?
“a small price to pay for the molecule.”
“torture the data”
http://web.archive.org/web/20120122013020/http://www.furiousseasons.com/zyprexa%20documents/ZY100378062.pdf
Report comment
Cat,
The killings are a Holocaust, and the perpetrators are psychopaths.
Report comment
…..note the Psychopathic tolerance towards loss of life.
Report comment
Gotta love when someone tells it like it is without holding back. The drugs are poisons. They are not medicines and I refuse to tiptoe around the fact that they are poisons by calling them neurotoxins. The fact that some of these drugs were discovered in the process of developing pesticides makes it clear they are poison. And you’re right, these perpetrators are criminal.
Report comment
Great response! By the way, the Leucht 2009 review is even worse than you suggest, because it includes all the studies of atypicals that you rightly criticised in Mad in America. Lots of these studies were done with chronically hospitalised patients who were already taking long-term antipsychotics, and were then randomised to take a second generation antipsychotic or discontinue altogether (most likely abruptly). Given this, the difference in ‘response’ rates between the drug and placebo (17%) is very disappointing!
Report comment
Randal,
They do discuss the Wunderink study, in a section on tapering/discontinuation. They discuss it regarding whether there is a subset of people who can do okay when tapered down to a low dose/no dose, and incorporate the Wunderink study into a conclusion that: A subgroup of patients, which may be as large as 20%, may maintain remission or partial remission for extended periods off medication.
So they are not presenting it as a referendum on the long-term merits of antipsychotics in general, but whether a percentage of patients can get down to a low dose. While there is a tone in Lieberman’s article of dismissing this as significant, they present this data correctly.
However, in terms of looking at Wunderink as providing information regarding the long-term effects of antipsychotics, you need to analyze the study in a different way, which I did in The Case against Antipsychotics, and thus, since they cited that article as raising concerns about the long-term merits of antipsychotics, they were aware of.
The group randomized to the tapering arm, were more likely to be off the drugs long-term, or down to a very low dose. But after that initial tapering moment, it became a naturalistic study, with people in the drug-maintained group free to go off. And so what you want to do is analyze long-term outcomes for all patients according to medication usage, and if you do that, you find that the low-dose, off medication had much better outcomes on all domains that were measured.
When analyzed in that way, as a naturalistic study following an initial moment of tapering, it provides yet another longitudinal finding that tells of medicated patients doing worse than those off antipsychotics (or down to a very low dose.) But LIeberman and colleagues don’t mention that data at all, and so once again, they avoiding presenting longitudinal data that supports the conclusion that antipsychotics worsen long-term outcomes.
I chose not to discuss this in this article just for space purposes, as the article was already so long, and this one needed extra space to show why they treated Wunderink in the way they did.
Report comment
Hi Bob,
This is an excellent review. Thank you.
I think a response to what you write above is that the decision to taper was influenced by clinical factors. So those who got to be on low or no dose could have gotten there because of some characteristic in their presentation that was independent of drug effect. This is the argument often raised about Harrow although, as you point out, the group who was never on drug was still having a high degree of psychotic symptoms at 2.5 years and the improvement observed was captured at four years and later.
I will write more later but I continue to think there is a conundrum about how best to respond to psychosis in the short run when it leads to behaviors that puts a person in harm’s way. I hope to write more but I have come to wonder if there is something in addition to guild pressure and Pharma influence – something inherent in the nature of clinical decision making – that creates a cognitive distortion for the physician. Relapse risk looms larger than more distant, less quantifiable risks. I am influenced by the writing of Daniel Kahnemann and hope to flesh these ideas out more. This comes from reading his work, thinking about my own experiences in trying to taper, and working/supervising other doctors for many years. Just as your intent is far from nefarious, these cognitive biases are not always nefarious but a reflection of the limits of cognition when faced with uncertainty. All of these statistics – which I suspect I will be debating for the duration of my career – will never resolve with certainty the question of what is best for the individual.
Report comment
The introduction of medicine into the hospital is relatively recent: mid-19th century. Previously, hospitals served as an asylum for the poor, the aged and the disabled, who were often locked up by force. Then the hospital was divided into several institutions: retirement home, sanatorium, establishment for mentally deficients, etc. Most of these institutions have retained their function of social control for old people, mad people and homeless people.
Psychiatry can not be scientific, because its function is not medical, but social. Capitalist society permanently created deviants that it can not integrate, these deviants (old people, homeless, disabled, mentally retarded, delinquents, etc.) are then locked up in institutions or sedated until their death.
If you do not understand this, you can not understand why psychiatry also grossly refuses the scientific method and the medical ethic.
Capitalism proceeds from the destruction of the community, the development of institutions, the division of labor and the atomization. “What is good for individuals” is the restoration of the community, such as Soteria or Pavilion 21. But the community is precisely the opposite of the institution. This is why “reforming the institution” has no meaning: the development of truly human relationships necessary for the disappearance of psychosis inevitably leads to the suppression of institutions.
Report comment
Sandra,
I know you are ‘one of the good guys/gals’ but power corrupts; absolute power corrupts absolutely. Whether it’s ‘nefarious’ or guild pressures, or whatever, is kind of irrelevant except in a theoretical sense, though I do appreciate your attempt at fair play. Even if psychology/psychiatry had anything to offer as I help my wife heal, I will NEVER let her close enough to find out because of the absolute power they wield (edit: though I do use their attachment theory and some other concepts in ways they can’t/won’t). I’m doing well enough, heck, way better than the experts from ISSTD ever claim to do with their patients, and so I will never let the woman I love be potentially subjected to the horrors I regularly read on wordpress where I blog and elsewhere, even if it literally kills me from the stress as I try to help her heal…
Respectfully,
Sam
Report comment
Sandra,
I was diagnosed as a terrible case in 1980/81 with guarded prognosis in Ireland, due to a fairly obviously inaccurate account of me coming from England.
In the next few years I had suicidal hospitalization after suicidal hospitalization culminating in 1984 when I was judged to be absolutely hopeless.
Then I came off the drugs very carefully, engaged in community psychotherapy and have remained well since.
When I was leaving Ireland in 1986 I collected some references from people that had known me over the years. In contradiction to my psychiatric records these references were very positive.
Report comment
Hi Sandra, You write, “I have come to wonder if there is something in addition to guild pressure and Pharma influence – something inherent in the nature of clinical decision making – that creates a cognitive distortion for the physician.” I wonder what the relevance this would have. Since guild and pharma influences are so powerful and virtually ubiquitous (albeit not necessarily consciously experienced), when would this putative clinical factor even come into play? The former two influences coopted many idealistic therapists–products of the countercultural 60s– during the threshold of development of psych-pharmaceutical complex in late 1970s and 80s. (Bonnie Burstow discusses the transformation of the few idealistic young professionals into drug pushing social control agents–and their eventual apostacy.)
On the other hand it does not seem as if the clinical factor you hypothesize adversely influenced many of those who worked at programs such as Open Dialogue or Soteria–they resisted whatever impulse they may have felt to resort to encouraging neuroleptics.
Seth
Report comment
I am thinking about this idea and may write more. Of course, this is just a hypothesis based on my reading of Daniel Kahnemann and my self reflection as I have tried to shift my own practice. I also do not think one can ever tease apart the multiple factors that influence clinical decision making.
Kahnemann studied how people make decisions and calculate risk in the midst of uncertainty. Each of us every day has to make decisions based on an intuitive sense of the odds of having one outcome vs. another. In his work, he (and many others – his worked led to the development of the field of behavioral economics) realized that people make decisions that do not follow the actual odds. For instance, this plays out in the decision to buy insurance which most of us do even though it might not be the best decision from a purely economic perspective.
I have reflected on my own experiences in working with people to taper off drugs or to avoid using them in the first place. You and I probably have some fundamental disagreements but at least from my perspective, I notice that the risk of a person returning to what I am going to call “psychosis” with the risks that can entail, feels worse that the risks associated with maintaining the drug. This feeling state remains even though I essentially agree with people like Robert Whitaker and Joanna Moncrieff, I am not a member of the APA, I am pretty disgusted with the commercial influences on medicine and psychiatry.
I bring this up because for those of us who are in the reformer camp as opposed to the abolitionist camp with regard to psychiatry, might find value in thinking about why it is hard to have people change practice. I suspect this kind of thing might have played a role in the evolution of those idealistic professionals to whom you refer. It also might play a role in why psychiatrists who are sympathetic to the clinical practice of Open Dialogue might not fully adopt its prescribing practices. This seems like an important thing for us to understand since the use of drugs may play a very important role in the reported outcome of OD.
Report comment
That is a very interesting point about possible cognitive distortions in physician’s decision-making. I would suggest it’s not just confined to psychiatry. I suspect that I have encountered this in various medical fields, in all major aspects of my medical care. This has convinced me that patients need to be fully informed and need to have as much of a say as possible in decision-making, since patients will be looking through a different lens than doctors and will probably not hold quite the same biases.
Report comment
I join in the plaudits. Something I react to whenever I read something like this however:
we focused on its institutional behavior since 1980, when the American Psychiatric Association published the third edition of its Diagnostic and Statistical Manual. This was when the APA adopted its disease model for categorizing mental disorders, with the profession then taking up the task of selling this new model to the public. This was the particular guild interest that arose in 1980, and has shaped its behavior ever since.
This gives the impression that before 1980 psychiatry did not have a “disease model,” when the very existence of psychiatry as a supposed branch of medicine is predicated on the assumption that there are “mental diseases.” WAY before 1980 I was woken up every morning on the psych ward to the cry of “MEDICATIONS!” — and they weren’t for heartburn.
All these DSM’s have ever done is play around with labels; psychiatry has purported to treat diseases since its inception.
Report comment
I agree Oldhead.
AND Psychiatry has always had “guild interests” to protect and extend its influence as a medical specialty; based both on faulty science and invented concepts of “mental illness.”
The major collusion between Psychiatry and Big Pharma that began in the late 1970’s was the advent of Biological Psychiatry; representing the very worst of psychiatry now on high doses of its own steroids. AND all this now riding a tidal wave of the pharmaceutical industry’s rapid expansion and innate drive for profit – by any means necessary.
Four decades of perhaps the largest multi-billion dollar PR campaign and medical hoax ever perpetrated in human history, and here we are today. This extremely powerful institution of Psychiatry is now so deeply embedded in the social fabric of our society that it has become both a NECESSARY AND ESSENTIAL INSTRUMENT OF SOCIAL CONTROL preserving the continued existence of the U.S. empire.
Richard
Report comment
Thanks, Richard! In Feb. 2016, the local hospital, “Cheshire Medical Center/Dartmouth Hitchcock-Keene” (CMC/DHK), fired Dr. Marcia Pabo, a psychiatrist, which resulted in them closing their 6-bed adolescent psych unit. A few months later, they fired 30+ staff, and closed the 12-bed adult psych unit. This was around the time they spent $1.5Million re-doing their ER to install several new “psych holding cells”. In 2016/2017, Dartmouth-Hitchcock got the contract to provide psychiatrists to the State mental hospital. They have so far failed to provide full psych staff levels as mandated by that contract, but the State is amazingly lenient. Psychiatry is on the ropes here in New Hampshire. The local private drug treatment detox has to rely on a single psychiatrist, who’s over 80, to sign off on their billing. The local CMHC does not seem to use the very word “psychiatry”….
We ALL here at MiA need to KEEP UP THE GOOD WORK! Psychiatry is a pseudoscience, a drug racket, and a means of social control. It’s 21st Century Phrenology, with neuro-toxins. The DSM is a catalog of billing codes. ALL of the bogus “diseases” in it were INVENTED, not “discovered”. Repetition is reinforcement. Repeat the TRUTH after me, “Psychiatry is a pseudoscience, a drug racket, a means of social control….”….
So-called “mental illnesses” are exactly as real as presents from Santa Claus….
Report comment
The major collusion between Psychiatry and Big Pharma that began in the late 1970’s was the advent of Biological Psychiatry
Thorazine was created in or around 1950. There was no qualitative difference between psychiatry in the late 60’s and the late 90’s that would justify giving the latter a different name. “Biological psychiatry” is just more of the same. And using the term as though it means any more than it does could lead some to believe that we don’t need to eliminate ALL psychiatry, just the “biological” kind.
Report comment
Oldhead,
I think the difference is — Richard conveys it aptly–is that in the 1980s the drug industry rather than the guild became the dominant influence. But the guild influence was always there and it requires using pseudo-medical treatments on “psychotics.”
Remember in 19th century psychiatrists were managers and custodians of lunatic asylums. In order to win out over lay competition they had to appear as much like doctors as possible. In 19th century medical treatment entailed attacks on the body, whereas in 20th–as Breggin noted–it entailed direct assaults on the brain of “psychotics.”
There were major differences after big pharm took over–you could say they were merely “quantitative” but that doesn’t make them less radical. The number of people subjected to Psychiatry is vast today as compared to the 1950s, as Bob documented in AE.
Guild interests required shrinks pose as doctors from the start, and their attitude towards psychotics has always been disdainful and punitive–their “treatments” have always been destructive. But their influence was relatively limited. Now their influence on society is extensive and ever-increasing.
sf
Report comment
Thank you, Mr. Whitaker, for this extremely thorough rebuttal of Lieberman, et al’s published paper. This is why I continue to return to this site.
Research I’d really love to see would be the effect of antipsychotic treatment on those with so-called bipolar disorder. Since an author on MIA recently touted the disproven notion that SSRI-induced mania is indicative of bipolar – an idea that is widespread but even the DSM5 disputes, it’d be interestinf to see what the effects of long-term antipsychotic treatment is on those who never were psychotic to begin with – those of us given antipsychotics as “mood stabilizers”. I’d appreciate being pointed to any such research that already exists. Since in my own case, the only psychotic symptom I’ve ever had began when I stopped treatment, I’m very interested in seeing long-term outcome studies of those with bipolar.
I’ve been doing some medical sleuthing on myself trying to figure out how I ended up in this situation – and with a child diagnosed with RAD – because of the articles I’ve read here describing the treatment of the autistic community and the symptoms described by some authors that are surprisingly similar to mine. I also learned that autism is a differential diagnosis for RAD and that my child had never been tested for autism. So I had my genome sequenced and found that while I do have a few (four) snp’s that supposedly code for bipolar, I have dozens of gene variants that code for and indicate an increased likelihood to develop autism. Additionally, my nephew has autism. Since the RAD diagnosis exists almost solely in the adopted community, I believe autism/PDD would have been my daughter’s diagnosis had she not been adopted. So that’s a long way of saying I’m curious what the effect of antipsychotic drugs is on autistic folks.
Thanks again, articles like this keep me going on the days when it seems establishment psychiatry is winning the propaganda war.
Report comment
Dear fellow nefarious critics of psychiatric drugs,
These eight psychiatrists must feel threatened and fear their status and prestige is crumbling, to go to all that trouble of trying to discredit their critics. It also shows that those critics have reached a critical mass that cannot be ignored or dismissed as inconsequential.
I do not believe that we should waste too much energy trying to convince people to change their beliefs when they do not have the capacity for change. They are too rooted in dogma and motivated by their own financial survival and status.
I believe Mad in America’s greater gift is to offer an organization and support to those that instinctively know, without the benefit of a scientific study, that they would be better off without medication and those that want to help them. That awareness takes an evolution and strength that some may never achieve. Yet, Mad in America is providing that community and environment that is helping more and more people come to that knowledge by themselves. I applaud MIA and everyone involved for their courage and dedication to helping others at their own financial sacrifice.
Are there MIA buttons? I would like to wear one and would delight in seeing Jeffrey Lieberman’s reaction in spotting it. We should celebrate the birthday of Mad in America. As the years have progressed, we see the growth of this organization in members and strength. So thanks Lieberman, for highlighting to your peers how strong your critics’ voices have become. And thank you again Robert Whitaker for providing a gathering place for those critics. Be persistent and consistent and eventually we will be heard.
Report comment
Kindred Spirit, you bring up a really important point.. There are no studies that I know of on the long-term effects of antipsychotics when they are used for other purposes, bipolar, autism, and so forth. They get tested in the most haphazard way, over the short term and often as an “adjunct” therapy, and even in the short term adjunct trials, they don’t provide much of a “benefit” in terms of symptomatology. If I remember correctly, when they tested one of the atypicals for “autism,” they concluded it doesn’t cause much akathisia in this youth, although there was a note that the autistic youth had to “self-report” they were feeling anxious, rather than have doctors look for it. But really, all this use of antipsychotics for other purposes is really just the result of a marketing campaign, and made possible because antidepressants may not really work for many people, the “mood stabilizing” agents for bipolar aren’t effective for so many, and so forth.
I hae a hard time imagining that long-term use of antipsychotics is good for youth diagnosed with autism. But it’s easy for me to imagine that it does a great deal of harm for youth so diagnosed and so treated.
Report comment
I could not find the study Nancy Sohler et al. Am J Orthopsychiatry. 2016; 86(5): 477–485. Weighing the Evidence for Harm from Long-term Treatment with Antipsychotic Medications, A Systematic Review.
This study shows that “Psychiatry’s Evidence Base For Antipsychotics Comes Crashing to the Ground”: https://www.madinamerica.com/2015/12/timberrr-psychiatrys-evidence-base-for-antipsychotics-comes-crashing-to-the-ground/
Other studies e. g. “Antipsychotic treatment: experiences of fully recovered service users
Jone Bjornestad, Larry Davidson, Inge Joa, Tor Ketil Larsen, Wenche ten Velden Hegelstad, Johannes Langeveld, Marius Veseth, Ingrid Melle, Jan Olav Johannessen & Kolbjorn Bronnick
Journal of Mental Health”
http://www.tandfonline.com/doi/abs/10.1080/09638237.2017.1294735
use these results: «Due to the lacking long-term evidence base (Sohler et al., 2016)…»
Report comment
I feel it goes way deeper than guild interest though of course an institutional sense of self-belief in role that attracts status, privilege and power is a heavy bias – but can those at the top be unaware of the nature of their choices? I think not – but they may operate from a sense of self and world that effectively ‘captures’ their mind just as they seek, and to a large extent succeed, in capturing and directing the narrative of acceptable or official or mainstream belief.
For what I see is capture or usurpation of regulatory bodies, educational and media – indeed the financial system itself is a form of capture within a debt inducing system of control that links with corporate cartels that plunder wealth and resources for gratifications that evaporate while power for its own sake operates destruction and degradation.
Whether true or not there is a belief in many that eugenics never went away and population control operates under the mask of trojan beliefs that cannot be challenged without penalty. Indeed many cannot even think on or consider such ‘no go’ areas by induced self-censorship or simply recoil from a sense of horror – for if you don’t ‘go there’ you can carry on as if you don’t know and are not complicit or subject to what is essentially a kind of mind-control operating through or upon our unconscious psychic emotional conditionings.
The idea that the system or society is insane and so will treat non conformity as insanity – (which is now equated with physical disease) – like a heresy under the rule of dogma – for science has been no less captured in the patterning of a ruse it did not disclose or illuminate – but has managed to hide even more deeply.
This patterning is not unknown to us but calling it ‘psychology’ frames it in dissociations and rationalisations of ‘define and control’ that suits a ‘pharmaceutical management’ of life-defined-as-sickness – whereas calling it psychic-emotional conflict and fragmentation suggests more relational participance and therefore potential for awakening responsibility. This is a challenge for growth and not just a quick way to feel more secure – that can capture in addiction and consolidate patterns of belief that make it more difficult to challenge or be curious in relation to the issues that are underlying the difficulty.
The core ‘define and control’ facet of narrative control that is part of every personality structure is our largely unconscious acquired beliefs that are the embodiment of conditioning or past experience. These are often held in society to be fixed conditions – in other words ‘Reality’; the world, and the way things work.
There is always another way of looking at whatever is felt dissonant and the willingness to let this in, is a significant step.
Report comment
I am deeply indebted to you for opening my eyes to the medical disaster that is psychiatry.
I have made Mad in America required reading for the MA-level course I teach, Social Dimensions of Psychotherapy, and I have requested that our graduate school invite you to speak at our 40th anniversary celebration in 2018.
You ask the most important question at the end of this article. I believe that psychiatry has gained so much power that it will take a massive social rebellion, even greater than the one that challenged it in the 1960s-70s, to uproot it. I believe that the groundwork for that rebellion is being laid today and that you are an important part of that process.
I thank you from the bottom of my heart for your courage and integrity in showing us what needs to change and for launching the frame of an organization (this website) that can take us forward.
Report comment
Go, Susan! Where do you teach?
Report comment
I teach at Adler Graduate Professional Schools in Toronto – http://www.adler.ca/
Report comment
Thanks, Susan. I want to say that I was a guinea pig for “residents” at McLean. They were kids and they got to toss me around like a plaything for a few years. Well, now they are grown up, mostly rich I suppose. I should have been paid handsomely for being their stepping stone.
All the while I kept a journal. Those residents scoffed at me as if my writing were child’s play.
Dear Residents, Here’s what Anne Lamott has to say, “You own everything that happened to you. Tell your stories. If people wanted you to write warmly about them, they should have behaved better.” –from Bird by Bird: Some Instructions on Writing and Life
Report comment
And Susan has written some great books, too, very concise and accessible.
Report comment
“I believe that psychiatry has gained so much power that it will take a massive social rebellion, even greater than the one that challenged it in the 1960s-70s, to uproot it.”
not a chance. not even slightly.
the mass public are absolutely useless.
Report comment
agree with you
Report comment
Susan,
Just to say, that it is great you are teaching your students this “counter-narrative, and also to say that to change the hold that “biological psychiatry” has on our society is to change society, and as you say, that is going to take a grass roots rebellion.
Report comment
Thanks for the new essay Bob. I did not read all of the responses so i hope this is not redundant.I feel compelled to address a controversial issue- I brought up in response to other critics of the dominant paradigm–to Jonanna Moncrieff and Dr Larrsen-Barr. In your response to Allen Frances you wrote, “I think science is telling us that antipsychotics, on the whole, worsen long-term outcomes, even when prescribed for ‘clear cut psychiatric disorders,’ and thus, if psychiatry wants to develop evidence-based protocols, it needs to figure out how to minimize their long-term use. ”
Some of the dissidents have been seduced by the prospect of “a middle way”–as if it is Buddhistic. You described the mildly dissident Frances ‘credo, “Prescribe them to the right patients, because for these patients the drugs can be life-saving, but curb the overuse and polypharmacy that can prove harmful to so many, particularly for those who have ordinary problems, as opposed to real psychiatric disorders. As you can see in his blog, he also sees this middle way as informed by his own clinical experience.”
And you continue” But, here’s the rub: the “middle way” he describes is not an evidence-based practice. It is not a practice that is informed by science that tells of drugs that induce a dopamine supersensitivity, which may increase the biological vulnerability to psychosis; or of science that tells of drugs that shrink the brain, with this shrinkage associated with worse negative symptoms and functional impairment; or of animal research that tells of why antipsychotics fail over time; or of science that tells of much higher recovery rates over the long term for unmedicated patients. Those are drug effects that are not immediately visible to the clinician, but rather are made known through the illuminating powers of science, and they pertain to those with “clear cut psychiatric disorders” too.”
Now some of the most well known dissidents in the field seem to think that there is a more reasonable patient-centered alternative to discouraging long-term use of neuroleptics. There are a number of reasons why this is not true. Let me mention two. Even if there were some patients for whom long term use of anti-psychotics were optimal, we would not be able to identify them in advance.
As you say the drug effects of long term use cannot be known in advance, they “are not immediately visible to the clinician.” Nor are they visible to the patient. Some clinicians think that these effects are visible to patients –if mental health professionals only ask the right questions over and over ostensibly a group of neuroleptic- responders will gradually emerge. Dr Moncrieff writes, “Psychiatrists need to support people to evaluate the pros and cons of antipsychotic treatment FOR THEMSELVES [my emphasis] and to keep doing this as they progress through different stages of their problems.” I think the effect will be that more patients’ lives will be ruined by the drugs. I will grant for arguments sake that a few genuine responders to long term use will be identified. Still we will increase the false -positives and overall do more damage. Let us remember –as Moncrieff notes–that even those genuine responders are not invulnerable to tardive dyskinesia, diabetes, akathasia, brain damage, tardive psychosis etc
Second, I do not believe there are genuine responders to long term use of neuroleptics. There are responders to the placebo and the nocebo effects which are confounded with the positive reinforcement given to compliant patients; thus the compliant patient’s satisfaction grows with the approval of her psychiatrist–and therapist and families and friends all of whom say “Take your meds”‘ These are the ALLEGED long term responders to anti-psychotics–but they pay a high price for this social approval.,Psychiatry’s approval is conditional on patients’ compliance with the anti-psychotic regimen.
You have said Bob that psychiatiy should commit itself to minimizing long term use of neuroleptics.
To me this translates into a moral obligation for clinicians–particularly psychiatrists–to say to their patients,”I encourage you not to take anti-pychotics on a long term basis. I think you can do it.” And we need to realize that one cannot take a “neutral” position– as if the patient can make a decision that is itself pure, free of social influence. Thus relieving the clinician of the responsibility to take a stand. I think the idea of socially unbiased pure decision of the patient is the illusion that informs the position of otherwise strong dissidents like Joanna Moncrieff.Considering the enormous social pressures on patients to take drugs it is particularly incumbent on dissidents to say to patients, “I am confident that you will do well without needing those brain-damaging drugs.’
Report comment
I agree with you, Seth.
Given the evidence, I don’t see how we can ethically recommend neuroleptics for anyone. Especially since there are so many alternatives, and more could be developed if there was a will to do so.
If one must use a drug for acute psychological crisis, why not use short-acting opioids as an adjunct to social support? They are calming and induce a sense of well-being when people are frightened or in pain.
As with post-surgical pain, withdrawal or dependence is not a problem after a few days of opioid use. But I cannot imagine the establishment going for that. Too much is invested in the way things are. And too little is invested in providing what people really need.
Report comment
Susan
Opioids?: The government and medical establishment are trying to prevent even people with chronic pain from getting opioids, even though only a tiny percentage of opioid addicts got them from doctors. (Ironically NSAIDs like ibuprofen are much more harmful.)
I think opioids make people feel too good–so the establishment doesn’t like them. They probably would be helpful for many people in a state of panic, as would benzodiazapines, but apart from financial factors, “anti-psychotics” are –like “schizophrenia” itself– a sacred symbol of psychiatry–they are integral part of metanarrative about “psychosis.”
But my point is dissident professionals should not wait for their “patients” to weigh “the pros and cons” of neuroleptics–of a chemical lobotomy–, as some dissidents have advised here at MIA. They should act with authority as mainstream doctors do, and are expected to do, and tell their patients on the basis of experience and familiarity with the “science”,”I would advise you not to take anti-psychotics–particularly on long term basis because…”
In a humane society they would have been phased them out of existence. As you say there are many positive alternatives…
Seth
http://www.sethHfarber.com
Report comment
I agree with you. I have often wondered why opioids weren’t used during the first psychotic break to calm me down in the hospital without all the restless side effects of anti-psychotic medication, and then remove me from them before I got too adicted to them. The withdrawals would have been mild in comparison to Geodon. And no movement disorder.
Report comment
Epthe,
Why? I hope you are not still wondering.
They don’t care about your well being and comfort–or not beyond the limits of very narrow parameters. Guild and pharm influences determine these parameters.
Seth
http://www.sethHfarber.com
Report comment
Why? But we must stop thinking that drugs are the solution for psycho-social problems! It looks like ants that eat the poisoned honey that has been deposited there to destroy them … Bon appétit! https://santeprosperite.files.wordpress.com/2011/12/aspartame_ant_poison_3.gif
Report comment
Seth: The medical community continues to push “medication assisted treatment” as goal #1 for the medical industry to “treat” heroin/opiate “addiction”. What’s that “medication”, exactly? Methadone. (Or some almost exact equivalent….) Methadone, an OPIATE. They’re even running ads on TV for a new DRUG to treat so-called “OIC”, – “opioid induced constipation”. (Why name the DRUG, and give it more free publicity than it deserves?)
Report comment
I agree, but would prefer, even high, doses of cannabis, as to my knowledge, the addictive effect is, if at all, purely psychogenic. Good luck. 🙂
Report comment
As with the pharmaceutical industry, the fundamental reason for the distribution of neuroleptics by psychiatrists is economic.
1) Income
Prescribing neuroleptics takes a maximum of 1/4 hour per patient.
_ A psychotherapy session a minimum of 3/4 hour per patient.
By prescribing neuroleptics, the psychiatrist triple his income.
2) Social demand
By prescribing neuroleptics, the psychiatrist effectively solves a social problem in 70% of cases in the short term. This is the one and only thing the society asks of him.
3) Dependence
After some months of treatment, if the person stops gradually, the “relapse” rate is doubled for 18 months (Wunderink, 2007). If the person stops suddenly, the relapse rate is 75% in only 3 weeks.
By the neuroleptics, the psychiatrist is assured to retain a customer for many years. The legislation on forced and compulsory treatments plays exactly the same role.
The psychiatrist acts exactly like a street dealer and the state, instead of repressing the dealer, forces the drug addict to consume his toxic.
Addiction is not an undesirable effect for the psychiatrist: it is the very purpose of treatment.
Thus the question of neuroleptics is far from being exclusively scientific: it is above all an economic, political and social question.
Report comment
The economic and political structure tends to define and frame perceived self interest so as to result in mind-share/market capture – and all of that is a form of mind control. The ideas generally under the heading of mind-control range from social engineering, PR, and narrative control – through to extremes such as MKUltra via the fragmentation of personality to program triggerable responses of otherwise suppressed or unconscious personality. In any case the nature of the control is coercive deceit.
Socialisation includes mind-control in all manner of ways – as part of induction and adaptation to a society predicated upon it as the means of the suppression of the feeling being and the limiting of consciousness to forms of substitution for genuine presence – and diversion from the inherent dissonance of a conflicted sense that becomes ‘unconscious’ while leaking out as undercurrent communication.
Coercion and deceit are part of the masking persona with which we become identified as our thinking – our core beliefs and accepted self-definitions which predicate our economic, political and social structures.
So an inability to maintain the mask of a kind of a mind-control already operating meets the energetics of guilted fear that operates a self-reinforcing negative. Now this is as true for the psychiatrist as the politician as the corporate, as the banker as the one whose life ‘falls apart’ or whose ‘reality breaks down’ or whose psychic-emotional conflicts overwhelm their capacity to manage their lives on their current basis.
I contd here:
http://willingness-to-listen.blogspot.com/2017/06/the-social-economic-and-political.html
Report comment
Yes I agree entirely but you omitted to mention psychiatrists role as junior partners of the pharmaceutical industry which makes billions on these life-long customers. And noew psychiatrists are expanding the market for neuroleptics to include infants.
It’s not just psychiatrists anymore–all(including other “mental health” professionals) are part of psychiatric-pharmaceutical industrial complex, which is as intractable as MIC.
sf
Report comment
Dear Mr Whitaker. I enjoyed this article and wholeheartedly support the views expressed. I just wondered of you could clarify one of the figures. On page 5 you state that 83% of subjects in the Leucht study fall into the “harm” category. This consists of the 59% who don’t respond to drugs and the 24% who would have responded to placebo. I’ve been puzzling over this. If I give 100 patients antipsychotics and 41 respond then, as you say, 59 are now at risk of adverse effects for no discernible gain. This means that you are classifying some of your responders as now at risk of harm. However, I don’t think it can be 24 patients as surely the only ones at risk of harm are 24% of the 41 who responded (roughly 10 patients) – who would have responded to placebo if they had been given this. Your harm category would then be about 69% (still a substantial figure, obviously).
Is it possible that another figure might be 41.5%. My imaginary cohort is actually 200 patients. I give 100 the antipsychotic and 100 nothing. Overall, 59 from the first group are now at risk of harm and 24 from the second group are also at risk (as they would have responded to a placebo) this means that the calculation is 83/200 = 41.5%
None of this addresses the assumption that you are never at risk of harm from a placebo and we know that some patients in trials do suffer side effects from placebos. It’s difficult to explain this in terms of physiology but it does happen. The assumption that those who don’t respond to placebo are not at risk of any harm is therefore perhaps a theoretical one rather than one that is borne out by study results.
I’d be interested in any thoughts you have, It’s entirely possible that I’ve just misunderstood the figures completely (not an unusual occurrence for me!)
I wondered if the true figure for those in the harm category should be
Report comment
Sparkytus:
The NNT is used to assess the benefit/risk equation of a treatment. In this instance, 59% of the group are non-responders, and thus they have been exposed to the adverse effects of neuroleptics without any benefit. They are thus among the harm group. As you write: “If I give 100 patients antipsychotics and 41 respond then, as you say, 59 are now at risk of adverse effects for no discernible gain.
But you also have to add in to this harmed group those who would have responded without access to drugs (percentage of placebo responders.) They are also in the harmed group because they are now exposed UNNECESSARILY to the adverse effects of the drugs.
So total harmed group is 59% plus 24%, or 83%.
Another way to conceptualize the NNT numbers would be this. Imagine 80% of all patients with a certain disease respond to the treatment. This is a very effective treatment, right? Well, if 80% of all such patients also respond to placebo, then you have a treatment that produces no additional gain in response rates, yet all patients are exposed to the adverse effects of the treatment. Under NNT calculations, 100% of the patients would be seen as harmed. The 80% who would have responded to placebo, and the 20% of non-responders–all patients have been unnecessarily exposed to the adverse effects of the treatment, given that the response rate between treatment and placebo is the same.
I hope this makes sense,
Bob
Report comment
Is it possible to give a rough guess on the effect of antipsychotics on recovery?
Thank you Bob for answering.
Leucht et al has 2009 found (How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials) the effect NNT=6. However this was looking at symptoms.
Bola et al. Cochrane.org 2011 found just 5 studies with real placebo, i. e. RCT. One og them Rappaport et al 1978 found that umedicates pasients managed better, e. g. readmission into hospital. NNH turned out to be 2.9 (NNH= number nead to harm).
Nancy Sohler et al. gives 2016 this summary: «For many years, this (…)clinicians’ belief in the need for long-term use of antipsychotic medications strong (Lehmann, 1966) that it has been impossible to design a sound observational study to address the question of efficacy or harm … (O)ur study also could not conclusively evaluate whether long-term antipsychotic medication treatment results in better outcomes on average. We believe the pervasive acceptance of this treatment modality has hindered rigorous scientific inquiry that is necessary to ensure evidence-based psychiatric care is being offered.»
So as I understand there are nearly no RCT controlled studies answering my question on recovery.
However is it possible to give a very rough guess?
Approx. 60% or so of first-episode patients may recover without the use of antipsychotics.
Jaakko Seikkula has reported on long term outcome of first-episode psychotic patients treated with Open Dialogue Therapy in Western Lapland approx. 80% recovery. Showing the benefit of using not much medication supported by psychosocial care.
Bjornestad, Jone et al. 2017 reported “Antipsychotic treatment: experiences of fully recovered service users”: “(b)etween 8,1 and 20% of service users with FEP achieve clinical recovery (Jaaskelainen et al., 2013)”.
Now I know this guess is not exact science, but does it seem that approx. 40% of pasients subject to regular medication (e. g. in Norway “National guideline for diagnosis, treatment and follow-up of individuals with psychotic disorders”) loose long term recovery compared to nonmedicated pasients?
Would this be a fair rough guess of the long term effect of antipsycotics on recovery?
I would appeciate your answer based on your knowledge of studies. Thank you in advance.
Report comment
Walter K, My observation of patients, over 34 years, as fellow patient, is that they get better on their own, yes. I have seen it with my own eyes. If you observe, people do.
Any form of “treatment” sustains the belief that there is an “illness.” Therefore, “treatment” sustains and prolongs any “illness” state there is, causing more illness and ultimately, early death.
I don’t know about anyone else out there but to me it’s just plain ole common sense. Which we as a species should use more often.
Julie
Report comment
Julie G, thank you for your answer. I have the same personal experience from myself and relatives.
However psychiatry does not listen and acts different.
Walter
Report comment
I think a found the answer: “A critical review reveals that this paradigm of care worsens long-term outcomes, at least in the aggregate, and that 40% or more of all schizophrenia patients would fare better if they were not so medicated. ” in “The case against antipsychotic drugs: a 50-year record of doing more harm than good.” https://www.ncbi.nlm.nih.gov/pubmed/14728997
Report comment
Great article, Robert!
It leaves me with a couple of questions.
This may be a moot point, but how do you assess the role of guild as greater than Big Pharma?
They seem to me to be so intertwined. And then there is the role of the government in many ways.
When Regan introduced neoliberalism to the US policies, many people lost their jobs and of course were depressed. That’s the same time that Prozac came on the market. Doesn’t seem coincidental to me.
As an example of Big Pharma’s interventions, check out NAMI, who are hugely funded by them. They reach many families convincing them that mental illness is like other illnesses–not to be stigmatized, but instead to be treated with medication, like any other illness.
As to your question of how to make reforms, have you ever submitted to the American Journal of Psychiatry or Psychology Today, or written letters published in any other format that might be read by med students or guild members?
Thanks again,
Don
Report comment
I just lost a close 63 year old friend who has been on antipsychotics for years. I always feared this would happen because it caused various health issues. Lieberman and all the psychiatry drug zealots can go to hell.
Report comment
sorrows for your loss.
bizarre that not even one person acknowledged you. how inhumane.
maybe we’re all animals, monsters, robots and puppets now. never gonna be true humans ever again.
Report comment
Thanks, Bob, There is so much corruption going on behind the curtain at the uppermost levels. I am surprised Lieberman is still alive.
I have tried to get a grasp on the dopamine super-sensitivity thing. Does anyone out there know if this is what causes our permanent, hellish insomnia that plagues so many of us, on or off drugs, in our later years? This is totally separate from apnea, which seems to be a separate issue though overdiagnosed for sure. I for one cannot sleep at all without chemicals. and this seems to be permanent damage.
Or, is it that epigentic methylation thing? Does anyone out there have an actual cure? Even the supposed cure my naturopath suggested doesn’t really work. Anyone out there please contact me if you have any answers, many are desperate……..
Report comment
Awesome article and exactly what in needed to shove wikipedias article about schizophrenia in the butte, lol.
I want to answer to some comments here:
The truth about mental illnesses can be found out, but some might need help.
I am a marine biologist and have learned to test my hypothesies.
When i had my bouts of psychosis. i tried to remain calm and test every foreign thought as good as i could and later on forced medication, tested the ability of neuroleptics to influence aberrant thought.
My findings were that neuroleptics do not help at all in cognitive processes. I can still spin very fantasy, like.
But what is not fantasy is the existence of souls and the survival of the individuality of a complex live-form, even after death. As the (still) prevalent opinion throughout the world, i never dared to deny its existence and when shit hit the fan (so to say), it remained the only valid explanation of what i had experienced. I will not go into detail here, but can say that some of my “angels” dare to talk within my head sometimes and they are distinct from me.
This doesnt help against truly aggressive souls, but the insecurities about inferiority, suicide and destruction of the (never having died yet) ego, that body forms in life, simple can be “externalized”.
I want to prove that with the creation of a open science database with case essays in order to show the similarities in modern psychologic afflictions, arguing for the unlikely of a evolutionary brain that has neuronal algorythms for suicide, technophoby, superiority and inferiority complexes, etc.
This database shall also encompass a report section for complains about psychiatric misstreatment in order for compensation and cessation mass-law suits or similar.
Please do not attack me for my “awakenedness”, or i might tell you what a SH*T-Brain your inner demon is. Have fun and be good! 🙂
Report comment
*every fantasy, i like (sorry :))
Report comment
Found this via a link from Wikipedia, and parts of this article mirror my partner’s experience in the UK. She was given anti psychotic medication after a single psychotic episode at age 19, and sure enough 2 years later when she stopped taking the meds she had a relapse which prompted psychiatrists to advise her she would have to take them indefinitely. Despite this “advice” and after 12 years of various different meds
(mirtazipine, Trifluoperazine, aripiprazol/abilify) she tapered off the drugs slowly and along with cognitive behavioural therapy, counseling and other talking therapies has been well ever since. I am convinced she could’ve recovered from the initial illness all those years ago with the right treatment and without the anti psychotics, but it was easier for Drs to follow what increasingly looks like a flawed protocol and just medicate.
Your team is doing some great work, keep it up.. maybe the John Arnold Foundation and it’s fight against bad science could help!
www wired com/2017/01/john-arnold-waging-war-on-bad-science/
Report comment
Babylon mek me sad an mad so:
http://www.schizophreniaforum.org/news/meta-analysis-ranks-antipsychotics-efficacy-side-effects
If anyone could provide additional research on non-effectiveness of neuroleptics, it would help greatly in editing:
https://en.wikipedia.org/wiki/Schizophrenia
Particular modern review (bloody-peer-reviewed) articles and meta-analysis (LOL, meta-analysy?), would be helpful.
I will use the authors articles, even if i have to argue myself to the top, but a broader base would from “reliable sources” would be very nice. I think this is very important, as i consider wikipedia the main information source for many that are not directly involved in anti-psychiatry.
Thank you and good luck. 🙂
Report comment
Love this article, Mr. Whittaker!
Like Susan Rosenthal, I too am a grad school educator. However, I am “closer to the edge of the abyss” as I teach Intro to Clinical Psychopharm and Psychopathology at the Chicago School of Professional Psychology. I am one of several faculty who use your writings in classes, and who strive to encourage critical thinking and skepticism about the current toxic atmosphere in mental health.
I’ll play a bit of devil’s advocate here, however,in order that we don’t swing the pendulum too far to the other side. As much as Lieberman and the Liebermen do their best to snivel and deceive, one point to salvage is that some people with schizophrenia do in fact benefit. Two truths are (1) that this number is a lot smaller than organized psychiatry would like to believe, and (2) that we DO NOT KNOW who is whom: which people are better off taking them or not. That to me is the research mystery that must be solved. And to add to some of the great research details presented by commenters here, the brain imaging research does NOT help answer the key questions, not least because that field has its own systemic-guild problems…
I warn my psychopharm students that it will be a VERY pessimism-inducing course, with few answers and few solid recommendations. I can’t imagine that this tone is conveyed in med school…
One aspect that is more encouraging to me is the growing acceptance that mental health is about more than the brain, something that will ultimately require psychiatry to make substantial adjustments in their model.
Another is that pharma is investing less money into researching traditional psych meds, so there is less pharmalfeasance. Thus more psychiatrists consider themselves “neuro” or “bio” doctors. For the rest of the meds, it’s more about generics now.
The overall way I explain psychotropic meds is as a means to help people better use other modes of intervention. But the meds do not work on their own, nor should they be used for an extended period of time–how long? *shrug* But they contribute to the more general process of learning how to manage life, how to change old patterns of behavior, and perceive experiences differently. It’s like someone helping push your car out of a ditch when it’s stuck in the mud or snow. You’re spinning your wheels with no hope of getting out on your own. However, you certainly don’t need that person hanging out in your trunk after you are out of the ditch!
In any case, thanks kindly and greatly for your in-depth response to this “sell job”
Looking forward to having my students read and incorporate it.
Ken Fogel, Psy.D.
Report comment
With little respect for the Psy.D. Mister Ken Fogel,
the “positive effects” of neuroleptics are sedation alone, e.g.:
http://medical-dictionary.thefreedictionary.com/neuroleptic
I can have that from natural, much less toxic (ever heard of LD50, “biodoctor”?) substances like:
ethanol, cannabis, opium, khat, etc., which also have an, in e.g.”schizophrenia”, often welcome effect of euphoria and the production could help many very poor communities instead of big-pharma.
There is an extensive amount of “new” research to sell this “rat-poison” to even more groups of ill or unwelcome people, find markers and genes, animal models and new types of “psychotropic” drugs e.g.:
https://www.ncbi.nlm.nih.gov/gquery/?term=neuroleptics
They DONT HELP people to use other “modes of intervention” e.g.:
https://simplecapacity.com/2017/08/what-a-shaman-sees-in-a-mental-hospital/
http://psychrights.org/Research/Digest/Effective/MIrwinNonDrugSchizophreniaTreatment.pdf
If you want to be a psycho (soul) doctor ((dunno) fixer (maybe)), be my guest,
but you might want to scream into the silence behind your eyes,
whether there is something that wants to talk, listen, care, explain, ask, define and console and generally is knowledgeable enough to explain everything a traumatized person might experince in a HOLISTIC, and PRODUCTIVE way.
I studied Biology (Knowledge of Life) and found death behind my eyes and everywhere as well.
It is often called “awakening” and is a blessing. But i was diagnosed and “force treated” long after any “positive or negative symptoms” and thats a clear violation against this:
http://www.un.org/en/universal-declaration-human-rights/index.html
AND this
http://www.un.org/disabilities/documents/convention/convoptprot-e.pdf
Good luck to you and you and all of us, but in my I&I, you sir, are a bruha! 😉
Report comment
OK, so you disrespect my education. Not necessarily relevant to the discussion, certainly rude. But whatever.
I’m sure you realize that “natural” does not mean “less toxic,” and listing ethanol among the drugs you listed was, well, unfortunate for your argument.
You provided a link to a list of potential articles about neuroleptics. Not very helpful.
You provided two links in response to my suggestion of other modes of intervention. One to a blog entry about a shaman’s visit to a mental hospital, which highlighted the importance of considering difference in worldview. I certainly don’t disagree with the premise or conclusions of the article but wonder if you are suggesting that Westernized people consult a shaman for their condition and expect positive results.
The other link to a review of studies that demonstrate the effectiveness of therapy without medication is helpful, thank you.
I have helped many people with trauma, in my own, “Psy.D.” way, and I believe my understanding is just fine, thank you.
No need to link to the laws.
… and then you refer to me as a “bruha,” the meaning of which I was ignorant. Looked it up. “Witch, hag,” or “asshole.”
Nice. Whichever one you meant, winking emoji or not.
You might want to look into the nature of your “awakening,” and wonder how you could talk to people this way…
No need for me to respond to anything further you say.
Report comment
No need to discourse further in that unscientific way of yours, i concur.
A bruha (the spelling varies) is a shaman that is considered bad. Like in spirits that hurt, associate with them and make it possible to fake healing by leaving when due pay is exacted. The opinions on good and bad can vary greatly among the respective clients and you might not be aware of it and therefore not fit the definition.
Natural means certainly less toxic as synthetic:
1. It developed by “natural evolution” or “intelligent design” and is not supposed to hurt the “victim/patient” as they are often beneficial to the e.g. plant by distributing seed, polinating, acting in a general beneficial way on the rest of the eco-system.
2. Their uses form a strong symbiotic bond with with the lifeform (e.g. has a better survival chance than “weeds”, and spirits of the agents, like in:
https://en.wikipedia.org/wiki/Animism
Your comment on ethanol shows very good how much psychiatry and non-soul-based-psychology are a pseudo-sciences:
E.g. I can drink about 5 liters of beer before having to sleep and often have a great time until then.
5 liters a 5% ethanol equals 250ml ethanol loosely transform to 250mg ethanol. Now which psychiatric drug has a similar effects at that dose?
I was forced to take 16mg of haloperidol per day for 3 weeks with no positive effect. I dare you to take 250mg haloperidol! That is what toxicity and “Lethal Dose at 50%” is about.
I have consumed highly diluted ethanol (beer, cider, etc.) for more than 20 years with no medical perceivable ill effect, while 7 years of forced neuroleptics left me various physiological “disorders”.
LOLOLOL: “potential articles”…
I dont know of any successfully practicing “shamans” but the spirits that define them are still around sometimes, associating with a single individual or acting as a free agent. Quite a few “western” people visit (apparently in your world-view “non-western”) shamans with reported positive effects.
That is the big question: What is your “own Psy.D. way”? You question valid scientific research. You teach. You “help many people with trauma.” And you “BELIEVE”!
“Awakening” means that you get shown and become to KNOW, that the spirit world is real.
I gave up after, first you, lets say “form a bond” with your newest client and then write:”Most people don’t know what they really need”, and defined you as a bad man(s).
“No need to link to the laws.”, with respect to the, above mentioned argument, just makes me think that your definition of bruha is the more accurate.
Again, i wish us all the best. 🙂
Report comment
Can you give an estimate of the percentage of pasients who benefit of medication with antipsychotics. Do you refer to reduction of symptoms opening up for other intervetions?
From a pasients perspective I would like to add recovery as aim. What is the effect of neuroleptics on long-time recovery?
Leucht et al has 2009 found (How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials) the effect NNT=6 (1). However this was looking at symptoms on the Positive and Negative Syndrome Scale (PANSS).
Bola et al. Cochrane.org 2011 found just 5 studies with real placebo, i. e. RCT. One og them Rappaport et al 1978 found that umedicated pasients managed better, e. g. readmission into hospital. NNH turned out to be 2.9 (NNH= number need to harm).
Nancy Sohler et al. gives 2016 this summary: «For many years, this (…)clinicians’ belief in the need for long-term use of antipsychotic medications strong (Lehmann, 1966) that it has been impossible to design a sound observational study to address the question of efficacy or harm … (O)ur study also could not conclusively evaluate whether long-term antipsychotic medication treatment results in better outcomes on average. We believe the pervasive acceptance of this treatment modality has hindered rigorous scientific inquiry that is necessary to ensure evidence-based psychiatric care is being offered.»
So I understand there are nearly no RCT controlled studies (avoiding «cold turkey» problems) answering my question on recovery.
However is it possible to give a very rough guess?
Approx. 60% or so of first-episode patients may recover without the use of antipsychotics.
Jaakko Seikkula has reported on long term outcome of first-episode psychotic patients treated with Open Dialogue Therapy in Western Lapland approx. 80% recovery (6). Showing the benefit of using not much medication supported by psychosocial care.
Bjornestad, Jone et al. 2017 reported “Antipsychotic treatment: experiences of fully recovered service users”: “(b)etween 8,1 and 20% of service users with FEP achieve clinical recovery (Jaaskelainen et al., 2013)” under the profession’s current protocols.
Now I know this guess is not exact science, but does it seem that approx. 40% of pasients subject to regular medication (e. g. in Norway “National guideline for diagnosis, treatment and follow-up of individuals with psychotic disorders”) loose long term recovery compared to nonmedicated pasients?
Would this be a fair rough guess of the long term effect of antipsycotics on recovery?
Patients have a right to know in advance to decide with informed consent the benefit of actual symptom reduction in the beginning at the price of long-term reduction of recovery. What will your students be able to tell their pasients?
I would appeciate your answer based on your knowledge of studies. Thank you in advance.
Report comment
Hi Walter, I am afraid I am going to disappoint you, which is unfortunate given the time and effort you put into your comment.
However, I will offer some food for thought that might address some of what is driving your questions (if I’m wrong in this, I apologize in advance):
– First off, no, I cannot offer you a numerical estimate. Meds only reduce sx; recovery is indirect effect only;
– I tell my students that no prescriber can tell any patient when to STOP taking their meds, certainly not based on research. Pretty much all of psychiatry is about what to START and sometimes what to change. But the sooner you can get people off meds the better.
– For the consent issue, in general, for all patients, they need to know that there are always costs/benefits to taking/not taking meds. Typically, the choice is “experience symptoms” or “experience side effects.” For people experiencing psychosis, can they manage their hallucinations on their own or with the support they currently have? If so, great! However, if they cannot, they face that decision. Some will, reluctantly, choose the meds. Not everyone with psychosis can “tough it out,” or manage their lives by sheer force of will. Sure, some can. But if you read the studies that are pro- or anti-psychiatry, the common theme is that there are always people in the “non-successful” group. On both sides of the argument. If you spend too much time on your own side, you neglect to see the other side.
– So, in terms of consent, people need to know that a big part of this whole enterprise is guesswork. However, if you have a decent and empathic provider, your chances of success are greater, just from the standpoint of wellbeing. Call it placebo if you want but that does not diminish the positive effect.
– The problem with using research studies to help people make decisions is that they are based on group statistics. They don’t apply to individual cases. Does it help someone to tell them that there’s a 40% chance of improvement? An 80% chance? What does that mean FOR THEM? What does it mean if they choose the treatment with an 80% chance of “success,” but it doesn’t work? Is there something wrong with them? With the treatment? With the provider? I find that this limits the clinical utility of Cochrane studies. Especially in their studies of meds for mental illness/behavioral health, there are so few good/reliable studies to base their conclusions, that the conclusions are almost always “no conclusion can be made…”
– A wonderful question to ask a prescriber/physician is if she/he would follow the same protocol with a loved one. And jump on any hesitation. Then you’ll find out the real issues about the treatment. Any clinician who refuses to answer or is uncomfortable with such a “role reversal” is not someone I would want to see for treatment.
– Another common theme/recommendation of sorts has to do with mindfulness. Increasingly found to be beneficial or effective or whatever you want to call it. If you have a “monkey mind” like most in Western society, trying to be mindful is about as hard a task as you will find. I don’t think it is coincidental that cultures who are more attuned to their present being/context have fewer mental health problems, and those with diagnosable disorders fare better in the treatment offered in those countries (like India).
So, I apologize again. If you still want some numbers, I can dig some up for some of your questions, or at least in an indirect way, since we know how little there is out there. However, it looks like you are very well read up on this.
Take care and thanks for the thought-provoking commentary
Ken
Report comment
Hi Ken, I had to look into it myself. The result is:
Neuroleptics are used to ease symptoms and to prevent relapse with evidence at the beginning of the psychosis for a minority of patients. There is no evidence that antipsychotics promote “psychosocial functioning, professional functioning, and quality of life” (Buchanan et al 2010 PORT Treatment Recommendations). Recovery treatment still wins terrain and will be put into a historical context. Mike Slade et al. 2014 describes the implementation of recovery with both usage and abuse of the term. Too high doses of neurroleptics to too many patients over long time cause catastrophic poor treatment outcomes regarding recovery, disability / illness and chronic illness. A paradigm shift to lower doses for fewer patients over a shorter period of time with, for example, Open dialogue quadrupled recovery, reduces schizophrenia per year to one tenth and disability benefit / illness decreases to one third.
http://wkeim.bplaced.net/files/recovery-en.html
http://wkeim.bplaced.net/files/Dialogical_practice_is_effektive.png
Report comment
Hello walter.keim,
have you read this article:
https://www.madinamerica.com/2016/07/the-case-against-antipsychotics/
And this:
http://psychrights.org/Research/Digest/Effective/MIrwinNonDrugSchizophreniaTreatment.pdf
…already?
I want to add, that, since psychosis is psychogenic (personal experience), recovery with antipsychotics doesnt prove effectiveness of neuroleptics and compliance and reliance on them might hinder recovery in that the wishes of the effecting spirit(s) might be ignored. I consider the most “positive effects” of antibiotics as a bad sign, in that the effecting spirit might wish to hurt physiological and long-term. Personal experience makes me believe, that enduring and testing the emotional and cognitive “hypotheses” is usually welcomed by positive thinking souls. But that was not your question, sorry.
I have copied your comment for citation purposes and would ask you to participate with any scientific negative analysis of the positive effects of neuroleptics under the following link (which might contain further valid citations for you:
https://en.wikipedia.org/wiki/User_talk:Jytdog#Schizophrenia
Thanks and good luck.
Report comment
Nradabhatse die Katze:
Thank you for your answer.
Yes I have read the article “The Case Against Antipsychotics” and “Treatment of Schizophrenia Without Neuroleptics: Psychosocial Interventions Versus Neuroleptic Treatment”. Very interesting.
I knew http://psychrights.org. The link http://psychrights.org/Articles/articles.htm is new for me and I enjoyed to read the latest news from Open dialogue of Jaakko Seikkula.
The context I am working on is a follow-up of “Knowledge- and research-based liquidation of current harmful psychiatric medication in favour of evidence-based practice to promote recovery” http://home.broadpark.no/~wkeim/files/open_letter_knowledge.html (sorry for bad language: English is not my mother tongue) about the conference at the House of Literature 8th February 2017. “What is the knowledge base for treatment with or without the use of psychotropic drugs?” with Whitaker and Jaakko Seikkula.
Now I search to try to quantify the negative long-time effects of the current protocol of teatment.
I am sure to need good luck 🙂
Report comment
Awesome some work professor Keim,
i dont have the inner calm to asses and include all the provided resources right away, but have copied it to the wikipedia link and would like to publish it, with your permission on:
https://web.facebook.com/groups/1564150087162991/?ref=group_cover&_rdc=1&_rdr
You will need more than good luck, i agree.
I havent specifically searched in regard to your project, but think that we have to do it ourselves.
Within a Truth and Reconciliation (+Compensation 🙂 ) setting, i want to initiate a database project of search and quantifiable case reports in order to show and analyse common themes of psychosis and compute damages and amount of arguable dept to the patients.
Now, i alone can maybe define the database but thats about it. MIA has a case report system, but i do not know whether they intent to process the data and how. I have sent emails about this proposition to some open science projects with no answer, yet.
But my current doable project is to broaden the group of informed people on/through wikipedia.
Suggestions regarding these projects would be welcome here and on [email protected] or the End Psychiatry link.
Thanks and in addition to good luck, success. 🙂
Report comment
I suspect, Mr Fogel and anyone, that we all define “benefit from drugs” differently.
For instance, I recall someone went to her doctor for drugs. He tried many. He was giving her drugs for depression and asked her if the drugs were “helping.” Finally, she told him that the third was best “because finally he ha given her something that helped her sleep.” This is an example of a short-term miscommunication with minimal harm, I hope.
Define benefit. I asked for pills. I was given pills and asked if they were “helping.” I noticed Lithium helped with my eating disorder. I said, “Yes, it does.”
They said, “Oh, so it helps with your bipolar.”
I said, “No, I came with an eating disorder, not bipolar.”
They said, “We don’t notice an eating disorder.”
For 30 years, I judged “effective” by how well a treatment helped me with ED. THEY judged a treatment by how little I “complained” afterward. Much complaining got me a paranoia diagnosis., or an accusation of “whining.” Yes they didn’t help much at all.
That I know of, patients define “it’s working” differently. Some even want a high.
Julie
Report comment
Hi, Julie.
I’m very, sincerely sorry that you, and the person you recall, went through that experience.
First of all, right off the bat, someone should NOT be going to the doctor “for drugs.”
Second, asking if drugs are “helping” is not helpful. We need to ask, “how are they helping/not helping?”
Third, giving drugs “for depression” is almost always pointless. Now, giving drugs to help someone sleep, maybe, but also not particularly helpful. Meds are for symptoms, not disorders. I disagree about the “minimal harm,” though, because it was based in miscommunication. The relationship and communication are everything.
Fourth, “benefit” means what it sounds like it means: help. How did the lithium help with the ED?
Fifth, “helps with your bipolar” is a stupid sentence, a waste of energy and breath, meaningless and foolish.
Unfortunately, in this day and age, with internet “self-help,” layperson misunderstanding of the kinds of info available online, evil marketing by pharma, spineless prescribers, and everyone’s desire to feel better quicker, meds are the thing.
Fact is, most things that are worth anything in this world take time, effort, and commitment to get over the initial hump. Most people don’t understand how therapy works. Most people don’t know what they really need. Most people don’t really listen to other people. etc.
Like I said, I feel bad that you had to experience such stress and heartache.
Hope what I said makes sense.
Ken
Report comment
Ken, I can talk till I’m blue in the face but that won’t stop my friends/acquaintances from going to doctors to beg for pills. They still think that’s what doctors are for. I can argue and argue but it’s useless. I myself was not raised with this “take a pill” mentality. When I first came upon it I was shocked. “Why take pills?”
A few years later it had rubbed off on me, though. I suffered from an eating disorder and no therapy ever helped in three decades. I found therapy imposing and abusive. I had over 20 of them. The decent ones didn’t stick around very long. Therapy sustained me in a disabled state, encouraging me to stay disabled. Sadly, in three decades they barely acknowledged I had an eating disorder even though I told them clearly!
By 1982, which was early on, I had concluded that therapy wasn’t going to help, so I figured pills might. There was research stating that pills help binge eating. The research was on the antidepressant imipramine. The book is out of print but it was done by prominant researchers. This went on to prescribing SSRI’s, Topamax, and now, Vyvanse.
Frankly, I think they’ll find Vyvanse as disappointing as the others, but let’s just say it’s pulling in a profit. My own experience is that ANY drug that reduces appetite in just the right way at just the right time will stop binge eating rather effectively, as will certain foods if eaten at the right time. You can also change up the order you eat your meals and this will do the trick, or, for some, eliminate or add certain food. Some find elimination of “trigger” foods helpful.
I found that lithium worked. It is known to put on weight, but for me, it reduced my appetite just enough. I had no clue, at the time, exactly how it was “working,” but the “effects” were immediate, dramatic, and very noticeable. TO ME.
However, because because binge eating is ALMOST ALWAYS done in secret, no one else noticed the difference. So the residential center I was staying at failed to validate that the Lithium had helped my ED.
This is very sad.
The last day of my lengthy stay there, in 1984, I met with the director. I told him, “I’m very happy. The lithium has obliterated my eating disorder, so now, I can go on with my life.”
He said, “You never had an eating disorder. It must have been very minor or you were only imagining it.”
I felt incredibly crushed. He was so wrong. After I left there, I was called schizophrenic because they assumed I had only invented my ED. It took three decades and nearly starving to death for the world of Mental Health to finally wake up.
I got over my ED by leaving MH “help” far behind, by ditching all the lies they told me, by ending all supervision and doing it all myself, by getting rid of the diagnoses, and by living as a free, undiagnosed person. I would wish the same freedom for anyone.
Julie
Report comment
Dear Walter, I knew many who took them, may or may not have “felt better.” They are mostly dead now.
I, as former patient, am happy not to have my head clouded nor too puffed up by an MD degree…..But saddened to lose so many to this obvious scam. This was not a “tradeoff” by any means. The price was too high to pay, for these unfortunate people taken too young, and for their families.
Julie
Report comment
Dear Julie, yes I think I understand. Both my own experience and the experience of my relatives as well as the statistics that people living with antipsychotic drugs live approx. 20 yeras less supports what you are writing.
Walter
Report comment
A lot of the people I knew who also took these drugs, are now also dead.
This is a Research Paper written by my Former Consultant Psychiatrist on the drugs that nearly killed me.
“Depot Antipsychotic Revisited”
http://ps.psychiatryonline.org/doi/abs/10.1176/ps.49.10.1361-b
Dr P A Carney (and others)
CRITICISM OF THE RESEARCH PAPER
(in brief)
Suicidal Reaction to these drugs as witnessed by my Consultant Psychiatrist PA Carney is not acknowledged in this Research Paper.
Severe Adverse Drug Reaction as these drugs are prone to cause is not mentioned in proportion.
‘Rebounding’ as a result of coming off medication, is wrongly categorized as ‘Relapsing’.
This Paper is ignorant of Withdrawal Syndrome – where a person runs into problems as a result of coming off drugs. This denies Medical fact.
The Blunt Reality is that Mental Health Diagnosis like ‘Schizophrenia’ , as referred to in this Paper cannot be relied upon because of the embedded dishonesty among Mental Health Professionals both in Ireland and England.
MH Dishonesty:- For example when I came to the UK in 1986 Requested Adverse Drug Reaction was deliberately Omitted from my Irish History. My History was also changed around to hide these Reactions.
MH Dishonesty:- Originally at Galway in November 1980 I was examined by a non European Doctor who judged me to be quite well. Yet Galway took their lead on Mental Health from UK sources who were very careful not to commit themselves to much.
The inclusion of the Community Nurse in this Paper seems a bit ominous, as the same nurse called to my house when I didn’t turn up for ‘my injection’. We had a civilised conversation at the time regarding my ‘involuntary movement’ problems and he recommended I do take these to my Doctor. But this conversation and it’s content was not recorded in my (FOI requested) notes.
In this Paper the depot medications are referred to as Economical options – this is NOT true.
There’s a Strong Financial and Corrupting Incentive attached to this Drug Research
https://www.nuigalway.ie/our-research/partners/
€9.6 million from Bristol Myers Squibb the Manufacturer
DENIAL OF RECOVERY
Research University NUIG in contradiction to their “purpose” do not acknowledge in this Paper Full Recovery from Severe Mental Illness as a result of discontinuing these Drugs and moving to Psychotherapy.
MY PSYCHIATRIC EXPERIENCE (IN BRIEF)
These drugs are given to “Severely Mentally Ill People” . I remained Severely Mentally Ill while I took them but I made Full Recovery when I stopped.
I tried to stop taking modecate depot injection because of its disabling side effects in October of 1983 and ended up in hospital in December of 1983.
This was considered to be Relapse, but I would describe it as a Rebound.
In hospital I was put back on the drug modecate at the introductory level of 12.5mg. The dosage was then increased. Following the dosage increase I had a suicide attempt while suffering from Acute Akithisia. I had had a similar suicide attempt some time previously under the exact same conditions.
I then attempted to withdraw from the modecate injection again but the anxiety became too much, and I sought help from my doctors. It was suggested to me that the depixol depot injection might have less extrapyrammidal side effects and that I might pchange to this drug.
I agreed to this suggestion and I turned up at the hospital and was injected with Depixol depot at twice the introductory dosage of 40 mg. even though I had explained to the doctor seeing me that I had experienced serious first time depot exposure reactions before.
When I woke the next day I was going crazy (with Akithisia) (similar to first time reactions I’d had before). I tried to get admitted to hospital but staff had been told not to allow me in. Eventually I was admitted, by the nursing staff.
I remained in hospital for less than two days and then I discharged my self. This hospitalization was categorized as a “Pre Psychotic Episode”.
This was my last hospitalisation. After this I moved to oral medication and tapered from there.
As a result of Stopping strong psychiatric drugs my Suicidal Episodes Stopped; My Hospitalizations Stopped; and My Disability Dependency Stopped.
I suffered from terrible Anxiety for a long time after discontinuing depot injection type medication. But I benefited from CBT type Psychotherapy and related activities like Meditation, Buddhist Philosophy, and Peer Groups. This anxiety has now reduced to a small fraction of what it was.
Report comment
Dear Recovered, I find my experience of “patients” is that they, too, stubbornly cling to the idea that “Doctor knows best.” Patients are lazy. They often staunchly refuse to do their own research. They refuse to claim autonomy and self-expertise, often deferring to the doctor over and over, even to the point of doc-shopping out of desperation for this “help” that doesn’t exist.
Recovery, to me, meant realizing there was no help. There is no help except the immense strength we each have within ourselves.
Julie Greene
Report comment
“If we can’t trust the profession to develop “evidence-based” treatments that put the interests of patients first, as opposed to their own guild interests, what should our society do?”
wait for jesus to destroy the antichrist, that’s about all. heh.
“The drugs were once again cast as essential and even as miracle agents (life-savers), and this became the narrative promoted to the public, and was repeated in stories published by UPI and on such websites as Science Daily and Medical News Today. Meanwhile, Lieberman also touted the importance of the study in a Medscape video, describing it as a “major development in psychiatry.” Dressed in a white coat, he said the study “came to a very firm conclusion as to the unquestionably positive benefit of these drugs,” and then he took aim at those who had dared to question their merits in the first place.”
Revelation 13:3 (TLB)
3 I saw that one of his heads seemed wounded beyond recovery—but the fatal wound was healed! All the world marveled at this miracle and followed the Creature in awe.
psychiatry the antichrist & DSM = 0
jesus & scripture = 1
*NOTICE: PLEASE IGNORE REALITY AND MAINTAIN THE DELUSION
Report comment
Thanks. Right on time.
Report comment
Thank you, please try to get this analysis published somewhere visible to psychiatrists and doctors. I was too sick to read this before getting off of Ativan, so someone like me would be unreachable. I’m tempted to send out the one longitudinal one over 20 years where people recover. Just straight in their mailbox.
Report comment
Open Letter to Donald C. Goff, Peter Falkai, Wolfgang Fleischhacker, Ragy R. Girgis, Rene M. Kahn, Hiroyuki Uchida, Jingping Zhao, Jeffrey A. Lieberman, Kim T. Mueser, US National Institutes of Health
Copy: Norwegian Health directorate, Norwegian Institute of Public Health
TAU falsified: Suggestion of further research with focus on recovery
I appreciate your constructive contribution: “Strategies for treatment discontinuation or alternative nonpharmacologic treatment approaches may benefit a subgroup of patients … More research is needed to determine whether some individuals may respond to alternative pharmacologic or nonpharmacologic treatments for a first episode of psychosis…” (Goff et al. 2017: The Long-Term Effects of Antipsychotic Medication on Clinical Course in Schizophrenia).
Based on:
size of antipsychotics effects,
increasing focus on recovery
falsification of current paradigm (Treatment as usual) i. e. recommendation that all individuals with new-onset schizophrenia should receive acute and maintenance antipsychotic treatment
further research is suggested with focus on recovery.
Effects of Antipsychotics
Antipsychotics are used to ease symptoms (Leucht et al 2009: NNT=6) and to prevent relapse (Leucht et al 2012: NNT=3) with evidence at the beginning of the psychosis for a minority of patients. There is no evidence that antipsychotics promote “psychosocial functioning, professional functioning, and quality of life” (Buchanan et al 2010 PORT Treatment Recommendations). Bjornestad, Larsen et al. 2017 admit that evidence of long-term maintenance medication is missing: “Due to the lacking long-term evidence base (Sohler et al. 2016) …” Current use of neuroleptics has been criticised. Studies show the advantage of a shift to minimal doses for fewer patients over a shorter period of time.
Recovery
Recovery is used in several meanings and has gained attention and has now become mainstream. Both the United States, Canada, New Zealand, Australia, the UK and Ireland are building their national strategies on recovery. The Norwegian Government’s Strategy for Good Mental Health (2017-2022) “Mastering Life” is based on WHO’s Action Plan 2013-2020 and The European Mental Health Action Plan 2013-2020 and EU JOINT ACTION 2016. The Norwegian Mental Health Expansion Plan mentions the needs of the user/patient as a starting point, “mastering one’s own life”, “successful return to working life” and “entering into a social relationship with family and friends” (Ottar Ness 2015). Recovery rates decreased: «17.7% in studies between 1941 and 1955, 16.9% in 1956–1975, 9.9% in 1976–1995, and 6.0% in studies after 1996» according to Jaaskelainen et al. 2013.
Harrow et al. 2007, Jääskeläinen et al. 2013, Harrow & Jobe (2017), Wunderink et al 2013, Wunderink 2019 look at recovery.
Naturalistic studies of Open dialogue reported good outcomes looking at recovery, reduces schizophrenia per year and reduced disability benefit. The evidence in support of OD has been criticised being of low quality, and randomized controlled trials are required to draw further conclusions.
Falsification of Treatment as usual
Tomi Bergström, Jaakko Seikkula et al. 2018 (1) compare FEP Open dialogue patients with all FEP patients in Finland over a period of 19 years. Open dialogue (OD) uses neuroleptics for 20% of patients in the beginning, standard treatment (CG control group) 70%. 97,3 % of the CG get neuroleptics at some point. At the end 36% of OD patients use neuroleptics, for CG it is 81%. Disability allowance, readmission and patients under treatment halves with OD, reflecting better recovery. This register study bypasses ethical and feasibility problems og long-term studies.
This register study reflects reality/facts about Finland on national level. Treatment as usual is falsified as the most effective treatment. RCTs could give further information which of Open dialogues approaches e. g. reduction of antipsychotic medication, immediate help within 24 hours, social network perspective, dialogue etc. contributes to the good treatment results.
Studies to find out why Open dialogue promotes recovery
Scientific studies can only explain reality not disprove. Respect of reality could considerable improve treatment and health of patients. Therefore I have asked Norwegian research institutions in 2018 to do further studies on a shift of Paradigm: Can Open dialogue improve recovery rate, reduce schizophrenia per year and reduce allowance/sickness?
Later a “Call for Studies to Find out why Open Dialogue Achieves better Results” to US National Institutes of Health, UK National Institute for Health Research Norwegian Psychiatric Society (NPF) and NORMENT: Norwegian Centre for Mental Disorders Research has been made: http://wkeim.bplaced.net/files/recovery-call.html .
Both National Institute of Health Research (NIHR) and The Institute for Dialogic Practice, Northampton MA already conduct research.
Would research with focus on recovery on the basis of exploring promising treatment results of Open dialogue be the way forward to promote and improve patients health?
http://wkeim.bplaced.net/files/Suggestion%20of%20further%20research%20with%20focus%20on%20recovery.html
Report comment
Scott Waterman, Professor of Psychiatry Emeritus at the University of Vermont, writes about his personal journey through psychiatry over the past several decades:
Why I Am Not a Psychiatrist
As the story of the systematically exaggerated efficacy, along with underplayed (not to mention actively hidden) risks of various pharmacotherapies unfolded, one conclusion became inescapable: massive conflicts of interest between the profession and the pharmaceutical industry had rendered psychiatry a case study in institutional corruption.
https://iipdw.org/why-i-am-not-a-psychiatrist/
Report comment
I am someone diagnosed with schizoaffective disorder and put on antipsychotics from the beggining of 2017.
I am aware I experienced what is called psychosis after a lot of stress and suffering and made some naive decisions related to money and personal choices about relationships. Maybe being medicated was the only choice at that time but it was never tried to take me away from the stressful factors, send me to a spa for example and see what happens.
It was decided I am mentally ill from an uncureable disease and that was it. First I was told I needed to be on antipsychotics for at least 6 months. After 6 months I was told I needed to stay on antipsychotics for at least 1 year. After 1 year I was told I needed to be drugged for the rest of my life.
I was recommended to a psychiatrist from a psychoanalyst I was seeing before, they worked together and since then everything I did and said was considered a symptom of the disorder. Once I said I was trying to do astral projetion, the psychoanalyst contacted the doctor and when I went to the appointment the doctor said it was necessary to increase the dosage of my antipsychotics because I was getting delusional again.
I said I wanted to learn how to program to create something like a social network like Facebook and it was considered delusions of grandeur and lithium was introduced.
Then I started to complain that I thought medicines were causing me memory loss, problems with concentrating so I couldn’t study and sexual dysfunction. The psychoanalyst would scare me and said: let’s see where you will end up without medication. And the psychiatrist said the problem was not medication and what happened was that I lost neurons because of psychosis so now I must take antipsychotics indefinitely to prevent more neurons loss. About the sexual dysfuction, she even asked me: which do you prefer, not having orgasms or going mad?
Where is the lab test about my neurons loss? Ok, I made some stupid decisions about money but why all the other people who go bankrupt are not medicated for bipolar traits? What about people who are exorcised in religious cults? Why aren’t they considered psychotic for fainting and rolling on the ground thinking they are incorporating ghosts and demons?What about transgenders and homosexuality, why is it that not so long ago it was treated with electroshock and now it simply isn’t a disorder anymore? Where is the evidence for psychiatric diagnoses?
I started to resent them for all of this and question the treatment I was receiving so I changed to another psychologist who I am seeing until now. She respects me, says I am absolutely conscious, takes seriously my concerns and believes I make sense.
I also consulted a new psychiatrist for a second opinion and again without any MRI no exams made whatsoever he said he believed what I probably had was a psychotic depression, said I was very sedated and changed the dosage of the medications I was already taking and introduced antidepressants with the warning: be careful because antidepressants might cause suicidal thoughts in the beginning, What the hell?!
I followed him and took the antidepressants for a few weeks but then I thought: if I am not depressed why on earth do I need this? Then I quit all medications about 3 months ago and I couldn’t feel better. I am back to studying, learning, reading and my sex life is getting awesome again. I feel alive and happy.
I kept seeing the first doctor with her thinking that I was taking the medication she prescribed me because I was afraid of getting institutionalized. I said: I am fine and she would reply: yes, you are fine BECAUSE of medication (the medication I was not taking). Then I asked her if it was not possible to try to take off the medicines because they were giving me side effects (when I took medicines my brother said my lips were moving involuntarily sometimes and I became afraid of developing tardive dyskinesia) and she said no, that I was on the limit of acceleration and if she took off my meds I would have very serious problems (keep in mind again I was not taking the meds).
What the hell is the limit of acceleration? She wants me as a sedated zombie?
I decided to try to stay med free, my new psychologist knows it and said it is my right unless I were a threat to myself or others and I probably wouldn’t be doing this without her support.
I don’t mean to influence anyone, I know people who feel benefited from psychiatric treatment and this is my unique story.
I hope things will keep going well.
Report comment
“Nowhere does Whitaker include references to the many studies showing structural brain abnormalities, neurological abnormalities, and neuropsychological deficits in individuals with schizophrenia who had never been treated with any medication.
Read more at: https://mentalillnesspolicy.org/myths/mad-in-america.html”
He also includes statements that are patently erroneous. For example, he claims that “even moderately high doses of haloperidol were linked to violent behavior,” when, in fact, studies have shown that haloperidol and other antipsychotics decrease violent behavior in individuals with schizophrenia. Many of Whitaker’s errors originate in his liberal footnoting of Dr. Peter Breggin, who has acknowledged having received support from Scientology, as a source.
Read more at: https://mentalillnesspolicy.org/myths/mad-in-america.html
Report comment